Tox Cards: Sulfonylurea-induced hypoglycemia
- Aug 3rd, 2017
- Adriana Garcia
- categories:
Author: Adriana Garcia, MD (Fidel Velázquez Sánchez Hospital) // Edited by: Cynthia Santos, MD (Assistant Professor of Emergency Medicine and Toxicology, Rutgers University Hospital), Alex Koyfman, MD (@EMHighAK, EM Attending Physician, UT Southwestern Medical Center / Parkland Memorial Hospital) and Brit Long, MD (@long_brit)

Case:
A 5 y/o girl is brought in by her family after being found unresponsive. Grandma’s morning dose of glipizide which she left on the kitchen table is missing. She was taken immediately to the ED by her parents. The ED calls the poison center for management. She had 2 glucose levels that were less than 40, and she is still sleepy. She has been started on a dextrose infusion, but apparently she is a hard stick so they do not want to start another line to give octreotide…
Question:
What is the management of sulfonylurea-induced hypoglycemia, and how does octreotide treat it?
Pearl:
- The time to recurrent hypoglycemia depends on the type and dose of sulfonylurea ingested, administration of food, frequency and duration of octreotide, and the maintenance dextrose infusion dose.
- Children can present with delayed hypoglycemia after ingestion despite having initial normal blood glucose levels and receiving treatment. Food and IV glucose can also delay onset of hypoglycemia.
- In a retrospective study of 1,943 sulfonylurea pediatric poisonings, 10% of the children had hypoglycemia occurring or persisting more than 12 hours after ingestion despite receiving treatment. The mean (SD) time to onset of hypoglycemia in children not given any prophylactic treatment was 2.0 (1.2) hours. The mean (SD) times in children receiving prophylactic food only, IV glucose only, and both food and IV glucose were 5.9 (3.9), 5.7 (2.5), and 8.9 (3.6) hours, respectively. 18% of the patients who received prophylactic food only had onset of hypoglycemia > 8 hours after sulfonylurea ingestion.[1]
- After recognizing hypoglycemia you can start with IV dextrose and feed the patient. An “amp” of D50W provides 25 gm of dextrose. The patient must eat as soon as decontamination phase ends (lavage, activated charcoal) and if the patient is awake, alert, and has no nausea or vomiting.
- Newborns can be given 0.5 – 1 g/kg (4-8 ml/kg) D12.5W IV or IO. In a child, D25W can be given peripherally at 0.5-1gm/kg or 2-4ml/kg IV or IO. Remember you cannot use D25W in newborns! D50 should be used exclusively in adults at 1 ml/kg.
- Octreotide should be considered first-line therapy in both pediatric and adult sulfonylurea poisoning with clinical and laboratory evidence of hypoglycemia.
- The recommended dose for octreotide in children is 1 – 2 mcg/kg up to 50 mcg SC or IV every 6-12 hours; in adults, octreotide 50 – 100 mcg SC or IV every 6-12 hours. The SC route is preferred. During this treatment IV dextrose infusion should be gradually tapered off. [Table 1, Ref 2]

- Octreotide prevents rebound hypoglycemia after treatment of sulfonylurea overdose with dextrose. By mimicking somatostatin, octreotide suppresses the secretion of gastrin, cholecystokinin, growth hormone, glucagon, and insulin.
- Voltage-gated calcium channels on pancreatic beta cells are bound by G-protein-coupled somatostatin-2 receptors. When octreotide binds to the somatostatin receptors, the calcium channels close, preventing the influx of calcium and subsequent secretion of insulin. (Fig. 1)
Fig. 1 Mechanism of sulfonylureas antidotes.[Ref 3]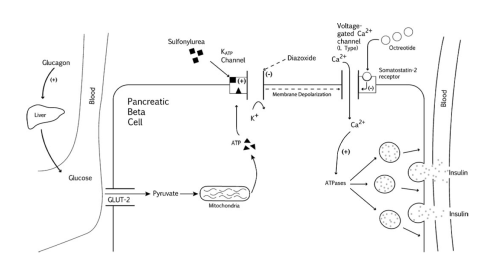
Main Point:
Hypoglycemia can be delayed, so patients will need to be admitted at least 24 hours. Children can present with delayed hypoglycemia after ingestion despite having initial normal blood glucose levels and receiving treatment. Food and IV glucose can also delay onset of hypoglycemia. Remember to give food to your sulfonylurea ingestions (if awake and alert, no n/v, and after GI decon). Hypoglycemic children will require dextrose infusions and octreotide. Octreotide can and should be given subcutaneously so not wanting to start another line is not a good reason to not start it.
This post is sponsored by www.ERdocFinder.com, a supporter of FOAM and medical education, who with their sponsorship are making FOAM material more accessible to emergency physicians around the world.
References / Further Reading:
- Lung D, Olson K. Hypoglycemia in Pediatric Sulfonylurea Poisoning: An 8-Year Poison Center Retrospective study. Pediatrics 2011; 127(6):e1558-64.
- Glatstein M. Octreotide for the treatment of sulfonylurea poisoning. Clin Tox 2012; 50(9):795-804.
- Dougherty P. Octreotide’s Role in the Management of Sulfonylurea-Induced Hypoglycemia. J. Med. Toxicol 2010; 6(2):199-206.


One thought on “Tox Cards: Sulfonylurea-induced hypoglycemia”