emDOCs Podcast – Episode 79: Open Globe Injury
- Jun 6th, 2023
- Jess Pelletier
- categories:
Today on the emDOCs cast with Brit Long, MD (@long_brit), we discuss a open globe injury with Jess Pelletier, MD.
Episode 79: Open Globe Injury
Incidence:
- Incidence of OGI is 2-6 cases per 100,000 population; males ages 10-30 account for 80% of cases
- Causes: Penetrating injuries, motor vehicle accidents, fights, and sports
- Risks: Eye surgery, connective tissue diseases
- OGI is a vision-threatening diagnosis; worse prognosis with delay to definitive care with antibiotics and surgery
- Surgical intervention within 12-24 hours is associated with lower rates of endophthalmitis and improved vision
- Up to 75% of appropriately treated patients can have vision measurable with a Snellen chart
- Among all cases, approximately 9% have no light perception, and 39% experience 20/40 vision or better in the affected eye
Definition:
- OGI occurs with complete penetration of all layers of the eye wall that may lead to endophthalmitis and vision loss
- Subcategories: laceration versus rupture
- Laceration is further subcategorized into penetration (only an entry wound present), perforation (entry and exit wounds present), and intraocular foreign body (IOFB)
- Mixed injury patterns do occur
- Rupture occurs with blunt trauma, usually at weak points such as the limbus, locations of prior surgery, optic nerve, or rectus muscle insertions on the globe
- Perforation, penetration, and IOFB are forms of sharp trauma due to lacerations of the globe
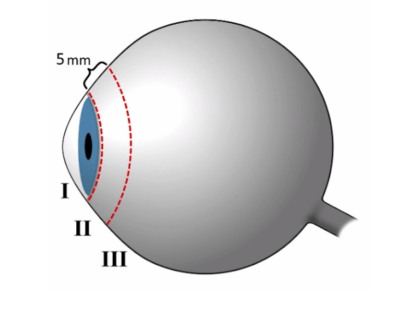
- Extent of injury using anatomical zones: Zone 1 extends from cornea to limbus; zone 2 extends from the limbus to 5 mm posterior to the limbus; zone 3 involves any area posterior to 5 mm behind the limbus
Pathophysiology:
- Three layers to the eye: cornea (anteriorly) and sclera (posterior to the limbus); uvea; and the retina
- Anterior chamber: space between the cornea and anterior edge of the iris/lens and contains aqueous humor
- Posterior chamber: extends from the posterior surface of the iris to the posterior edge of the ciliary body and the lens and is involved in production and circulation of aqueous humor
- Vitreous chamber is the largest and extends from the ciliary body posteriorly to the back of the eye where the retina is located; contains vitreous humor, which assists in supporting the posterior lens and maintaining the ocular shape
- Any traumatic injury can result in OGI, including blunt and penetrating mechanisms, including intraocular foreign bodies (IOFB)
- With OGI there’s risk of extrusion of intraocular contents and endophthalmitis (3-30%), as well as complete vision loss
Presentation:
- Eye pain and change in visual acuity
- Suspect OGI if there are injuries to the adnexa (such as lacerations), orbital floor fracture, or retrobulbar hemorrhage
- Most common mechanisms of OGI are striking against an object or person, cutting or piercing, accidental entry of a foreign body, falls, assault, motor vehicle collision, firearms, and machinery.
- Work-related injuries seem to universally be the most common cause of OGI
- Patients presenting with eye pain or vision changes after a work-related accident or a traumatic mechanism should raise concern for OGI
ED Evaluation:
- Evaluate and stabilize life-threatening injuries first
- Eye exam:
- Visual acuity with Snellen chart (then count fingers, motion, light perception)
- Pupils (contours, APD)
- Confrontation and extraocular movements
- Gross exam/general appearance (orbits, lids, conjunctivae, pupils looking for uveal prolapse, peaked pupil/teardrop shaped, hyphema)

-
- Seidel test: apply topical anesthetic eye drop to the affected eye, followed by application of a moistened fluorescein strip to the area with the suspected leak. You can also apply the fluorescein to the superior conjunctiva, allowing the dye to flow down the cornea. Visible fluorescein flow under Woods lamp or cobalt blue light = OGI. No need for Seidel test if there’s obvious globe rupture.

-
- Literature suggests we should avoid evaluating ocular pressure, though there are no case reports or peer reviewed data documenting extrusion of ocular contents from ocular pressure evaluation in the ED setting.
- If obtained, pressures < 5-10 mm Hg are suggestive of OGI
- Literature suggests we should avoid evaluating ocular pressure, though there are no case reports or peer reviewed data documenting extrusion of ocular contents from ocular pressure evaluation in the ED setting.
Imaging:
- CT can be obtained, but sensitivity ranges from 51-77%, and the specificity ranges from 75-100%
- CT findings: IOFB (only reliable for radiopaque objects), intraocular air, volume loss in the eye, decreased depth of the anterior chamber, globe deformity, displaced lens, and irregular scleral contour

- Ultrasound may be helpful, with high sensitivities and specificities
- Prospective studies and case reports that have evaluated the use of POCUS for globe rupture did not demonstrate any adverse events, but further data are required before this is utilized routinely for diagnosis
Management:
- Early ophthalmology consultation
- Placing an eye shield over the eye to protect it from further damage
- Avoiding removal of foreign bodies
- Make the patient NPO
- Treating pain and nausea to prevent Valsalva maneuver that could be associated with crying or vomiting
- Updating tetanus status if needed
- Administering broad-spectrum antibiotics, including vancomycin and a third- or fourth-generation cephalosporin (which can be substituted with a quinolone if the patient has a cephalosporin allergy). Antifungal coverage should be added in discussion with the ophthalmologist if the OGI involves dirt or there is an IOFB. Ophthalmology may proceed with intravitreal injection of amphotericin B or voriconazole given the lower risk of systemic side effects. Oral and intravitreal fluconazole have also been used for OGI; oral fluconazole has fewer systemic side effects than the aforementioned agents and good penetration of the eye
Prognosis:
- Time to antibiotics and surgery most important factor in determining prognosis
- Blunt mechanism of injury, initial visual acuity of hand movements or worse, relative APD, posterior wound location, metallic IOFB, associated injuries (lid laceration, lens damage, hyphema, retinal detachment, vitreous hemorrhage), endophthalmitis are associated with poor prognosis
Pearls:
- The extent of injury in OGI can be described using anatomical zones.
- Visual prognosis is determined by the time to surgical intervention.
- High-velocity projectiles or direct blunt trauma to the globe should raise concern for OGI, especially if there are associated facial fractures or injuries to the adnexa.
- The classic patient with OGI is a male injured at work, but the disease must be considered in any traumatic mechanism, including elderly patients with falls.
- Suspected OGI patients need a full ophthalmologic examination; however, assessment of ocular pressure is not recommended in the ED.
- Classic examination findings include a peaked pupil and positive Seidel test.
- OGI is a clinical diagnosis; imaging with CT may suggest the disease, but it cannot definitively exclude it.
- POCUS is controversial and should likely be avoided at the current time.
- Treatment includes covering the eye with an eye shield, avoiding removal of any foreign bodies, preventing Valsalva maneuvers, ensuring adequate tetanus vaccination status, and administering broad-spectrum antibiotics. Consider fungal coverage for soil involvement or cases of IOFB.
References:
