emDOCs Podcast – Episode 43: Oncologic Emergencies Part 2
- Dec 14th, 2021
- Brit Long
- categories:
Today on the emDOCs cast with Brit Long, MD (@long_brit), we cover two more oncologic emergencies, including tumor lysis syndrome and neutropenic fever.
Episode 43: Oncologic Emergencies Part 2
Hyperleukocytosis/Leukostasis
– Occurs with WBC greater than 50,000 (classically greater than 100,000).
– Leukostasis occurs in the setting of hyperleukocytosis with symptoms and is an emergency.
– May occur with myeloid leukemia (20% of patients) or chronic myeloid leukemia with blast crisis most commonly, but it can occur with other malignances.
– Symptoms are due to white cells plugging microvasculature and/or tissue hypoxemia with cytokine damage, often resulting in respiratory (30% of patients) and neurologic (40%) symptoms.
– If untreated, mortality at one week reaches 40%.
– Pulmonary symptoms include dyspnea and hypoxia. Arterial pO2 levels may be falsely decreased due to the elevated WBCs utilizing O2.
– Neurologic signs/symptoms include vision changes, headache, dizziness, tinnitus, ataxia, confusion, and coma. Patients with hyperleukocytosis have increased risk of intracranial hemorrhage for at least one week after treatment.
– Close to 80% of patients will display fever, so provide antibiotics. Myocardial ischemia, limb ischemia, and renal disease may also be present.
– Labs: High WBC (often above 100,000), falsely elevated platelets, and hyperkalemia. DIC is present in 40%.
– Management involves lowering the WBC count by cytoreduction (induction chemotherapy or leukopheresis), so hematology/oncology must be emergently consulted. Adequate fluid resuscitation is vital to maintain perfusion to end organs. Only chemotherapy has been shown to reduce mortality, as opposed to leukopheresis. Hydroxyurea (50-100 mg/kg/day) is also an option for asymptomatic hyperleukocytosis patients. DIC and tumor lysis syndrome are major risks during the treatment of leukostasis.
Neutropenic Fever
– Neutropenic fever is a commonly treated condition in the ED and an oncologic emergency. The cytotoxic medications used to treat malignancy have several effects on the body besides killing the cancer: the medications affect myelopoiesis (or production of blood/immune cells) and destroy the integrity of the gastrointestinal mucosa, allowing microbe translocation.
– The absolute neutrophil count (ANC) reaches its nadir at 5-14 days after chemotherapy.
– Fever is often the earliest, and sometimes only, manifestation of infection in these patients due to the muted inflammatory response. Many patients with cough and pneumonia will not show an infiltrate on chest Xray, which depends on the body’s neutrophil response to infection, while those with cellulitis may have more subtle erythema.
– Diagnosis per Infectious Diseases Society of America:
- A single oral temperature >38.3°COR a sustained temperature >38.0°C for 1 h, and
- an absolute neutrophil count (ANC) <500 cells/μLOR <1000 cells/μL with an expected decrease to <500 cells/μL. ANC is calculated by: (% neutrophils + % bands) × white blood cell (WBC) count (cells/μL).
– Notice this is an oral temperature, but if the patient has mucositis, then use tympanic membrane or axillary thermometry. Classically rectal temperatures are avoided due to risk of local mucosal trauma and bleeding.
– 20-30% of fevers in neutropenic patients are due to infection. Bacteria are the most common infectious cause, and the species is usually part of the endogenous flora (up to 80). Gram-positive bacteria became most common (60% of cases), specifically S. epidermidis . Gram-negative infections are typically more serious. Fungal pathogens are more common in high-risk patients with prolonged antibiotic use and increasing number of treatment cycles. Most viral pathogens affect those high-risk patients and are due to reactivation (70%), rather than primary infection.
– High-risk patients are those presenting with shock or are critically ill, ANC levels < 500, ANC levels that are low for > 7 days, or other organ dysfunction (liver/kidney).
– Several risk scores for stratification include the MASCC risk index and the CISNE score.
– MASCC: Use in neutropenic patients with fever at least 100.4°F (38ºC). Do not use in patients with acute leukemia undergoing induction chemotherapy or allogeneic hematopoietic stem cell transplant conditioning, per IDSA guidelines. Patients with scores > 21 have low risk for adverse events, but those with scores, < 21 are high risk.

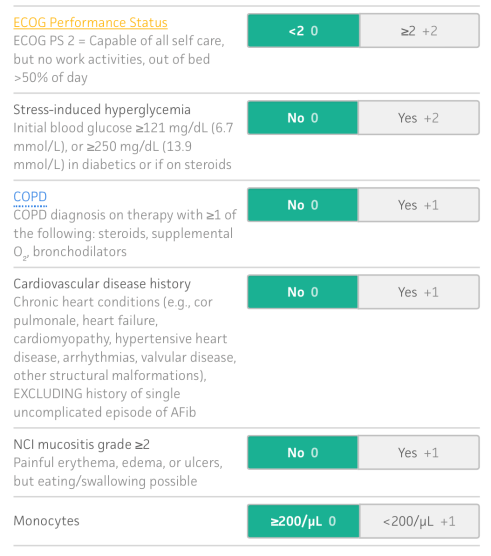
– CISNE: For use in adult outpatients ≥18 years old with solid tumor, fever ≥38°C (100.4°F) over 1 hour, and neutropenia (500 cells/mm³or fewer, or 1,000 cells/mm³ with expected decrease to 500). It should not be used in patients who are obviously unwell, defined by the original study authors as any of the following: acute organ failure (renal, cardiac, and respiratory), decompensation of chronic organ insufficiency, septic shock and hypotension (systolic BP <90 mmHg), known severe infection, or other serious complications that would themselves require admission. Low risk is 0, intermediate is 1-2, and high risk is 3 or more.
– Management of these patients revolves around early recognition of neutropenic fever. CBC and blood cultures with lactate, urinalysis, renal function panel, liver function panel, chest x-ray, and ECG are also recommended.
– Guidelines quote 60 minutes as the timeframe within which patients should be given bug juice after recognition. If antibiotics are delayed, mortality rates can reach 70%.
– Empiric treatment within sixty minutes is aimed at treating the most likely and virulent pathogens. Broad-spectrum coverage includes gram-positive and negative bacteria. IDSA guidelines state those high-risk patients should start with cefepime 2g, meropenem 1g, or piperacillin-tazobactam 4.5g. Ceftazidime 2g monotherapy has increasing resistance among gram-negative bacteria and does not adequately cover gram-positive bacteria. Vancomycin should only be added in the setting of the following: skin/soft tissue/central line infections, pneumonia, mucositis, or hemodynamic shock. If necrotizing mucositis, intraabdominal/pelvic infection, sinusitis, or perirectal cellulitis is present, then add anaerobic coverage. Monotherapy against Pseudomonas, as opposed to dual coverage, has equivalent outcomes with less adverse events. If penicillin allergic, use ciprofloxacin plus clindamycin or aztreonam plus vancomycin. An empiric antifungal agent should be added if fungal infection is suspected, after 4-7 days in high-risk patients with no change in temperature, and if reassessment/clinical studies have not demonstrated a cause of infection.
– For central lines, there is a great deal of controversy surrounding the removal of these lines if they are suspected as the source. There is a grade 1B recommendation for removal of the central line for S. aureus, P. aeruginosa, or Candida. A pocket infection or deep infection along the central line track or port is also cause for removal. Speak with the oncologist and admitting physician regarding line removal.
– Low risk patients based on clinical decision making and/or clinical scoring may be appropriate for discharge. This decision should be made with oncology, with rapid follow-up. Success rates in outpatient treatment are approach 80%, with 20% needing readmission. Those at risk for failing outpatient treatment includes age > 70 years, poor performance status at home, severe mucositis, and neutropenia less than 100. Regimens include ciprofloxacin plus amoxicillin/clavulanic acid, with ciprofloxacin and clindamycin another option for penicillin-allergic patients.

One thought on “emDOCs Podcast – Episode 43: Oncologic Emergencies Part 2”