ECG Pointers: Atrial Fibrillation with Aberrancy
- May 11th, 2022
- Lloyd Tannenbaum
- categories:
Authors: Lloyd Tannenbaum (EM Attending Physician, San Antonio, TX) and Brannon Inman (EM Resident, San Antonio, TX)// Reviewed by: Jamie Santistevan, MD (@jamie_rae_EMdoc, EM Physician, Presbyterian Hospital, Albuquerque, NM); Manpreet Singh, MD (@MPrizzleER); and Brit Long, MD (@long_brit)
The Case:
It’s 2 am on your first moonlighting shift since becoming a staff physician. You’re starting to feel the strain of that 24-hour shift, and with only 4 hours left, your eyes feel a little heavy. Right as you’re starting to nod off, you see the nurses come running towards you with an EKG. They look nervous, which, of course, makes you feel nervous. You take a look and see the following EKG:

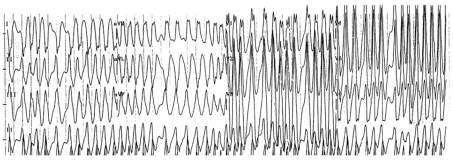
Figure 1: This EKG shows a wide-complex, irregular rhythm. It looks, to quote one of my mentors, “bad.”
You take a look at the EKG and look perplexed. It’s definitely a wide complex tachycardia, but what should you do? Should you shock? Should you go see the patient? Does the patient have a pulse? Do they have blood pressure? What is your blood pressure? Is this EKG compatible with life? Are the nurses just pranking you?
You look up and the nurses are urging you to get to the resuscitation bay. You jog over and see a pale looking man with a tele monitor beeping all kinds of alarms and a rhythm strip that looks identical to the EKG in your hand. After taking a second to get the nerves out, you think back on the approach to a patient with a tachydysrhythmia.
Approach to tachydysrhythmias:
Tachydysrhythmias can be terrifying. They often come with lots of beeping machines, anxious ancillary staff, nurses, techs, and medics. And that’s not even counting the patient, who likely feels like their heart is trying to beat out of their chest. To be fair, that is likely because their heart is, in fact, trying to beat out of their chest. The approach to tachydysrhythmias, much like most things in medicine, is not as terrifying as it seems. There are 2 big questions we want you to ask yourself when you see a tachydysrhythmia:
- Is the rhythm narrow or wide?
- Is the rhythm regular or irregular?
If you just take a second to ask yourself about these questions, you’ll be able to guide yourself to identifying the underlying rhythm, which will help you figure out how to treat the patient. You likely saw this chart in residency, but just take a minute to refresh yourself with it:

Wide-complex, irregular tachycardias:
As you can guess, we’re just going to talk about the bottom right box: the wide and irregular tachycardia. Two of the three are often easily recognizable, as they are often tested and drilled into you, Ventricular fibrillation (Vfib) and Torsades Des Pointes (TdP). Let’s refresh ourself with two examples below:
The first rhythm strip shows Vfib. Notice the low electrical amplitude and lack of identifiable organized electrical activity. In general, it is considered poor form to get an entire EKG from a patient in vfib. You should be able to recognize it from the rhythm strip and start treating immediately… with electricity!

Below shows an excellent example of TdP, a type of polymorphic VT. Recall that all TdP is polymorphic VTach, not all Polymorphic VTach is TdP. TdP is a unique polymorphic VTach morphology that occurs in the setting of prolonged QTc intervals. Notice how in TdP the amplitudes of the QRS complexes rise and fall as though they are twisting on a point. 1,2

Finally comes the interesting two… Atrial Fibrillation with aberrancy, and Atrial Fibrillation with preexcitation
Let’s start with the basics. Atrial fibrillation is likely something you’ve heard of before. Instead of the sinus node being in charge of the electrical rhythm of the heart, there are multiple foci of electrical impulses stimulating the AV node, leading to irregularly irregular beats. See this example below:
This EKG shows a patient in atrial fibrillation. Notice the lack of discernable P waves and a variable ventricular rate (irregularly irregular rhythm).

Now, we covered the atrial fibrillation, what about aberrancy? Aberrancy, or aberrant conduction just means that the beats do not get conducted along the traditional conduction pathway. Atrial fibrillation with a right bundle branch block or left bundle branch blocks are good examples of atrial fibrillation with aberrancy.
See the below EKG of atrial fibrillation with aberrancy (likely a left bundle). Notice how this is a wide complex irregular tachycardia, and with each beat the morphology of the QRS is almost exactly the same.

The other critical type of atrial fibrillation with aberrancy is atrial fibrillation with Wolf-Parkinson-White (WPW) AKA atrial fibrillation with preexcitation. In WPW, there is an accessory pathway, the Bundle of Kent, which electricity can follow to bypass the normal conduction system. For a full, in depth look at WPW see here at http://www.emdocs.net/ecg-pointers-syncope-and-wolf-parkinson-white/
Take a look at this patient’s EKG again; it looks more pre-excited than a teenage boy at prom:

Notice that in comparison to afib with a bundle branch block, this patient’s EKG is a wide-complex irregular tachycardia where there are numerous different QRS complex morphologies. This is unique from atrial fibrillation with an underlying bundle branch block (which has a single morphology of QRS complex, but is still wide and irregular) and ventricular fibrillation (which has numerous morphologies of indistinct QRS complexes, that result in no perfusion). In this EKG notice the delta waves, best seen in the V5 rhythm strip. Why is important? The presence of a delta wave clues you into preexcitation or an accessory pathway, allowing the electrical current to go both ways. If the electricity goes down the accessory pathway and up the normal conduction pathway, you’ll see an EKG like this:
How do you treat these patients?
The answer is… it depends. There are a few right answers one wrong answer.
See the below chart from the 2014 AHA clinical practice guideline for the management of patient’s with atrial fibrillation: 3

When treating atrial fibrillation with preexcitation there is really only one wrong answer, and that’s to block the AV node. Blocking the AV node will shut down the portion of the heart’s conduction pathway that possess any capacity for gatekeeping the ridiculous electrical rave that is happening in the atrium of an afib patient. Think of the AV node as a bouncer at a bar keeping out a few hundred guests (the electrical current in the atrium). Once the bouncers stop working and close the front door the crowd floods in the side entrance. Now the rave made its way into the ventricle. The result?
Remember Vfib?
![]()
Unfortunately, this is often the result of giving an AV nodal blocker to a patient with afib and preexcitation. Some might call this a clean kill.
Even more unfortunate, many of our favorite medications block the AV node. Importantly amiodarone blocks the AV node. In fact, the 2014 AHA clinical practice guideline for the management of patient’s with afib recommended against its use when treating pre-excited afib, possibly due to a slew of case reports of poor outcomes. 3
So what are our treatment options in the ER? Well, if we were to follow this CPG there are two. One would be a whiff of sedation and synchronized cardioversion. Cardioversion is safe, the half life is short, and it’s quite effective. If you want a medication, procainamide is the go-to option with a level I recommendation. Procainamide has been shown to have a predilection for increasing the refractory period of accessory pathways. 3,4
Case Conclusion:
You notice the delta waves and wide complex irregular rhythm and correctly identify that the patient is in afib with WPW. His blood pressure is 80/palp and he is very pale. He feels like he is going to pass out. You have the pads placed on the patient and synchronized cardiovert him at 100J. After that, he goes back to normal sinus rhythm. His blood pressure stabilizes. The whole room breathes a sigh of relief.
Main ECG Pointers:
- Have a systematic approach to tachydysrhythmias
- Atrial fibrillation with WPW can get unstable quickly
- Avoid AV nodal blockers in patients with WPW
- If the patient is stable, you can try procainamide
- If the patient is unstable, emergent synchronized cardioversion is indicated.
References:
- Polymorphic VT and Torsades de Pointes (TdP) • LITFL. Accessed November 12, 2021. https://litfl.com/polymorphic-vt-and-torsades-de-pointes-tdp/
- Chan A, Isbister GK, Kirkpatrick CMJ, Dufful SB. Drug-induced QT prolongation and torsades de pointes: evaluation of a QT nomogram. QJM: An International Journal of Medicine. 2007;100(10):609-615. doi:10.1093/QJMED/HCM072
- Craig T. January M, Joseph S. Alpert M, Joaquin E. Cigarroa M, et al. 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation. AHA. Accessed November 12, 2021. https://www.ahajournals.org/doi/pdf/10.1161/CIR.0000000000000041
- Leitch JW, Klein GJ, Yee R, Feldman RD, Brown J. Differential effect of intravenous procainamide on anterograde and retrograde accessory pathway refractoriness. Journal of the American College of Cardiology. 1992;19(1):118-124. doi:10.1016/0735-1097(92)90061-Q
