Approach to Tachypnea in the ED Setting
- Dec 1st, 2016
- Dorian Alexander
- categories:
Author: Dorian Alexander, MD (Associate Program Director, Director of Critical Care in Emergency Medicine, Brookdale University Hospital, Brooklyn, NY) // Edited by: Alex Koyfman, MD (@EMHighAK, EM Attending Physician, UTSW / Parkland Memorial Hospital) and Brit Long, MD (@long_brit)
Case 1:
A 19 year old female with a past medical history of asthma controlled with an albuterol inhaler presents to the ED with a chief complaint of shortness of breath. Her vital signs at triage include T 98.7F, BP 135/78, HR 108, RR 36, SpO2 100% RA.
She reports visiting a friend’s house with multiple cats and has not used her inhaler for the past two days. Today, she notes that she’s wheezing significantly, and it’s hard to breathe. Her initial peak flow is 150 with a known baseline of 350.
On exam, she’s well-appearing but tachypneic with diffuse wheezing on auscultation bilaterally without rales or rhonchi, 5 -7 word dyspnea, (+)s1s2 tachycardic without JVD, no LE edema, and an abdomen that’s soft and NT/ND.
The patient is placed on a series of nebulization treatments with albuterol and ipratropium, with improvement in her symptoms. Prednisone 60mg orally is administered, and the patient is observed for a period of time. After 3 rounds of nebulization, the peak flow has improved to 350, and she’s able to ambulate without distress in the ED. Repeat exam shows resolution of wheezing with clear lung fields bilaterally. She’s able to be discharged from the ED with a prescription for steroids and an inhaler.
Introduction
The presentation of shortness of breath is one of the most common chief complaints in the Emergency Department and primary care settings.1 Tachypnea is a symptom of an underlying process and is not a disease itself. Tachypnea in the ED is different from the subjective sensation of “shortness of breath.” Patients can be short of breath but not tachypneic.
It can be helpful to define a few terms to better understand tachypnea. Abnormally fast breathing can present as rapid shallow breathing (tachypnea) or rapid deep breathing (hyperpnea), while dyspnea refers to the sensation of shortness of breath.
A consensus statement from the American Thoracic Society defines dyspnea in the following way: “Dyspnea is a term used to characterize a subjective experience of breathing discomfort that is comprised of qualitatively distinct sensations that vary in intensity.”1
For the purpose of this discussion we will evaluate tachypnea as both rapid and deep breathing abnormalities noted on clinical presentation as a subset of a patient’s presenting symptoms inclusive of dyspnea.
The definition and clinical presentation of abnormally fast breathing should generate the following question in every clinician’s mind – why is the breathing abnormal? The answer lies in the pathophysiology of dyspnea.
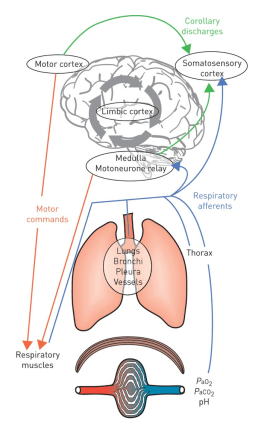
Pathophysiology of Dyspnea
Fig 12
The pathophysiology of dyspnea is related to multiple complex interactions between organ systems – the respiratory, cardiovascular, neurological systems, and oxygen carriers all play a role in the development of tachypnea and dyspnea.3 Stimulation of such receptors can be achieved by direct and indirect methods leading to multiple factors simultaneously playing a role in a patient’s clinical pathology.4
Physiologic receptors of tachypnea
Fig 25
The end point of receptor stimulation is dyspnea and tachypnea.6 Primary pulmonary receptors such as wall stretch and lower airway receptors are commonly stimulated by intra-pulmonary pathologies such as COPD/Asthma/CHF; however, chemoreceptors such as medullary and carotid body receptors are often affected by extra-pulmonary factors.3,6 The identification of extra-pulmonary factors as etiologies of dyspnea is a vital aspect of the Emergency Physician’s evaluation of acute dyspnea.
Given such complex etiologies of dyspnea and tachypnea, a systematic approach to the diagnosis and management of tachypnea will more often yield an accurate diagnosis with appropriate bedside interventions.
Pulmonary Etiologies of Tachypnea
The pulmonary system is the first organ system that is evaluated at the bedside in patients with acute dyspnea and tachypnea. Primary pulmonary pathologies can be readily identified through the use of appropriate lung physical exam techniques and radiologic imaging. History, physical exam, EKG, chest x-ray, and labs as necessary can usually yield the diagnosis in the majority of cases.
The use of point of care ultrasound (POCUS) as an adjunct to bedside evaluation of pulmonary pathology in patients with dyspnea and tachypnea should be incorporated into daily practice.
Fig 3: Asthma on chest x-ray with A-Lines on lung ultrasound 7,8
Fig 4: Pneumonia on chest x-ray with lung ultrasound findings 9,10
Fig 5: Pulmonary edema on chest x-ray with diffuse B-lines on lung ultrasound 8,11
Fig 6: Pneumothorax on chest x-ray with stratosphere sign on lung ultrasound 8,12
Case 2:
A 68 year old male with a past medical history of ESRD on hemodialysis presents to the ED with acute tachypnea. His last hemodialysis session was two days ago, and the patient completed 4 hours. Vital signs at triage include T 97.6F, BP 95/55, HR 104, RR 34, SpO2 92% RA, 98% 5L NC.
On exam, the patient appears uncomfortable with mild bibasilar crackles and is tachypneic, only able to speak in intermittent sentences, (+) s1s2 muffled, (+) JVD, (+) 1 b/l LE edema. His abdomen is soft and nontender.
Bedside lung ultrasound reveals minimal B-lines with scattered A-lines and no ultrasonographic evidence of pneumothorax. Cardiac echo reveals a pericardial effusion with bowing of the right ventricle.
The patient is placed on a cardiac monitor with 5L of supplemental oxygen via nasal cannula, and his oxygen saturation increases to 98%. Intravenous fluid with normal saline is started at 100ml/hr after an initial bolus of 500ml, and his repeat BP is 128/68. Bedside EKG shows sinus tachycardia with electrical alternans. Follow up chest x-ray shows an enlarged cardiac silhouette that is increased compared to an x-ray from one month prior.
A diagnosis of pericardial tamponade is made at the bedside, and with Cardiothoracic Surgery consultation, the patient is taken to the OR for a pericardial window.
Cardiovascular Etiologies of Tachypnea
Extra-pulmonary causes of tachypnea usually pose the biggest challenge to clinicians at the bedside. The cardiovascular system should always be considered as a potential etiology of undifferentiated tachypnea. Evaluation of heart sounds with murmurs on physical exam, presence or absence of JVD, pitting edema, and hepatomegaly can all indicate a cardiac etiology of symptoms.
Screening tools such as EKG and chest x-ray may reveal findings that lead to increased suspicion for primary cardiovascular origins of a patient’s dyspnea; however, they more often yield nonspecific information. POCUS showing pericardial effusion, tamponade physiology, diffuse B-lines, or RV > LV size may provide a higher diagnostic yield when combined with history, physical exam, EKG, and chest x-ray.13–16
Fig 7 Pericardial effusion with tamponade physiology and electrical alternans on EKG17,18
Fig 8 RV dilation and dysfunction in acute pulmonary embolus19
Hematologic Etiologies of Tachypnea
Case 3:
A 93 year old female with a past medical history of dementia is sent to the ED for increased SOB over the past two days. At baseline, the patient is non-ambulatory, non-verbal, fed via a PEG tube, and she is a full code as per her MOLST form. Her vital signs at triage are T 96.3F, BP 90/58, HR 110, RR 32, SpO2 98% RA.
On exam, the patient is a pale-appearing elderly female with notable tachypnea, clear lungs, mildly decreased breath sounds at the bases, (+) s1s2 tachycardic with a systolic ejection murmur, a soft abdomen that’s NT/ND, normal bowel sounds, a c/d/I PEG site, rectal exam (+) melena, (+) conjunctival pallor, and loss of visualization of her palmar crease.
The patient is placed on cardiac monitoring with large bore IVs and given an initial bolus of normal saline. Her repeat BP increases to 110/68, with a reduction in her HR to 84. Her EKG and CXR show NSR and bibasilar atelectasis, respectively. Her lab work is notable for a Hgb of 4 (baseline of 8 from 1 month prior) and an INR of 2.8 (the patient is on anticoagulation for DVT). The patient is transfused two units of PRBCs in the ED, started on a PPI drip, and her coagulopathy is reversed with FFP and vitamin K. The patient is adequately resuscitated with appropriate response to transfusion and admitted to the medical intensive care unit.
Hemoglobin (Hgb) acts as the major transporter of oxygen in the blood, and an acute or chronic drop in blood Hgb concentration can reduce its oxygen carrying capacity.20 In a compensatory mechanism to maintain oxygenation, neurological and carotid chemoreceptors are stimulated to maintain oxygenation by increasing minute ventilation.20 This increase in minute ventilation appears as an acute change in a patient’s baseline respiratory effort. Anemia is an often unrecognized etiology of dyspnea and tachypnea, as pending labs can delay diagnosis. However, appropriate physical exam findings can lead to earlier recognition and intervention.21
Metabolic Etiologies of Tachypnea
Case 4:
A 9 year old male with no prior medical history presents to the ED with his mother complaining of abdominal pain. As per his mother, he has been asking for a lot of water lately and going to the bathroom very often over the past 3 days. He developed one episode of vomiting today which progressed to abdominal pain. His vital signs at triage in include T 99F, BP 98/57, HR 120, RR 34, SpO2 100% RA, BGM – HIGH.
On exam, the patient is noted to be dehydrated and tired-appearing with deep, fast respirations and a questionable fruity odor on his breath, lungs clear bilaterally, (+) s1s2 tachycardic with no murmurs noted, a soft abdomen that is NT/ND, dry MM, and poor skin turgor.
The patient is immediately placed on a cardiac monitor with bilateral large bore IVs. A 20mg/kg fluid bolus is administered twice with labs drawn to evaluate for DKA including serum ketones and a venous blood gas. Initial results show a pH of 7.2, with a pCO2 of 16, and an anion gap of 22. The patient is immediately started on an insulin drip and admitted to the pediatric ICU for new onset diabetes and DKA.
Metabolic acidosis from a range of causes can lead to tachypnea. As the body attempts to compensate for worsening acidosis, the respiratory rate increases to reduce the pCO2 and maintain a compensated physiological pH.22 In many patients, this compensatory respiratory drive can be both visually impressive, as patients are generating large tidal volumes and may tire due to increased work of the respiratory muscles. The compensatory respiratory rate in metabolic acidosis is the driving force behind the tachypnea and dyspnea experienced by this subset of patients. The important clinical point to always consider is correction of the underlying etiology and not the tachypnea itself. Physiologic respiratory compensation mechanisms are very efficient in maintaining a respiratory alkalosis to compensate for a metabolic acidosis; however, a patient can tire out if the underlying cause is not treated and thus rapidly decompensate with hypercarbic respiratory failure and worsening metabolic acidosis leading to life-threatening acidemia, cardiac arrest, and death. Although the causes of metabolic acidosis are multifactorial, new onset DKA is a common ED presentation that every clinician should immediately identify based on available history, physical exam, and an easily obtainable POC blood glucose.
Management & Treatment
The multifactorial nature of tachypnea and dyspnea leads to complex management and treatment options depending on the underlying process involved. The primary goal is to always treat the primary etiology and support the respiratory system via adjunctive therapies as necessary. The detailed management of all causes of tachypnea is beyond the scope of this discussion; however, we can make some broad generalizations by organ system.
Pulmonary: Adjunctive respiratory support in the form of inhaled beta agonists and anticholinergics for bronchospasm induced disease states with additional steroids to reduce inflammation over time are the mainstay in asthma and COPD exacerbations. Diuretics work to reduce extravascular fluid in CHF states, and nitrates can assist in fluid redistribution for CHF. It’s important to note that these medications often do not provide instant relief, and patients in acute distress from bronchospastic disease or acute pulmonary edema might benefit from the initiation of non-invasive ventilation in the form of BIPAP or CPAP. Laboratory studies, although not always necessary in reversible exacerbations of asthma, might include CBC, BMP, a blood gas, troponin, and BNP. Radiologic studies in the form of chest x-ray combined with bedside lung ultrasound often confirm the diagnosis.
Cardiovascular: Cardiac causes may overlap with pulmonary etiologies: for example, an NSTEMI leading to decompensated CHF. Although workup strategies may be similar, the addition of bedside cardiac ECHO can reveal important diagnostic information. The presence of a pericardial effusion and tamponade physiology will lead to emergent changes in bedside management. RV: LV > 0.9 raises clinical suspicion for PE, and thus additional diagnostic testing such as a bilateral LE duplex and a CTA of the chest could be performed leading to earlier diagnosis and treatment.
Hematologic: Hematologic emergencies can have a broad range of management options and treatment modalities, not all of which are available in the ED. Symptomatic anemia however, is one medical emergency that should be recognized by the Emergency Physician and treated with appropriate blood product transfusion in the form of PRBCs, FFPs, and platelets as necessary.
Metabolic: Tachypnea and dyspnea from metabolic causes are a direct compensatory mechanism due to the underlying acidosis. A comprehensive differential for the evaluation of metabolic acidosis is beyond the scope of this discussion, but common etiologies such as DKA, which is managed with IVF resuscitation and initiation of insulin therapy to correct the anion gap acidosis must be recognized at the bedside for early initiation of therapy and reversal of acidosis. Other causes of metabolic acidosis, especially those related to renal failure or potentially lethal toxic overdoses, may require hemodialysis for correction.
Summary & Take Home Points
Tachypnea can be the presentation of multiple different pathologies. A focused history and physical exam, along with an understanding of the pathophysiology of appropriate disease states, can lead to thorough evaluation and management at the bedside. A systematic organ system approach to the patient can quickly lead to bedside diagnosis and initiation of treatment in patients with undifferentiated tachypnea.
As Emergency Physicians we should:
- Avoid anchoring on the pulmonary system as the only cause of tachypnea
- Maintain a broad differential for extra-pulmonary causes of tachypnea
- Use bedside ultrasound in the setting of undifferentiated tachypnea; lung US can reveal pathology of PTX, Asthma, CHF, and PNA effectively and accurately
- Utilize follow up chest x-ray to improve diagnostic ability
- Combine EKG findings with bedside ECHO to quickly identify life threatening conditions
- Remember that metabolic acidosis can present as tachypnea & point of care testing can give clues to an early diagnosis of DKA
References/Further Reading:
- Parshall MB, Schwartzstein RM, Adams L, et al. An official American thoracic society statement: Update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med. 2012;185(4):435-452. doi:10.1164/rccm.201111-2042ST.
- Laviolette L, Laveneziana P. Dyspnoea: A multidimensional and multidisciplinary approach. Eur Respir J. 2014;43(6):1750-1762. doi:10.1183/09031936.00092613.
- Ashton MD R, Raman MD D. Dyspnea. http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/pulmonary/dyspnea/. Published 2015. Accessed June 11, 2016.
- Sharma V, Fletcher SN. Review Article. N Engl J Med. 2014;333(23):1-9. doi:10.1111/anae.12709.
- Kabrhel C. Approach to the Patient with Undiffrentiated Dyspnea.; 2012.
- Burki NK, Lee LY. Mechanisms of Dyspnea. Chest. 2010;138(5):1196-1201. doi:10.1378/chest.10-0534.
- Bickle I. Hyperinflated lungs in Asthma. https://radiopaedia.org/cases/hyperinflated-lungs.
- Touw HRW, Tuinman PR, Gelissen HPMM, Lust E, Elbers PWG. Lung ultrasound: Routine practice for the next generation of internists. Neth J Med. 2015;73(3):100-107.
- Kwong Y. Pneumonia. https://radiopaedia.org/cases/klebsiella-pneumonia-1.
- Zhan C, Grundtvig N, Klug BH. Performance of Bedside Lung Ultrasound by a Pediatric Resident A Useful Diagnostic Tool in Children With Suspected Pneumonia. Pediatr Emerg Care. 2016;0(0):1-5.
- Dixon A. CHF. https://radiopaedia.org/cases/pulmonary-oedema-5.
- Jaff M. Pneumothorax. https://radiopaedia.org/cases/pneumothorax-14.
- Lichtenstein DA. BLUE-Protocol and FALLS-Protocol. Chest. 2015;147(6):1659-1670. doi:10.1378/chest.14-1313.
- Ultrasonography P, Moore CL, Copel JA. Point-of-Care Ultrasonography. N Engl J Med. 2011;364(8):749-757. doi:10.1056/NEJMra0909487.
- Koenig S, Chandra S, Alaverdian A, Dibello C, Mayo PH, Narasimhan M. Ultrasound assessment of pulmonary embolism in patients receiving CT pulmonary angiography. Chest. 2014;145(4):818-823. doi:10.1378/chest.13-0797.
- Bataille B, Riu B, Ferre F, et al. Integrated use of bedside lung ultrasound and echocardiography in acute respiratory failure: a prospective observational study in ICU. Chest. 2014;146(6):1586-1593. doi:10.1378/chest.14-0681.
- Maung M. Khin Hou R, I. Martin A, A. Bassily E, Coffman GJ, A. Siddique M, M. Whitaker D. Redistribution of pericardial effusion during respiration simulating the echocardiographic features of cardiac tamponade. Int J Case Reports Images. 2016;7(4):261. doi:10.5348/ijcri-201645-CR-10633.
- Roediger J. Electrical Alternans. http://ecgguru.com/ecg/electrical-alternans. Published 2012.
- Presently E, Tte E, States U. Role of Echocardiography in Patients with Acute Pulmonary Thromboembolism. Journal of Cardiovascular Ultrasound. 2008;16(1):9-16.
- Ferrari M, Manea L, Anton K, et al. Anemia and hemoglobin serum levels are associated with exercise capacity and quality of life in chronic obstructive pulmonary disease. BMC Pulm Med. 2015;15:58. doi:10.1186/s12890-015-0050-y.
- Santra G. Usefulness of examination of palmar creases for assessing severity of anemia in Indian perspective: A study from a tertiary care center. Int J Med Public Heal. 2015;5(2):169. doi:10.4103/2230-8598.153830.
- Ingelfinger JR, Seifter JL. Disorders of Fluids and Electrolytes Integration of Acid–Base and Electrolyte Disorders. N Engl J Med. 2014;19371(6):1821-1831. doi:10.1056/NEJMra1215672.










2 thoughts on “Approach to Tachypnea in the ED Setting”