Trauma ICU Rounds – The rEVOLUTION of ECMO
- Jan 8th, 2021
- Dennis Kim
- categories:
Originally posted on Trauma ICU Rounds on May 8, 2020 – Visit to listen to accompanying podcast. Follow Trauma ICU Rounds (@traumaicurounds) and Dr. Kim (@dennisyongkim) to learn more on simplifying trauma critical care together.
What are the indications for ECMO beyond ARDS and refractory cardiogenic shock? In which patients should we consider eCPR and is this the new standard of care for patients sustaining out-of-hospital cardiac arrest? Finally, how do I work towards safely and efficiently weaning my patient from VV or VA ECMO?
These are just a few of the questions that we address on Rounds with our guest faculty member and Director of the UCLA Adult ECMO Program, Dr. Peyman Benharash. In this comprehensive review of ECMO we also explore the regionalization of ECMO care here in Los Angeles County, as well as the day-to-day considerations that you want to bear in mind when assessing and caring for your patients requiring extracorporeal life support.
Learning Objectives
By the end of rounds you should be able to:
1. Understand the indications & contraindications to VV and VA ECMO support
2. Describe the basic components of an ECMO circuit
3. Describe the role of eCPR in the management of adult patients with out-of-hospital cardiac arrest
4. Discuss key management strategies to safely wean patients from ECMO
5. Describe common complications of ECMO and strategies to mitigate them
Take Home Points
- ECMO is time-sensitive, therefore, early and safe cannulation is an important determinant of outcome
- ECMO is a bridge to therapy
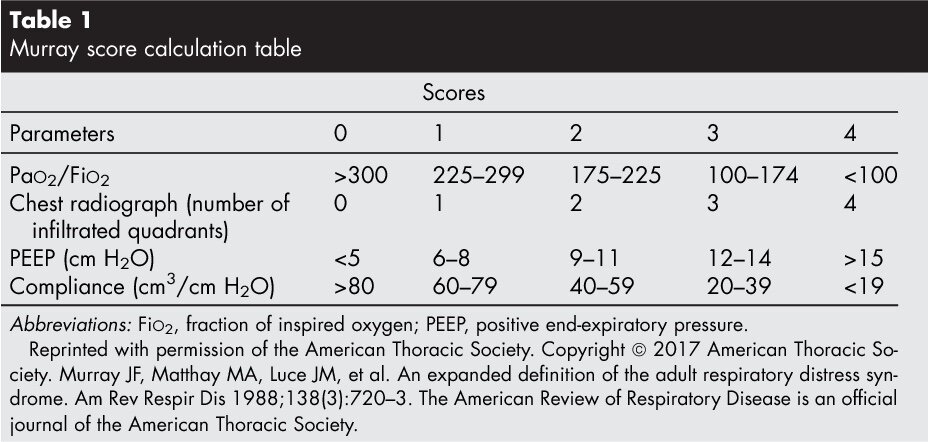
- Use of scoring systems like the Murray Score may be useful to stratify the severity of ARDS among patients being considered for VV ECMO support
- The indications for ECMO are expanding to include technically challenging operative cases
- eCPR is a promising therapy for patients presenting to an ECMO center of excellence with refractory VF/VT cardiac arrest
- ECMO therapy, particularly VA ECMO, may affect virtually organ system
- The potential role of ECMO therapy during the current COVID-19 pandemic remains to be defined
Time Stamps
- 00:12 Introduction
- 01:16 Overview of Rounds
- 02:13 The rise of ECMO
- 02:46 CESAR & EOLIA trials summarized
- 05:40 Venovenous (VV) vs. Venoarterial (VA) ECMO
- 08:24 How to decide whether or not to place a patient on VA ECMO?
- 10:33 Timing & indications for ECMO support
- 11:38 Murray Score explained
- 12:24 Contraindications & patient selection for VV & VA ECMO
- 13:56 Expanding indications for ECMO
- 15:23 ECMO in the Setting of Trauma: Pneumonectomy & Retrohepatic IVC injuries
- 17:45 Regionalization of ECMO in Los Angeles County
- 21:52 Who should be cannulating?
- 23:22 Approach to cannulation
- 24:50 Distal perfusion catheters for VA ECMO
- 26:10 Differences between VV & VA ECMO
- 28:24 The W5H of eCPR
- 34:26 Considerations for access for VV ECMO
- 35:53 Avalon catheter
- 37:51 VV versus VA ECMO circuits/set-up explained
- 43:30 Getting your patient off of ECMO & other key considerations
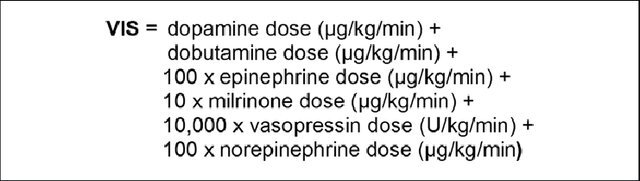
- 48:56 Vasopressor & inotropic therapy during VA ECMO
- 50:31 Virchow’s triad, antithrombotic therapy & bleeding on ECMO
- 54:30 AKI, end-organ dysfunction & the daily assessment of patients on ECMO
- 57:22 ECMO 2.0 & the role of evolving technologies
- 61:20 Role of ECMO during the COVID-19 pandemic
- 66:45 Take-home points
- 68:38 Outro
What are the indications for ECMO beyond ARDS and refractory cardiogenic shock? In which patients should we consider eCPR and is this the new standard of care for patients sustaining out-of-hospital cardiac arrest? Finally, how do I work towards safely and efficiently weaning my patient from VV or VA ECMO?
These are just a few of the questions that we address on Rounds with our guest faculty member and Director of the UCLA Adult ECMO Program, Dr. Peyman Benharash. In this comprehensive review of ECMO we also explore the regionalization of ECMO care here in Los Angeles County, as well as the day-to-day considerations that you want to bear in mind when assessing and caring for your patients requiring extracorporeal life support.
Learning Objectives
By the end of rounds you should be able to:
1. Understand the indications & contraindications to VV and VA ECMO support
2. Describe the basic components of an ECMO circuit
3. Describe the role of eCPR in the management of adult patients with out-of-hospital cardiac arrest
4. Discuss key management strategies to safely wean patients from ECMO
5. Describe common complications of ECMO and strategies to mitigate them
Take Home Points
-
ECMO is time-sensitive, therefore, early and safe cannulation is an important determinant of outcome
-
ECMO is a bridge to therapy
-
Use of scoring systems like the Murray Score may be useful to stratify the severity of ARDS among patients being considered for VV ECMO support
-
The indications for ECMO are expanding to include technically challenging operative cases
-
eCPR is a promising therapy for patients presenting to an ECMO center of excellence with refractory VF/VT cardiac arrest
-
ECMO therapy, particularly VA ECMO, may affect virtually organ system
-
The potential role of ECMO therapy during the current COVID-19 pandemic remains to be defined
Time Stamps
-
00:12 Introduction
-
01:16 Overview of Rounds
-
02:13 The rise of ECMO
-
02:46 CESAR & EOLIA trials summarized
-
05:40 Venovenous (VV) vs. Venoarterial (VA) ECMO
-
08:24 How to decide whether or not to place a patient on VA ECMO?
-
10:33 Timing & indications for ECMO support
-
11:38 Murray Score explained
-
12:24 Contraindications & patient selection for VV & VA ECMO
-
13:56 Expanding indications for ECMO
-
15:23 ECMO in the Setting of Trauma: Pneumonectomy & Retrohepatic IVC injuries
-
17:45 Regionalization of ECMO in Los Angeles County
-
21:52 Who should be cannulating?
-
23:22 Approach to cannulation
-
24:50 Distal perfusion catheters for VA ECMO
-
26:10 Differences between VV & VA ECMO
-
28:24 The W5H of eCPR
-
34:26 Considerations for access for VV ECMO
-
35:53 Avalon catheter
-
37:51 VV versus VA ECMO circuits/set-up explained
-
43:30 Getting your patient off of ECMO & other key considerations
-
48:56 Vasopressor & inotropic therapy during VA ECMO
-
50:31 Virchow’s triad, antithrombotic therapy & bleeding on ECMO
-
54:30 AKI, end-organ dysfunction & the daily assessment of patients on ECMO
-
57:22 ECMO 2.0 & the role of evolving technologies
-
61:20 Role of ECMO during the COVID-19 pandemic
-
66:45 Take-home points
-
68:38 Outro
Core Concepts, Equations, and Other Stuff
Vasoactive Inotrope Score (VIS)
Murray Score
Recommended Reading
Articles
-
Peek GJ, Mugford M, Tiruvoipati R, et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial [published correction appears in Lancet. 2009 Oct 17;374(9698):1330]. Lancet. 2009;374(9698):1351‐1363. doi:10.1016/S0140-6736(09)61069-2
-
Combes A, Hajage D, Capellier G, et al. Extracorporeal Membrane Oxygenation for Severe Acute Respiratory Distress Syndrome. N Engl J Med. 2018;378(21):1965‐1975. doi:10.1056/NEJMoa1800385
-
Mosier, J.M., Kelsey, M., Raz, Y. et al. Extracorporeal membrane oxygenation (ECMO) for critically ill adults in the emergency department: history, current applications, and future directions. Crit Care 19, 431 (2015). https://doi.org/10.1186/s13054-015-1155-7
-
Schmidt, Matthieua,b; Franchineau, Guillaumea,b; Combes, Alaina,b Recent advances in venovenous extracorporeal membrane oxygenation for severe acute respiratory distress syndrome, Current Opinion in Critical Care: February 2019 – Volume 25 – Issue 1 – p 71-76 doi: 10.1097/MCC.0000000000000567
-
Pineton de Chambrun, Marca,b; Bréchot, Nicolasa,b; Combes, Alaina,bVenoarterial extracorporeal membrane oxygenation in cardiogenic shock: indications, mode of operation, and current evidence, Current Opinion in Critical Care: August 2019 – Volume 25 – Issue 4 – p 397-402 doi: 10.1097/MCC.0000000000000627
-
Kalra, Rajata,∗; Kosmopoulos, Marinosa,b,∗; Goslar, Tomaza,b,c,∗; Raveendran, Ganesha; Bartos, Jason A.a; Yannopoulos, Demetrisa Extracorporeal cardiopulmonary resuscitation for cardiac arrest, Current Opinion in Critical Care: June 2020 – Volume 26 – Issue 3 – p 228-235 doi: 10.1097/MCC.0000000000000717
-
Krishnan, Sundara; Schmidt, Gregory A.b Hemodynamic monitoring in the extracorporeal membrane oxygenation patient, Current Opinion in Critical Care: June 2019 – Volume 25 – Issue 3 – p 285-291 doi: 10.1097/MCC.0000000000000602
-
Guttman, Matthew P. MD1,2; Tillmann, Bourke W. MD1,3; Pannell, Dylan MD, PhD2,4; Vallelonga, Mark CCP5; Nathens, Avery B. MD, PhD1,2,6; Haas, Barbara MD, PhD1,2,3,6 Extracorporeal Membrane Oxygenation Use in TQIP Centers, Journal of Trauma and Acute Care Surgery: April 17, 2020 – Volume Publish Ahead of Print – Issue – doi: 10.1097/TA.0000000000002756
-
Huang, James E. DSc; Holland, Seth R. DSc; Patrick, Joshua PhD; Piper, Lydia C. MD; Sams, Valerie G. MD Predictive survival factors of the traumatically injured on venovenous extracorporeal membrane oxygenation, Journal of Trauma and Acute Care Surgery: January 2020 – Volume 88 – Issue 1 – p 153-159 doi: 10.1097/TA.0000000000002457
-
Jacobs, Jordan V. MD; Hooft, Nicole M. MD; Robinson, Brenton R.; Todd, Emily; Bremner, Ross M. MD, PhD; Petersen, Scott R. MD; Smith, Michael A. MD The use of extracorporeal membrane oxygenation in blunt thoracic trauma, Journal of Trauma and Acute Care Surgery: December 2015 – Volume 79 – Issue 6 – p 1049-1054 doi: 10.1097/TA.0000000000000790
-
Ahmad, Sarwat B. MD; Menaker, Jay MD; Kufera, Joseph MA; O’Connor, James MD; Scalea, Thomas M. MD; Stein, Deborah M. MD, MPH Extracorporeal membrane oxygenation after traumatic injury, Journal of Trauma and Acute Care Surgery: March 2017 – Volume 82 – Issue 3 – p 587-591 doi: 10.1097/TA.0000000000001352
Guidelines
AAST Critical Care Committee Clinical Consensus: ECMO
Zonies D, Codner P, Park P for the American Association of the Surgery ofTrauma Critical Care Committee, et al AAST Critical Care Committee clinical consensus: ECMO, nutrition Extracorporeal membrane oxygenation (ECMO)Nutrition Trauma Surgery & Acute Care Open 2019;4:e000304. doi: 10.1136/tsaco-2019-000304
ELSO Guidelines for Adult Respiratory Failure August, 2017
Click to access ELSO%20Guidelines%20For%20Adult%20Respiratory%20Failure%201_4.pdf
ELSO Guidelines for Adult Cardiac Failure
Click to access e76ef78eabcusersshyerdocumentselsoguidelinesforadultcardiacfailure1.3.pdf
ELSO Guidelines for ECPR Cases
Click to access 6713186745cusersshyerdocumentselsoguidelinesforecprcases1.3.pdf
ELSO Guidelines for ECMO in COVID-19
Click to access ELSO%20covid%20guidelines%20final.pdf
Advanced Pulmonary and Cardiac Support of COVID-19 Patients: Emerging Recommendations from ASAIO – A “Living Working Document”!
Click to access ASAIO-COVID19-White-Paper.pdf
Websites
UCLA ECMO Home Page
https://www.uclahealth.org/heart/ecmo
UCLA Core Lab
http://surgery.ucla.edu/corelab
Extracorporeal Life Support Organization
https://www.elso.org
American Society for Artificial Internal Organs
https://asaio.org
Podcast
EAST TraumaCast – ECMO: Overview for the Acute Care Surgeon
https://podcasts.apple.com/us/podcast/ecmo-overview-for-acute-care-surgeon-current-techniques/id464280790?i=1000409201383
