Pediatric Small Talk – The Rhythm Is Gonna Get Ya’: Age Based Approach to Pediatric Narrow Complex Tachydysrhythmia
- Jan 5th, 2022
- Joe Ravera
- categories:
Welcome back to Small Talk; a new monthly section from emDOCs. Every first Wednesday of the month we will release high yield PEM content written by PEM talent from around the country. We hope you enjoy these reviews. Comments, questions, accolades or concerns: feel free to reach out to Joe Ravera, MD (pemgemspod@gmail.com).

Author: Joe Ravera, MD (@pemuvm1, Director of Pediatric Emergency Medicine, Assistant Professor of Surgery, Division of Emergency Medicine, University of Vermont Medical Center) // Reviewed by Alex Koyfman, MD (@EMHighAK) and Brit Long, MD (@long_brit)
Cases
Case 1: A 6-month-old presents with fussiness and difficulty feeding. On exam there the infant is tachypneic and tachycardic. The initial triage heart rate is 210.
Case 2: A 4-year-old presents with a “funny feeling” in his chest. He has a history of a repaired VSD but no cardiac restrictions. His triage heart rate is 200.
Case 3: A 16-year-old presents with palpitations after drinking an energy drink. The patient has no previous cardiac history. The initial triage heart rate is 180.
Epidemiology, Evaluating Risk, and Expanding the Diagnosis of “SVT”
Pediatric narrow complex tachycardia, commonly referred to as Supraventricular Tachycardia (SVT), is the most common rhythm disturbance in pediatrics, with an estimated prevalence of 1 in 250-1000. The range of presentations varies from subtle fussiness to palpitations. The spectrum of disease also varies from well-tolerated palpitations to fulminant cardiogenic shock – particularly in children with a history of structural congenital heart disease (CHD). Dysrhythmia disproportionately effects children with CHD – up to 7% of children with CHD have dysrhythmia, as opposed to less than 1% without it – and, moreover, these children may not have the cardiac reserve to tolerate sustained tachycardia.1,2 Children with both structural disease and rhythm disturbance are a high-risk population and early consultation with pediatric cardiology/PICU is recommended.
In a crisis, a PALS algorithm card can be extremely helpful for quick reference and management (Figure 1).3

As clinicians we often use the term “supraventricular tachycardia” (SVT) as shorthand for discussing narrow complex tachydysrhythmias. The classification of SVT is helpful to make rapid decisions with a deteriorating patient in critical situations. However, when there is time to think about the underlying disorder it is important to remember that SVT encompasses multiple different rhythms, each with a different pathophysiology.
SVT includes the rhythms:
- Sinus Tachycardia
- Atrial Fibrillation
- Atrial Flutter
- Multifocal Atrial Tachycardia
- Junctional Ectopic Tachycardia
- Atrial Ectopic Tachycardia
- AV Nodal Reentrant Tachycardia (AVNRT)
- Atrioventricular Reciprocating Tachycardia (AVRT)
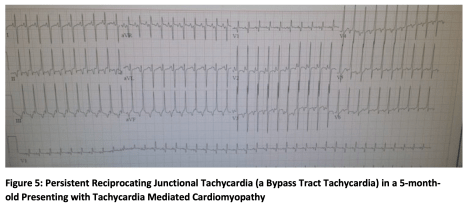
SVT often refers to either atrial ectopic tachycardia or, more commonly, to a reentrant tachycardia like AV nodal reentrant tachycardia (AVNRT) or atrioventricular reciprocating tachycardia (AVRT) (Figure 2). While they sound similar, there is a major physiologic difference between AVRT and AVNRT – AVRT has a bypass tract which has implications for therapy with AV nodal blockade. Making this distinction on a dysrhythmic EKG can be extremely difficult, if not impossible. It should be noted that age is a strong predictor of AVRT since most children under 8 and nearly all children under 1 have a bypass tract (Figure 3).4


Infant Tachydysrhythmia: The Challenge is Recognition
The main difficulty in managing infant SVT is actually making the diagnosis. There are several factors which make recognition challenging: infants have higher resting heart rates and can tolerate tachycardia; they are non-verbal; and they do not have the exertional demands of older children. Given these factors, the presentation can vary from subtle symptoms like fussiness or fatigue to the more overt increased work of breathing and tachycardia mediated cardiomyopathy. A percentage of infants with SVT can be sub-clinically symptomatic or asymptomatic for an extended period of time.5
To make matters more difficult, infants’ naturally higher heart rate can be exacerbated by stress such as fever or pain, so the challenge becomes differentiating sinus tachycardia from a pathologic reentrant tachycardia. Several EKG features, notably the rate, variability, and presence of p-waves, can help make the distinction (Table 1).


After diagnosing reentrant tachycardia, patient management and disposition are straightforward. Nearly all reentrant tachycardia in this age group is associated with a bypass tract. While AV nodal blockade is the initial treatment, it must be respected – and these patients should have electrical cardioversion pads in place before chemical cardioversion is attempted.
Before trying chemical cardioversion, vagal maneuvers (such as a placing a bag of ice on the face or taking a rectal temperature) can be attempted. If this is unsuccessful, pharmacologic cardioversion with adenosine (0.1 mg/kg) should be attempted. If there is no rhythm change at all, attempts should be made at better access, a faster mediation push, and/or an increased dose to 0.2 mg/kg. Occasionally, if access is difficult and there is no pause in the rhythm achieved with 0.2 mg/kg, the dose can be increased to 0.3 mg/kg.5
If this is a first episode, the child will almost certainly be admitted even if ED cardioversion is successful. Discharge may be possible but only in consultation with pediatric cardiology.
Older Children and Adolescents with SVT: Easier to Diagnose, Straightforward to Manage, but More Nuanced Dispositions
As opposed to infants, diagnosing SVT in verbal children is usually not subtle. They will often present with palpitations. Moreover, in the absence of structural cardiac disease, they will often be relatively stable with normal perfusion.
Initial history taking should focus on the presence of structural cardiac disease, any previous episodes, and an underlying diagnosis like Wolf-Parkinson-White. Absent those, the history can focus on other cardiac questions such as the child’s baseline exercise tolerance.
The electrocardiographic distinction of a bypass tract is typically not possible from the dysrhythmic EKG (Figure 6). A post conversion EKG (Figure 7) and during conversion rhythm strip will be the most helpful in determining the presence of a bypass tract. It should be noted that a normal post-conversion EKG does not exclude the diagnosis of a bypass tract.


The initial treatment for a reentrant tachycardia, regardless of the presence of a bypass tract, is adenosine 0.1 mg/kg (adult dose 6 mg) increasing to 0.2 mg/kg (adult dose 12 mg) if the lower dose is unsuccessful. While there is concern about using medications that cause AV nodal blockade in patients with an undiagnosed bypass tract, proper preparation can help manage these concerns. One study examining children in the cath lab with known bypass tract found a transient run of atrial fibrillation in approximately 12% of patients receiving adenosine. Atrial fibrillation in patients with a bypass tract is a risk factor for ventricular fibrillation and, as such, this needs to be a consideration.1,3,6 The current recommendations are that adenosine is a reasonable choice for SVT in the presence of a bypass tract, as long as appropriately sized resuscitative equipment is readily available, and the patients are prepared with pads on. In short, respect these kids when you give them adenosine.
Assuming these patients are successfully cardioverted, the next question that comes up is disposition. In patients with a known diagnosis, a discussion with their pediatric cardiologist can be helpful, and most of these kids should be able to go home.
If this is a first presentation, the critical question is often- Do these children have underlying structural heart disease? In the absence of structural heart disease, the risk of sudden cardiac death in children with Wolf-Parkinson-White and dysrhythmia is low.7 In this case, a discussion with pediatric cardiology to assure follow-up may be appropriate if there are no red flags for undiagnosed structural disease (e.g. cardiac murmurs or exercise intolerance).
Failed Cardioversion and Special Circumstances
While most patients presenting with SVT will be stable and will convert with adenosine. There is a subset of patients who are either unstable or will have a rhythm that does not respond to adenosine. Unstable patients with hypotension or poor perfusion are straightforward and require emergent cardioversion with 0.5-2 J/kg for a narrow complex tachycardia.3
Patients who don’t convert with adenosine usually fall in to one of two categories. The first did not have a pause and, in this case, they simply need a higher dose of adenosine given as fast and as close to the heart as possible. The second category – when there was a noticeable pause, but the patients then re-enter the abnormal rhythm – is more challenging. In these patients, look for an underlying etiology such as sepsis, a toxidrome, or concomitant structural heart disease.
Patients with an underlying etiology will require longer acting rhythm control, which can be done in consultation with a pediatric cardiologist. As a quick guideline, this author recommends avoiding AV nodal blocking agents in patients with a known or suspected bypass tract, which makes procainamide a good first line agent. In patients without a bypass tract, a longer acting AV nodal blocking agent like diltiazem could be considered.
Lastly, it is important to remember that electrical cardioversion is always an option and, while there may be a mental block to performing this procedure in children, functionally it is no different than adults. Occasionally, patients have a rhythm that adenosine will not terminate such as atrial flutter (Figure 8 and 9) and cardioversion after sedation may be a reasonable option.


Pearls and Pitfalls:
- The presentation of SVT varies by age and can be subtle in infants
- Most children and nearly all infants have an associated bypass tract
- Beware the child with structural and dysrhythmic heart disease – call for help early
- Adenosine is first line in SVT, even in known WPW, but respect the cardioversion and have pads on.
- Have a plan if the adenosine fails – don’t be afraid of electrical cardioversion if needed.
References:
- Manole MD, Saladino RA. Emergency department management of the pediatric patient with supraventricular tachycardia. Pediatr Emerg Care. 2007 Mar;23(3):176-8
- Tripathi A, Black GB, Park YM, Jerrell JM. Factors associated with the occurrence and treatment of supraventricular tachycardia in a pediatric congenital heart disease cohort. Pediatr Cardiol. 2014 Feb;35(2):368-73.
- Topjian AA, Raymond TT, Atkins D, et al. Pediatric Basic and Advanced Life Support Collaborators. Part 4: Pediatric Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020 Oct 20;142(16_suppl_2):S469-S523.
- Ko JK, Deal BJ, Strasburger JF, Benson DW Jr. Supraventricular tachycardia mechanisms and their age distribution in pediatric patients. Am J Cardiol. 1992 Apr 15;69(12):1028-32.
- Moak JP. Supraventricular tachycardia in the neonate and infant. Prog Pediatr Cardiol. 2000 May 1;11(1):25-38.
- Strickberger SA, Man KC, Daoud EG et. al. Adenosine-induced atrial arrhythmia: a prospective analysis. Ann Intern Med. 1997 Sep 15;127(6):417-22.
- Pappone C, Vicedomini G, Manguso F, et. al. Risk of malignant arrhythmias in initially symptomatic patients with Wolff-Parkinson-White syndrome: results of a prospective long-term electrophysiological follow-up study. Circulation. 2012 Feb 7;125(5):661-8.

One thought on “Pediatric Small Talk – The Rhythm Is Gonna Get Ya’: Age Based Approach to Pediatric Narrow Complex Tachydysrhythmia”