Elevated Troponin in the Setting of Supraventricular Tachycardia: Is it Clinically Significant?
- Jun 15th, 2016
- Erica Simon
- categories:
Author: Erica Simon, DO, MHA (EM Resident Physician, SAUSHEC) // Edited by: Alex Koyfman, MD (@EMHighAK, EM Attending Physician, UTSW / Parkland Memorial Hospital) and Stephen Alerhand, MD (@SAlerhand)
A 33 year-old male presents to your emergency department with the chief complaint of shortness of breath. As you walk into the patient’s room to greet him, you glance at his monitor which displays: HR 152, SBP 127/82, RR 22, SpO2 98% on room air. You begin your history taking, noting the absence of respiratory distress. The patient speaks in full sentences, explaining that he noticed the onset of palpitations and acute shortness of breath while watching television and smoking a cigarette one hour prior to arrival. The patient denies any past medical history. Family history is remarkable only for a maternal grandmother with DM II. Review of systems is negative for recent travel, history of DVT/PE, thyroid pathology, and lower extremity edema.
As you scroll through the triage note, you come across the patient’s EKG, demonstrating the absence of p-waves, and a narrow regular QRS complex with a ventricular rate of 154. Suspecting supraventricular tachycardia (SVT) as the etiology of the patient’s palpitations and potentially his shortness of breath, you attempt vagal maneuvers. After failed modified Valsalva technique, you administer 6 mg IV adenosine, which results in conversion to normal sinus rhythm.
While gathering your thoughts regarding the various labs and radiologic studies that you would like to order, you contemplate sending a troponin. The patient is a young male without chest pain; he has one cardiac risk factor. Is the troponin needed for risk stratification? Is the troponin likely to be elevated in the setting of SVT? Should a troponin be included in the standard evaluation of not just this patient’s SVT, but all patients presenting with SVT?
If you have pondered questions such as these, the following provides a discussion of the research on the topic, in addition to tips regarding the tailoring of your personal practice.
Troponin Levels – A Quick Pathophysiologic Review
Cardiac troponin T (cTnT), cardiac troponin I (cTnI), and cardiac troponin C (cTnC), in addition to actin and myosin, compose the myocardial sarcomere.1-5 At the molecular level, cardiac contraction is mediated by the entrance of calcium into the myocyte sarcolemma. When calcium binds to cTNC, a conformational change results, triggering the dislocation of troponin I from actin, and tropomyosin from myosin, allowing for actin and myosin interaction and subsequent contraction.6 (See the Annals of Clinical Biochemistry (reference 6) figure below for a quick review. Note: Red component = calcium.
Figure 1. Components of the Myocardial Sarcomere6
Programmed proteolytic degradation of the sarcomeric unit results in a steady-state level of cTnT (6-8%) and cTnI (2-4%); hence the normal laboratory reference values. 1,2 Myonecrosis, occurring in the setting of ischemic versus non-ischemic cardiac myocyte injury, is evidenced by elevated circulatory levels of cTnT and cTnI.1-7 As cTnT and cTnI are localized to the cardiac myocyte, elevations of these proteins are sensitive indicators of myonecrosis. 1-7
Troponin Sensitivity and Specificity
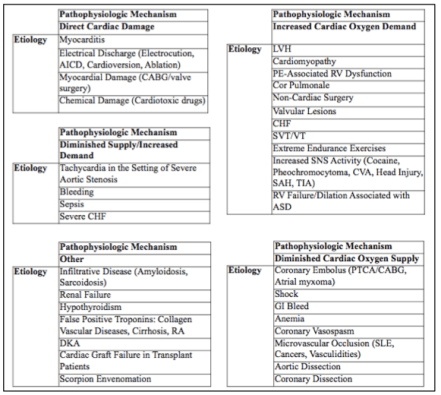
Cardiac troponin assays are utilized as the gold standard in the detection of acute cardiovascular events, however, elevated troponins are not synonymous with myocardial infarction.1-3,5,7-11 Current cardiology literature details numerous studies citing varying etiologies of, and settings in which, cardiac troponins may be elevated in the absence of coronary artery disease. The following figure includes a summary of such etiologies and is adapted from Mahajan et al.’s and Clark’s works cited below. For a complete list of references utilized by Mahajan et al. and Clark, please view these respective publications directly.
Figure 2. Etiologies of Elevated Troponin in Patients with Normal Coronary Arteries1,4
Note: Troponin elevations secondary to these pathophysiologic mechanisms are not isolated to the adult population. Case reports have identified cTnI elevation s/p SVT in children with and without underlying cardiac pathology (HOCM).12,13
Go here for further reading: http://www.emdocs.net/the-elevated-troponin-what-else-besides-acs-could-cause-troponin-elevation/
What Does the Literature Say About Elevated Troponin Levels and SVT?
The following chart is a summary of relevant literature. The articles contained within are also cited in the Best Evidence Topic (BET) Summary, published in the Emergency Medicine Journal in 2010.
(Note: In seeking to assess the appropriateness of the routine use of troponin levels in the evaluation of SVT, the authors of the BET summary performed a Medline search (dates) using the Pubmed interface [SVT] and [troponin levels] and [evaluation of CAD]. Based upon their findings, the authors concluded that there was not sufficient research to support the routine utilization of troponin levels in the evaluation of uncomplicated SVT.14)
| Author | Study Type | Subjects | Presenting Symptom(s) | CAD Risk Factor(s) | Outcomes | Findings |
| Patane et al., 20093 | Case Study | 49F with SVT. Cardiac risk factor: current smoker. | Palpitations | Current Smoker. | Elevated cTnI | Echo with mitral regurgitation and septal hypertrophy. Troponin normalized. Note: Confounding factor: History of multinodular goiter and paroxysmal SVT. Anti-TPO antibodies elevated and TSH low during hospital stay. |
| Miranda et al., 20065 | Case Study | 49F with SVT and elevated troponin. | Retrosternal pain, nausea, diaphoresis, shortness of breath, palpitations | None reported. PMHx of tachycardia with propranolol therapy. | Elevated cTnI | Coronary angiography without findings. |
| Zellweger et al., 20037 | Case Series | Four patients (ages 44-57) with SVT and elevated troponins. | 44M: Chest pain and shortness of breath 48F: Atypical chest pain 50M: Dizziness, lightheadedness, shortness of breath, nausea. 57F: Dizziness, chest pain. | 44M: None reported. PMHx of SVT. 48F: None reported. PMHx of SVT. 50M: None reported. 57F: None reported. | Elevated cTnI for all. 57F with ST depression in infero-lateral leads s/p adenosine. | Myocardial perfusion imaging (48 F, 50 M), stress echocardiography (50 M), coronary angiography (44 M, 57 F); all without findings of coronary artery disease. |
| Bakshi et al., 20028 | Prospective Cohort | Three patients (ages 37-49) presenting with SVT and elevated troponin. (Note: Study included 21 patients with elevated troponins who underwent coronary angiography for suspected CAD) | 37F: Non-anginal chest discomfort. 45 year-old male: Atypical chest pain. 49F: Typical chest pain and diaphoresis. | All: No PMHx reported. | Elevated cTnI. EKG of 49F with ST depressions. | Two patients with EKG changes suspicious for ACS: coronary angiography unremarkable. One patient with normal EKG with unremarkable coronary angiography. |
| Redfearn et al., 200510 | Retrospective Cohort | Three patients (ages 22-72) with SVT and elevated troponin. | 22M, 56M, 72M: no presenting symptoms reported. | All: No PMHx reported. | Elevated cTnI | All patients with unremarkable coronary angiography. |
| Yeo et al., 200611 | Case Series | Three patients (ages 22-58) with SVT and elevated troponins. | 22M: Palpitations and dyspnea.
45M: Asymptomatic. 58M: Asymptomatic. |
22M: No CAD risk factors.
45M: No CAD risk factors but PMHx of non-ischemic cardiomyopathy, VT and COPD. 58M: HTN. PMHx also significant for CKD. |
All patient with elevated cTnI. 45 year-old male EKG: VT. 58 year-old male EKG: RBB, VT. | All patients with unremarkable coronary angiography. |
-Legend: M = Male, F = Female, PMHx = Previous Medical History
-Note: Unless otherwise indicated, all patient EKGs consistent with narrow complex tachycardia (SVT).
-Cardiac risk factors: DM, Smoking, HTN, HLD, Family Hx of CAD <55 years of age.
Is there Prognostic Significance of cTnI Levels in Hospitalized Patients Presenting with SVT?
To date, only one study published out of Johns Hopkins has collected data on this topic. Chow et al. retrospectively screened patient records given an ICD-9 discharge diagnosis of SVT from 2002-2006. Patients included in the study were those who had been evaluated and treated in the emergency department, possessed an EKG demonstrating SVT, had at least one cTnI level and creatinine recorded, and received follow-up within one year of discharge. Patients excluded included those who ultimately received a diagnosis of atrial fibrillation or flutter, those who presented with a severe concurrent illness, and those who died within 30 days of discharge due to unrelated causes.
In total, 78 patients met criteria for the study (54% female; mean age 62.2 ±15.8 yrs) and 29 patients had an elevated cTnI. Univariate predictors of elevated cTnI included: LVEF <50%, renal dysfunction, ST segment depression, LBBB on EKG, and mod/severe valvular regurgitation.
Multivariable adjustment identified the presence of elevated cTnI with SVT as being associated with increased risk of death, MI, or cardiovascular re-admission (hazard ratio: 3.67; 95% CI 1.22-11.1; p = 0.02).15
Note: Hospitalized individuals with an elevated troponin more commonly possessed medical co-morbidities as compared to their counterparts presenting without elevated troponins. Please see the reference below if interested in further reading/evaluation.15
What Can We Conclude?
- Cardiac troponins are sensitive in terms of locale – they are found only in the myocardium. Troponin elevation is NOT specific for myocardial infarction or coronary artery pathology. Cardiology literature has identified numerous etiologies of troponin elevation in the absence of coronary angiographic findings. Case reports in the pediatric population have also demonstrated the same.
- Current research regarding the utilization of troponin levels in the evaluation and management of SVT is limited to small cohort studies (low n), case series, and case reports. One Best Evidence Topic Summary published in the Emergency Medicine Journal in 2010 recommends against the routine use of troponin levels in the setting of uncomplicated SVT (a presentation undefined in the BET summary), due to the potential for unnecessary testing and treatments.14
- A study out of Johns Hopkins has demonstrated an increased risk of death, MI, and CV re-admission in patients requiring hospitalization following an ED presentation of SVT with elevated troponin (these individuals were more likely to have numerous medical co-morbidities [CAD, DM, COPD, CrCl <60ml/min, etc.]).15
Bottom Line
Given this review and the aforementioned findings, it is reasonable to infer that the decision to send a troponin should be based on a thorough H&P – if the history is concerning, anginal equivalents are present, there are cardiac risk factors, major medical comorbidities exist, or there are findings on physical exam concerning for cardiac pathology (new murmurs, signs/symptoms of new onset CHF, etc.), a troponin should be sent.
Is troponin elevation in the setting of SVT significant? In the appropriate clinical setting, yes, it can be.
References / Further Reading
- Mahajan N, Mehta Y, Rose M, Shani J, and Lichstein E. Elevated troponin level is not synonymous with myocardial infarction. Int J Cardiol 2006; 111: 442-449.
- Hein S, Scheffold T, Schaper J. Ischemia induces early changes to cytoskeletal and contractile proteins in diseased human myocardium. J Thorac Cardiovasc Surg 1995; 110: 89-98.
- Patane S, Marte F, Di Bella G. Abnormal troponin I levels after supraventricular tachycardia. Int J Cardiol 2009; 132: e57-e59.
- Clark M. Elevated cardiac troponins: Their significance in acute coronary syndrome and noncardiac conditions. J Okla State Med Assoc 2006; 99(6): 363-367.
- Miranda R, Machado M, Takakura I, da Mata P, da Fonseca C, Mouco O, et al. Elevated troponin levels after prolonged supraventricular tachycardia in patients with normal coronary angiography. Cardiology 2006; 106: 10-13.
- Gaze D, Colinson P. Multiple molecular forms of circulating cardiac troponin: Analytical and clinical significance. Ann Clin Biochem 2008; 45(Pt 4): 349-55
- Zellweger M, Schaer B, Cron T, Pfisterer M, Osswald S. Elevated troponin levels in the absence of coronary artery disease after supraventricular tachycardia. Swiss Med Wkly 2003; 133: 439-441.
- Bakshi T, Choo M, Edwards C, Scott G, Hart H, Armstrong P. Causes of elevated troponin I with a normal coronary angiogram. Int Med J 2002; 32:520-525.
- Costabel J, Urdapilleta M, Lambardi F, Campos R, Vergara J, et al. High-sensitivity cardiac troponin levels in supraventricular tachyarrhythmias. Pacing Clin Electrophysiol 2016. doi: 10.1111/pace.12851. [Epub ahead of print]
- Redfearn D, Ratib K, Marshal H, et al. Supravantricular tachycardia promotes release of troponin I in patients with normal coronary arteries. Int J Cadiol 2005; 102:521-22.
- Yeo K, Cruz L, Hong R. Tachycardia-induced elevations in cardiac troponin in the absence of coronary artery disease. Hawaii Med J 2006; 65:86-87.Luna C, Adie M, Tessle I, Acherman R.
- Luna C, Adie M, Tessler I, Acherman R. Troponin I elevation after supraventricular tachycardia in a child with hypertrophic cardiomyopathy. Pediatr Cardiol 2001; 22:147-149.
- Moore J, Arcilla L, Wang S, Lee M, Shannon K. Characterization of cardiac troponin elevation in the setting of pediatric supraventricular tachycardia. Pediatr Cardiol 2016; 37: 392-398.
- Carley S. Towards evidence based emergency medicine: best BETs from the Manchester Royal Infirmary. Emerg Med J 2010; 27(2): 141-142.
- Chow G, Hirsch G, Spragg D, Cai J, Cheng A, et al. Prognostic significance of cardiac troponin I levels in hospitalized patients presenting with supraventricular tachycardia. Medicine 2010; 89(3):141-147.


great work! congratulations, really usefull… greetins from Colombia