Controversies of Thrombolytics for Pulmonary Embolism
- May 28th, 2016
- Brit Long
- categories:
Author: Brit Long, MD (@long_brit, EM Chief Resident at SAUSHEC, USAF) // Edited by: Jamie Santistevan, MD (@Jamie_Rae_EMdoc, EM Resident, University of Wisconsin) and Alex Koyfman, MD (@EMHighAK, EM Attending Physician, UTSW / Parkland Memorial Hospital)
Pulmonary embolism (PE) is a disease with significant morbidity and mortality, with an annual incidence of 100,000 cases in the U.S. which increases with age, from 1 per 1500 in early life to 1 in 300 per year above age 80 years.1,2 As providers know, the clinical presentation varies, with up to 25% of patients experiencing sudden death, while other patients with large thrombus burden experiencing few symptoms.3
The American Heart Association (AHA) and European Society of Cardiology (ESC) classify acute pulmonary embolism into three different categories: non-massive, submassive, and massive. Acute management and treatment is based on the patient, vital signs, and signs of clinical shock/instability. 4,5 Mortality for PE can reach 17% in the first three months,6 but rates of mortality in massive PE reach 30-50%.7,8 Increased mortality is seen in patients older than 70 years and those with congestive heart failure, chronic obstructive pulmonary disease, cancer, presence of one lung, hypotension, tachypnea, hypoxia, altered mental status, renal failure, prior cerebrovascular accident (CVA), right ventricular (RV) dysfunction, and elevated cardiac biomarkers.9-17
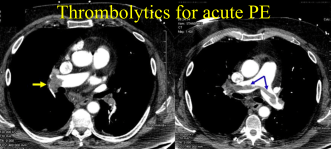
The benefits of thrombolysis is established for massive pulmonary embolism,18 but the use of thrombolytics for submassive PE is controversial in the literature due to different definitions of submassive PE, different outcomes and definitions of benefit, and the risk of life threatening hemorrhage. Thrombolytic use may reduce intravascular thrombus size and pulmonary resistance; however, there is risk of major bleeding, including intracerebral hemorrhage (ICH). Thus, the conundrum for physicians and patients.
Definitions of PE: Massive and Submassive
The definitions for massive PE, submassive PE, and nonmassive PE are shown in Table 1. 5,19 Unfortunately, many guidelines classify acute PE using different nomenclature including non-massive or low-risk, submassive or moderate/intermediate-risk, and massive or high-risk. We will use non-massive, submassive, and massive for classification of PE in this post.
Table 1 – PE Definitions and Criteria4,5,19,23
| Type of PE | Definition |
| Massive | Pulselessness, persistent bradycardia with rate less than 40 bpm, and signs of shock or sustained hypotension.
– Sustained hypotension includes SBP <90 mm Hg for >15 minutes, SBP of <100 mm Hg in a patient with a history of hypertension, or a >40% reduction in baseline SBP. Decrease in blood pressure must not be due to arrhythmia, hypovolemia, sepsis, or left ventricular (LV) dysfunction.
|
| Submassive | Normal or near-normal systolic blood pressure (SBP > 90 mm Hg) with evidence of cardiopulmonary stress including RV dysfunction or myocardial necrosis.
– Defined by RV dilatation on echo (RV diameter divided by LV diameter greater than 0.9), RV systolic dysfunction on echo, BNP > 90 pg/mL, N-terminal pro-BNP >500 pg/mL, or ECG changes (new right bundle-branch block, anteroseptal ST elevation or depression, or anteroseptal T-wave inversion). – Myocardial necrosis is defined by elevation in troponin I or T over laboratory normal value or above the patient’s baseline. |
| Nonmassive | No signs of clinical instability, hemodynamic compromise, or RV strain (US or biomarkers). |
Submassive PE accounts for approximately 20% of all PE. Though mortality is 5%, morbidity can be severe, with increased risk of pulmonary hypertension, impaired quality of life, persistent RV dysfunction, and recurrent thrombus formation.17-19
Current Guidelines
There are several guidelines for thrombolytic use in PE from the American Heart Association (AHA), The American College of Chest Physicians (ACCP), European Heart Association (EHA), and The American College of Emergency Physicians (ACEP), which are summarized in Table 2.4,5,19,23
Table 2 – Thrombolytic use in submassive and massive PE4,5,19,23
| Guideline | Submassive PE | Massive PE |
| American Heart Association (AHA) | Fibrinolysis may be considered for patients with submassive acute PE judged to have clinical evidence of adverse prognosis (new hemodynamic instability, worsening respiratory insufficiency, severe RV dysfunction, or major myocardial necrosis) and low risk of bleeding complications (Class IIb; Level of Evidence C). | Fibrinolysis is reasonable for patients with massive acute PE and acceptable risk of bleeding complications (Class IIa; Level of Evidence B). |
| The American College of Chest Physicians (ACCP) | In the majority of patients with acute PE and no hypotension, no thrombolytics should be given (Grade 1B).
|
In patients with acute PE, SBP < 90mmHg, and low to moderate risk of bleeding, thrombolytic therapy is recommended (Grade 2B).
Thrombolytic therapy is recommended for patients with acute PE who decompensate after starting anticoagulation and have low bleeding risk (Grade 2C).
|
| European Heart Association (EHA) | Routine use of thrombolysis in non-high-risk patients is not recommended, but may be considered in selected patients with intermediate-risk PE and after thorough consideration of conditions increasing the risk of bleeding. | Thrombolytic therapy is the first-line treatment in patients with high-risk PE presenting with cardiogenic shock and/or persistent arterial hypotension, with very few absolute contraindications. |
| The American College of Emergency Physicians (ACEP) | At this time, there is insufficient evidence to make any recommendations regarding use of thrombolytics in any subgroup of hemodynamically stable patients. Thrombolytics have been demonstrated to result in faster improvements in right ventricular function and pulmonary perfusion, but these benefits have not translated to improvements in mortality.
|
Administer thrombolytic therapy in hemodynamically unstable patients with confirmed PE for whom the benefits of treatment outweigh the risks of life-threatening bleeding complications.* (Level B)
Consider thrombolytic therapy in hemodynamically unstable patients with a high clinical suspicion for PE for whom the diagnosis of PE cannot be confirmed in a timely manner. (Level C) *In centers with the capability for surgical or mechanical thrombectomy, procedural intervention may be used as an alternative therapy. |
Treatments
Thrombolytics include alteplase, tenecteplase, and streptokinase. Before providing a thrombolytic medication, review the contradictions and discontinue heparin. Contraindications include prior intracranial hemorrhage (ICH), known structural intracranial cerebrovascular disease, suspected aortic dissection, known malignant intracranial neoplasm, ischemic stroke within three months, recent surgery encroaching on the brain or spinal cord, and recent closed-head or facial trauma with fracture or intracerebral injury.
Alteplase can be given as a full bolus at 10mg IV, followed by 90mg IV over 2 hours for patients greater than 65kg. For patients less than 65kg, adjust dosing so the medication does not exceed 1.5mg/kg. Half dose treatment can also be used, with alteplase given at 50mg IV bolus. Tenecteplase is dosed as a bolus, but it is not FDA approved for PE. Dosing for tenecteplase is weight-adjusted, with an IV bolus of 30-50mg over 5 seconds with a 5mg increase every 10kg from 60kg to 90kg.4,5
PE and Cardiac Arrest – Thrombolytics
Patients with cardiac arrest provide an opportunity for bedside ultrasound (US) if suspecting PE. Evaluation of RV size and function is vital in these circumstances. If findings on US are consistent with PE such as RV dysfunction and/or enlargement, consideration should be given for systemic thrombolysis, catheter-directed thrombolysis, or surgical embolectomy. Cardiothoracic surgery should be consulted.4,5,28,29
Massive PE – Thrombolytics
Thrombolysis is recommended for massive PE, as well as for patients undergoing cardiopulmonary resuscitation with US evidence of massive PE. Most guidelines state thrombolysis in patients with hemodynamic instability and massive PE is acceptable.4,5,19,23 A meta-analysis including 154 patients with massive PE found thrombolysis decreased the risk of death and recurrent PE from 19% to 9.4%, with an odds ratio of 0.45 (95% CI 0.22 to 0.9).5 For massive PE, the NNT to prevent recurrent PE or death with thrombolysis was found to be 10. The number needed to harm (NNH) was 8, however.31 A separate study by Thabut et al. estimated the number needed to harm to be 17.32
Submassive PE – Thrombolytics
Several recent studies and meta-analyses have evaluated the use of thrombolytics in submassive PE. Of note, these studies vary in their outcomes and definitions for PE.31,32 The MAPPET-3 trial in 2002 was a double blinded, randomized clinical trial including 256 patients with PE and pulmonary hypertension or RV dysfunction, but otherwise stable. Patients were given heparin with 100mg of alteplase or heparin and placebo, with a primary end point of in-hospital death or clinical deterioration. No difference was found for mortality, but for patients treated with heparin alone, more cases of deterioration were found (24.6% compared to 10.2%, P=0.004). No change in bleeding was found between groups.33
The MOPPET trial in 2013 was a single center, unblinded randomized trial with 121 patients with PE, but this study differs in that it used half dose thrombolytics. This study is arguably the best supporter of thrombolytic use in PE. These patients had RV dysfunction, and these patients demonstrated greater rates of tachypnea, hypoxia, and tachycardia, potential signs of clinical decompensation. The moderate-risk PE patients were defined as > 70% thrombus in the lobar or main pulmonary arteries (by computed tomographic pulmonary angiography), rather than using biomarkers or RV dysfunction. The investigators used moderate-risk PE, instead of submassive PE. However, these patients had smaller incidence of RV enlargement (21%) and RV dysfunction (6%). The interventional group received thrombolytics at half dose, or 50mg alteplase, rather than full dose. The investigators used an anatomical definition of submassive PE based on the extent of thrombus. The primary outcome of pulmonary hypertension, as defined by echocardiography at 28 months, was decreased in the thrombolytic group (16% of patients vs. 57%, P < 0.001, NNT 2). No bleeding was found in either group, which brings in to question the quality of data collection. Unfortunately no functional outcome was assessed, and no short-term outcomes were evaluated. This 41% difference in the primary endpoint is suspicious due to use of surrogate outcomes, rather than direct patient outcome. The investigators did not use symptoms plus echocardiographic findings, but echocardiographic findings alone. Evaluating pulmonary hypertension may reflect quality of life and exercise tolerance, but this is not for certain.34
The PEITHO trial is the largest double-blinded multicenter randomized control trial to date on submassive PE with 1006 patients which included patients with confirmed PE, abnormal RV on echocardiography or CT, and a positive troponin. Patients were randomized to heparin and placebo versus heparin plus weight-based tenecteplase bolus. The primary endpoint included death or hemodynamic collapse after 7 days, which was reduced in the thrombolytic group (2.6% vs. 5.6%, OR 0.44, 95% CI 0.23-0.87, P=0.02), but with an overall difference in hemorrhage of 9% between the groups. Those given thrombolytics also displayed 2% greater incidence of ICH. Major bleeding risk was greatly increased in patients over 75 years.35
The TOPCOAT trial evaluated 83 patients with submassive PE randomized to tenecteplase with heparin or placebo with heparin. A short-term endpoint of death, need for intubation, or surgical thrombectomy was evaluated at 5 days, and the patients returned at 6 weeks for repeat echocardiogram and 6 minute walk test. Patient perception of wellness was measured. Thrombolytic use was associated with higher probability of favorable composite outcome. At three months, composite outcomes of recurrent PE or poor functional capacity of SF 36 score were assessed. Unfortunately, the only independent variable in the study statistically significant was self-assessment of health at 90 days using SF-36 (a survey used for a variety of disease endpoints).36
Several meta-analyses have evaluated thrombolytic use in submassive PE. These meta-analyses have included the prior mentioned studies. Chatterjee in JAMA evaluated mortality benefits and bleeding risks in hemodynamically stable patients with RV dysfunction receiving thrombolysis. The analysis evaluated 2115 patients, finding a number need to harm (NNH) of 18 for major bleeding, which was not significant for patients less than 65 years, with a number needed to treat (NNT) of 59 for all-cause mortality benefit. The absolute risk reduction for mortality was 1.12%. The included studies have significant heterogeneity with varying definitions of instability, bleeding, RV dysfunction, and medication dosing.37 Nakamura et al. conducted a meta-analysis of 6 studies with 1510 patients, finding a larger absolute risk difference for death of 1.6% (not significant).38 The Cochrane database conducted a systematic review of 18 studies with 2197 patients, but the researchers state the low quality of evidence, large heterogeneity, and significant bias limits providers. Thrombolytics were associated with reduced odds of death (OR 0.57 with 95% CI 0.29-0.89), and higher rates of major and minor bleeding (OR 2.90 with 95% CI 1.95-4.31).39
A fourth meta-analysis found a significant mortality difference for patients given thrombolytics, which disappeared when the massive PE patients were removed from analysis. A significant increase in rates of major bleeding was found in the thrombolytic group.40 One meta-analysis evaluated thrombolytics versus anticoagulation in 1247 patients with submassive PE. This study found a significant reduction in recurrent PE or death (OR 0.37, 95% CI 0.21-0.66), with a significant increase in non-major bleeding (OR 4.12, 95% CI 2.37-7.17). However, major bleeding was not increased.41 All of these meta-analyses include studies with significant heterogeneity and differing definitions of submassive PE.
Catheter-Directed Treatment
Catheter-directed thrombolysis utilizes a catheter to direct thrombolytics with ultrasound assistance. A 2014 industry-sponsored study evaluated 59 patients with acute PE and RV enlargement based on echocardiogram, with patients randomized to ultrasound-directed thrombolytic with unfractionated heparin and heparin alone. RV dilatation at 24 hours was improved in the catheter-directed thrombolytic group. No bleeding complications were found in the intervention group. 28 The SEATTLE II trial was a multicenter, single-arm trial which evaluated US-facilitated, catheter-directed, low-dose thrombolysis. Investigators included 31 patients with massive PE and 119 patients with submassive PE. Treatment decreased RV dilatation, reduced pulmonary hypertension, decreased clot burden, and minimized risk of ICH. One patient suffered major bleeding with a groin hematoma and transient hypotension. 29
What should the emergency physician do?
For the patient with massive PE, the AHA, ACCP, EHA, and ACEP recommend thrombolytics.4,5,19,23 Literature supports thrombolytic use in the patient with submassive PE to reduce long-term pulmonary hypertension, but increased bleeding risk is present.
TOPCOAT and MOPPET demonstrate a benefit in long-term outcomes when using thrombolytics in patients with submassive PE. The question is whether the benefits provided to the patient outweigh the risk of major bleeding, specifically ICH at 2%. Studies have utilized different primary outcomes, so how patients may truly benefit is uncertain, except for long-term pulmonary hypertension.34,36 Patients with no prior lung disease and ample pulmonary reserve may show little benefit with thrombolytics, while the patient with conditions such as heart failure or obstructive lung disease may have greater benefit but at the same time increased risk for bleeding with thrombolytics, as demonstrated in the PEITHO trial.35 The trials also utilize differing protocols and doses. The risk of utilizing thrombolytics is major bleeding, particularly ICH. PEITHO demonstrated a bleeding rate of 11.5% with full dose tenecteplase, compared to 2.4% in the heparin alone group. However, this trial utilized heparin drips targeting aPTT levels of 2-2.5 times the upper limit of normal with full dose thrombolytics.35 The JAMA meta-analysis found a NNH of 18 for major bleeding (increased risk in those over 65).37 No increased risk of bleeding was present in patients less than 65 years.33-41
Shared Decision-Making
In submassive PE, the benefits and risks of bleeding should be discussed in a shared decision-making model with the patient, family, and admitting team, with thrombolytics considered on a case-by-case basis. The AHA, EHA, and ACCP support thrombolytics in patients with submassive PE and low bleeding risk.4,5,19
1) Patient factors including comorbidities, age, medications, and independence/functional ability must be taken into account. Patients over 65 years of age or with significant comorbidities have significant increased bleeding risk compared to younger patients.
2) The absence of contraindications must be ensured.
3) The entire picture including clinical course, ultrasound, biomarkers (troponin and BNP), and CT results should be considered.
4) Clinical decompensation including hypoxia, worsening tachypnea or tachycardia, and even brief episodes of hypotension requires consideration of thrombolysis.
If the patient is a thrombolytic candidate with bleeding risk, using half dose thrombolytics while discontinuing anticoagulation can demonstrate improved long-term functional outcomes, with lower risk of bleeding. If thrombolytics at a one-time half dose is not sufficient, a second similar dose can be provided while observing the patient for clinical improvement or decline. Starting anticoagulation after a period of observation for bleeding and decompensation may reduce bleeding.42
Catheter-directed treatments provide a separate avenue for management. With an extremely low risk of major bleeding, these agents are optimal first line treatment options, especially in patients with increased risk of bleeding (such as patients over 65 years of age), patients with clinical decompensation, and in patients who fail to improve with initial thrombolytics.28,29,43
Summary
– Submassive PE presents a challenge for physicians. Current literature including meta-analyses have inconsistent definitions of submassive PE, lack functional outcomes, have differing primary outcomes and assessments, and use different treatment protocols with thrombolytics and anticoagulation agents.
– Support exists for improvement in long-term outcomes with thrombolytics, with increased risk of major bleeding in high-risk patients.
– The risks and benefits of thrombolytic treatment should be considered on a case-by-case basis.
– Shared decision-making with the patient discussing the risks and benefits of treatment is recommended.
– Further studies that assess risk stratification, functional outcomes, and treatment protocols with thrombolytic dosing are needed.
References/Further Reading:
- Cushman M, Tsai AW, White RH, Heckbert SR, Rosamond WD, Enright P, et al. Deep vein thrombosis and pulmonary embolism in two cohorts: the longitudinal investigation of thromboembolism etiology. Am J Med 2004 Jul;117(1):19-25.
- Heit JA. The epidemiology of venous thromboembolism in the community: implications for prevention and management. J Thromb Haemost 2006 Feb;21(1):23-29.
- Lucena J, Rico A, Vázquez R, Marín R, Martínez C, Salguero M, Miguel L. Pulmonary embolism and sudden-unexpected death: prospective study on 2477 forensic autopsies performed at the Institute of Legal Medicine in Seville. J Forensic Leg Med 2009 May;16(4):196-201.
- Torbicki A, Perrier A, Konstantinides S, Agnelli G, Galie N, Pruszczyk P, Bengel F, Brady AJ, Ferreira D, Janssens U, Klepetko W, Mayer E, Remy-Jardin M, Bassand JP. Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). Eur Heart J 2008;29:2276-2315.
- Jaff MR, McMurtry MS, Archer SL, Cushman M, Goldenberg N, Goldhaber SZ, Jenkins JS, Kline JA, Michaels AD, Thistlethwaite P, Vedantham S, White RJ, Zierler BK. Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association. Circulation 2011;123:1788-1830.
- Brembilla-Perrot B, Miljoen H, Houriez P, Beurrier D, Nippert M, Vançon AC, de la Chaise AT, Louis P, Mock L, Sadoul N, Andronache M. Causes and prognosis of cardiac arrest in a population admitted to a general hospital; a diagnostic and therapeutic problem. Resuscitation 2003;58:319-327.
- Torbicki A, Gali N, Covezzoli A, et al. Right heart thrombi in pulmonary embolism. Results from the International Cooperative Pulmonary Embolism Registry. J Am Coll Cardiol 2003;41:2245- 2251.
- Dalen JE, Alpert JS. Natural history of pulmonary embolism. Prog Cardiovasc Dis 1975;17(4):259.
- Goldhaber SZ, Visani L, De Rosa M. Acute pulmonary embolism: clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER). Lancet 1999;353:1386-1389.
- Konstantinides S, Geibel A, Olschewski M, et al. Association between thrombolytic treatment and the prognosis of hemodynamically stable patients with major pulmonary embolism. Results of a multicenter registry. Circulation 1997;96:882-888.
- Becattini C, Vedovati MC, Agnelli G. Prognostic value of troponins in acute pulmonary embolism. A meta-analysis. Circulation 2007;116:427-433.
- Kucher N, Wallmann D, Carone A, et al. Incremental prognostic value of troponin I and echocardiography in patients with acute pulmonary embolism. Eur Heart J 2003;24:1651-1656.
- Aujesky D, Obrosky S, Stone RA, et al. A prediction rule to identify low-risk patients with pulmonary embolism. Arch Intern Med 2006;166:169-175.
- Jimenez D, Uresandi F, Otero R, et al. Troponin-based risk stratification of patients with acute nonmassive pulmonary embolism. Systematic review and metaanalysis. Chest 2009;136:974-982.
- Kreit JW. The impact of right ventricular dysfunction on the prognosis and therapy of normotensive patients with pulmonary embolism. Chest 2004;125:1539-1545.
- Klok FA, Mos IC, Huisman MV. Brain-type natriuretic peptide levels in the prediction of adverse outcome in patients with pulmonary embolism. A systematic review and meta-analysis. Am J Respir Crit Care Med 2008;178:425-430.
- Stein PD, Matta F, Janjua M, et al. Outcome in stable patients with acute pulmonary embolism who had right ventricular enlargement and/or elevated levels of troponin I. Am J Cardiol 2010;106:558-563.
- Bailén MR, Cuadra JA, Aguayo De Hoyos E. Thrombolysis during cardiopulmonary resuscitation in fulminant pulmonary embolism: a review. Crit Care Med 2001;29:2211-2219.
- Kearon C, Akl EA, Ornelas J, Blaivas A, Jimenez D, Bournameaux H, et al. Antithrombotic Therapy for VTE Disease: CHEST Guideline and Expert Panel Report. Chest 2016;149(2):315-352.
- Kuo WT, Gould MK, Louie JD, Rosenberg JK, Sze DY, Hofmann LV. Catheter-directed therapy for the treatment of massive pulmonary embolism: systematic review and meta-analysis of modern techniques. J Vasc Interv Radiol 2009;20(11):1431-1440.
- Engelberger RP, Kucher N. Catheter-based reperfusion treatment of pulmonary embolism. Circulation 2011;124(19):2139-2144.
- Kucher N, Boekstegers P, Müller OJ, Kupatt C, Beyer-Westendorf J, Heitzer T, Tebbe U, Horstkotte J, Müller R, Blessing E, Greif M, Lange P, Hoffmann RT, Werth S, Barmeyer A, Härtel D, Grünwald H, Empen K, Baumgartner I. Randomized, controlled trial of ultrasound-assisted catheter-directed thrombolysis for acute intermediate-risk pulmonary embolism. Circulation 2014;129(4):479-486.
- Fesmire FM, Brown MD, Espinosa JA, Shih RD, Slivers SM, Wolf SJ, Decker WW. Critical issues in the evaluation and management of adult patients presenting to the emergency department with suspected pulmonary embolism. Ann Emerg Med 2011;57:628-652.
- Rudd KM, Phillips EL. New oral anticoagulants in the treatment of pulmonary embolism: efficacy, bleeding risk, and monitoring. Thrombosis 2013;2013:973710.
- Becattini C, Vedovati MC, Agnelli G. Old and new oral anticoagulants for venous thromboembolism and atrial fibrillation: a review of the literature. Thromb Res 2012 Mar;129(3):392-400.
- Lanitis T, Hamilton M, Quon P, Browne C, Masseria C, Cohen AT. Cost-Effectiveness of Apixaban Compared to Low Molecular Weight Heparin/ Edoxaban for Treatment and Prevention of Recurrent Venous Thromboembolism. Value Health 2015 Nov;18(7):A375-6.
- Hernandez C, Shuler K, Hannan H, Sonyika C, Likourezos A, Marshall J. CAUSE: cardiac arrest ultra-sound exam—a better approach to managing patients in primary non-arrhythmogenic cardiac arrest. Resuscitation 2008 Feb;76(2):198-206.
- Borloz MP, Frohna WJ, Phillips CA, Antonis MS. “Emergency department focused bedside echocardiography in massive pulmonary embolism.” J Emerg Med 2011 Dec;41(6):658-660.
- Piazza G, Hohlfelder B, Jaff MR, et al. A Prospective, Single-Arm, Multicenter Trial of Ultrasound-Facilitated, Catheter-Directed, Low-Dose Fibrinolysis for Acute Massive and Submassive Pulmonary Embolism. The SEATTLE II Study. J Am Coll Cardiol Intv 2015;8:1382.
- Stein PD, Alnas M, Beemath A, Patel NR. Outcome of pulmonary embolectomy. Am J Cardiol 2007 Feb;99(3):421-3.
- Wan S, Quinlan DJ, Agnelli G, Eikelboom JW. Thrombolysis compared with heparin for the initial treatment of pulmonary embolism: a meta-analysis of the randomized controlled trials. Circulation. 2004 Aug 10;110(6):744-9.
- Thabut G, Thabut D, Myers RP, Bernard-Chabert B, Marrash-Chahla R, Mal H, Fournier M. Thrombolytic therapy of pulmonary embolism: a meta-analysis. J Am Coll Cardiol 2002 Nov;40(9):1660–1667.
- Konstantinides S, Geibel A, Heusel G, et al. Heparin plus alteplase compared with heparin alone in patients with submassive pulmonary embolism. N Engl J Med 2002 Oct;347(15):1143-50.
- Sharifi M, Bay C, Skrocki L, Rahimi F, Mehdipour M; “MOPETT” Investigators. Moderate pulmonary embolism treated with thrombolysis (from the “MOPETT” Trial). Am J Cardiol 2013 Jan 15;111(2):273-7.
- Meyer G, et al; PEITHO Investigators. Fibrinolysis for patients with intermediate-risk pulmonary embolism. N Engl J Med 2014 Apr 10;370(15):1402-11.
- Kline JA, Nordenholz KE, Courtney DM, Kabrhel C, Jones AE, Rondina MT, Diercks DB, Klinger JR, Hernandez J. Treatment of submassive pulmonary embolism with tenecteplase or placebo: cardiopulmonary outcomes at 3 months: multicenter double-blind, placebo-controlled randomized trial. J Thromb Haemost 2014 Apr;12(4):459-68.
- Chatterjee S, Chakraborty A, Weinberg I, Kadakia M, Wilensky RL, Sardar P, Kumbhani DJ, Mukherjee D, Jaff MR, Giri J. Thrombolysis for pulmonary embolism and risk of all-cause mortality, major bleeding, and intracranial hemorrhage: a meta-analysis. JAMA 2014 Jun 18;311(23):2414-21.
- Nakamura S, Takano H, Kubota Y, Asai K, Shimizu W. Impact of the efficacy of thrombolytic therapy on the mortality of patients with acute submassive pulmonary embolism: a meta-analysis. J Thromb Haemost 2014 Jul;12(7):1086-95.
- Hao Q, Dong BR, Yue J, et al. Thrombolytic therapy for pulmonary embolism. Cochrane Database Syst Rev 2015 Sep 30;9:CD004437.
- Marti C, John G, Konstantinides S, Combescure C, Sanchez O, Lankeit M, et al. Systemic thrombolytic therapy for acute pulmonary embolism: a systematic review and meta-analysis. Eur Heart J 2015 Mar 7;36(10):605-614.
- Chen H, Ren C, Chen H. Thrombolysis versus anticoagulation for the initial treatment of moderate pulmonary embolism: a meta-analysis of randomized controlled trials. Respir Care 2014 Dec;59(12):1880-7.
- Zhang Z, Zhai ZG, Liang LR, Liu FF, Yang YH, Wang C. Lower dosage of recombinant tissue-type plasminogen activator (rt-PA) in the treatment of acute pulmonary embolism: a systematic review and meta-analysis. Thromb Res 2014 Mar;133(3):357-63.
- Stein PD, Matta F, Steinberger DS, Keyes DC. Intracerebral hemorrhage with thrombolytic therapy for acute pulmonary embolism. Am J Med 2012 Jan;125(1):50-6