US Probe: Preventing Harmful Delays with POCUS During Cardiac Arrest
- Sep 6th, 2018
- Corlin Jewell
- categories:
Authors: Corlin Jewell (@BigC_MD, EM Resident Physician, University of Wisconsin), Tim Montrief (@EMinMiami, EM Resident Physician, Jackson Memorial Health System), Nikolai Schnittke (@nikolaischnittk, Ultrasound Fellow Physician, University of Wisconsin) // Edited by: Stephen Alerhand MD (@SAlerhand), Brit Long, MD (@long_brit), and Manpreet Singh, MD (@MprizzleER)
The Problem
You hear the trauma chime ring overhead and the entire resuscitation team turns their heads towards the ambulance bay. The doors fly open and EMS rushes the patient into the room with chest compressions ongoing. You quickly take report and transfer the patient over, and that is when the puzzle begins. What caused this man’s arrest? You grab the cardiac transducer on your ultrasound machine and get to work……
With the integration of bedside echocardiography into cardiac arrest, we now have a real-time tool to help us glean some of this critical missing information, as well as offer procedural guidance and prognostic data [1-6]. However, it can be tough to quickly and accurately utilize POCUS in the stress-filled environment surrounding cardiac arrest. For instance, it can take time to acquire images and interpret them, which is often more time than allowed by current guidelines. These suggest that any interruptions in CPR last for a duration of 10 seconds or less with a target chest compression fraction (time during arrest spent performing compressions) of 80% [7-8]. While TEE has been proposed as a potential way to get around some of these challenges and does not require interruption of CPR to perform, it necessitates specialized equipment and training that is not available to all emergency physicians [9,10].

The notion that TTE might cause harmful delays in chest compression is not just theoretical. Two groups (Huis et al. and Clattenburn et al.) recently used video recording of their cardiac arrest resuscitations to demonstrate that rhythm checks are significantly prolonged when POCUS is used, compared to when it is withheld [11,12].

While these studies show that we are generally not able to stay under the recommended 10 seconds during our compression pauses, they certainly indicated that POCUS delays us even further. While the studies are underpowered to detect a survival difference, this observation raises concerns that POCUS may be harming our cardiac arrest patients. The Clattenburg study also looked at some secondary outcomes, such as the CPR pause when the resuscitation leader versus another provider was performing the POCUS (a difference of 6.1 seconds!). In light of this data, one might think that we should be keeping sonography away from the arrests. However, instead of moving away from sonography, another way to approach this data is to recognize the problem and find ways to use ultrasound smarter and faster.
Scanning Smarter and Faster…
Until recently, there has been little research on how to implement better sonographic techniques to facilitate shorter CPR pauses. However, Clattenburg et al. proposed a solution detailed in a 2018 article published in Resuscitation [13]. In this study, they introduce a “Cardiac Arrest Sonographic Assessment” (CASA) protocol that guides how POCUS is used during rhythm checks. It is a sequential process used during the first three rhythm checks of a given arrest.
The Protocol:
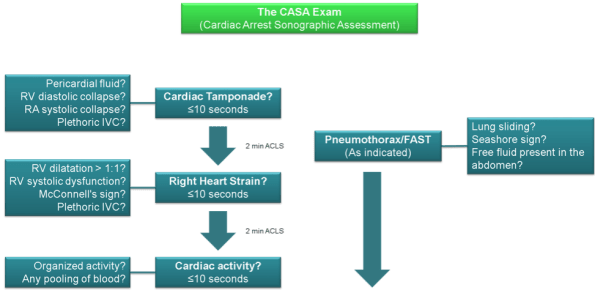
Figure 1. The CASA protocol
As seen above in the figure, the CASA protocol asks a single clinical question during each rhythm check. The probe is also still on the patient in-between checks so that the transducer is in place before the compressions are actually halted. Other work has already shown that TTE during ongoing CPR leads to faster diagnosis of certain etiologies of arrest [14]. By looking for individual causes of cardiac arrest during each pause, rather than all of them at once, the researchers hoped to shorten these checks.
The Results:
Prior to implementation of the CASA protocol, rhythm checks averaged 19.8 seconds. Following implementation and training on the CASA protocol, the average length of these checks was 15.8 seconds (16.5 seconds when controlling for additional independent variables such as the level of training of the operator). They also show a 3.3 second difference in rhythm checks in which the transducer was placed on the patient’s chest in anticipation of the rhythm check (i.e. before compressions were halted). The percentage of CPR pauses lasting less than or equal to 10 seconds jumped from 10% to 19% following implementation of CASA. They reported no significant difference in duration of rhythm checks or the number of patients achieving ROSC between pre and post-CASA implementation in arrests that did not use POCUS.
Reflections on the CASA Protocol
While CASA appears to decrease the amount of time spent during individual rhythm checks, the before-after design of the study carries some limitations. For example, the average rhythm checks decreased by 2.6 seconds without POCUS use. Though the authors report that this is not statistically significant, it is worth mentioning that the site’s focus on awareness of rhythm check length led to a decrease more than 50% of what is reported for the intervention. In addition, even with several interventions, compression pauses remain well above the recommended 10 second limit. This suggests that we still have significant room for improvement and that more work is needed to establish best practices. Despite these concerns, the results are encouraging and show that with some easy-to-incorporate interventions, one can have a significant impact on a smoother resuscitation. In conclusion, let’s break the problem into categories and discuss how additional future work might serve to further limit harmful extension of compression pauses.
Problem 1: There’s too much to look at:
The focus of the CASA study. Their solution is simple but effective; look for one thing at a time! The sequence of clinical questions proposed by CASA reflects the most common reversible causes of arrest, which you can identify by POCUS. It is possible that the differential diagnosis may be different in any given patient, and the order of your clinical questions might change. The philosophical frame-shift here is to not over-do it. One pause, One question!
Problem 2: It is easy to lose track of time:
First, it is important to acknowledge the problem–our rhythm checks are causing significant delays in chest compressions. There are three potential solutions to this problem:
1) Use a timer! A follow-up article presented by Gardner et al. at the same site as the CASA study suggests using a timer or counting down from 10 out loud (though it does look like counting out loud is less accurate) [15].
2) Empower your team to restart compressions! Too often, we as physicians are the cause of prolonged pauses due to asking for more time for intubation, central venous or arterial lines, or POCUS. Before the patient even rolls in, assign a dedicated person to keep track of time during each pause and make it clear that the job of the chest compressor is to compress the chest.
3) The ultrasound machine can HELP! At the University of Wisconsin, the machine is set to record a 6 second clip and then play it back on a loop. When compressions stop, hit the “Clip” button. After 6 seconds, the machine will beep, which signals that it is time to stop scanning and start compressing.
Problem 3: It is hard to find the view in time:
Start scanning before compressions start. We recommend preparing for the rhythm check like a NASCAR pit crew. Five to fifteen seconds before the rhythm check, put the transducer in the subxiphoid space, assign a timer, and precharge your defibrillator. Indeed, one of the secondary outcomes of the CASA study shows that placing the transducer on the chest in anticipation of the rhythm check resulted in shorter interruptions in chest compressions. This gives the sonographer a headstart on finding the adequate cardiac window, thus saving precious seconds. There is no reason to stop compressions before all the pieces are in place for a successful rhythm check.
Problem 4: I cannot interpret these images in time:
Interpret AFTER the compressions restart. Rather than trying to hold compressions until you know what is going on, separate the time for data gathering and the time for interpretation. Setting the machine to continuously loop your 6 second clip will allow the team to see the images and help interpret them. Now, interventions can be implemented during chest compressions and then reassessed again at the next pause. The CASA study also showed that ultrasound fellowship trained physicians had shorter rhythm checks in between cycles of compressions, indicating that acquiring (and to a certain extent, interpreting) the appropriate image is a barrier to efficient resumption of compressions. Therefore, if possible, the person chosen to perform the TTE should be the most experienced sonographer. This also highlights the importance of effective ultrasound training in EM training programs.
Take-Home Points
- TTE is clinically useful during cardiac arrests
- Watch your timing—using POCUS during rhythm checks can lead to significant delays between compressions.
- Place the transducer on the chest at least 5-15 seconds before the rhythm check in order to minimize the time spent acquiring the appropriate cardiac window.
- Evaluate for one finding at a time! It is difficult to assess for each etiology of cardiac arrest in a single rhythm check.
- Have a backup method for knowing when 10 seconds have elapsed and chest compressions must resume.
- Save the clips as you acquire them, then watch these clips only after compressions resume.
Resources/Further Reading
- Gaspari R., Weekes A., Adhikari S., et al: Emergency department point-of-care ultrasound in out-of-hospital and in-ED cardiac arrest. Resuscitation 2016; 109: pp. 33-39
- Breitkreutz R., Price S., Steiger H.V., et al: Focused echocardiographic evaluation in life support and peri-resuscitation of emergency patients: a prospective trial. Resuscitation 2010; 81: pp. 1527-1533
- Blyth L., Atkinson P., Gadd K., et al: Bedside focused echocardiography as predictor of survival in cardiac arrest patients: a systematic review. Acad Emerg Med 2012; 19: pp. 1119-1126
- Niendorff DF, Rassias AJ, Palac R, Beach ML, Costa S, Greenberg M. Rapid cardiac ultrasound of inpatients suffering PEA arrest performed by nonexpert sonographers. Resuscitation 2005;67:81–7.
- Chardoli M, Heidari F, Rabiee H, Sharif-Alhoseini M, Shokoohi H, Rahimi-Movaghar V. Echocardiography integrated ACLS protocol versus conventional cardiopulmonary resuscitation in patients with pulseless electrical activity cardiac arrest. Chin J Traumatol 2012; 15: 284–7.
- Aagaard, R. Granfeldt, A, Botker, M. Mygind-Klausen, T. Kirkegaard, H. Lofgren, B. The Right Ventricle is Dilated During Resuscitation From Cardiac Arrest Caused by Hypovolemia: A Porcine Ultrasound Study. Critical Care Medicine 2017; 20: 1-8
- Link M, Berkow L, Kudenchuk P, Halperin H, Hess E, Moitra V, et al. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015; 132: S444-64.
- Meaney P, Bobrow B, Mancini M, Christenson J, de Caen A, Bhanji F, et al. Cardiopulmonary Resuscitation Quality: Improving Cardiac Resuscitation Outcomes Both Inside and Outside the Hospital: A Consensus Statement from the American Heart Association. Circulation 2014; 128: 417-35
- CEP Board of Directors : Guidelines for the use of transesophageal echocardiography (TEE) in the ED for cardiac arrest. Ann Emerg Med 2017; 70: 442-445
- Fair J, Mallin M, Mallemat H, et al. Transesophageal Echocardiography: Guidelines for Point-of-Care Applications in Cardiac Arrest Resuscitation. Ann Emerg Med. 2018; 71: 201-207.
- Huis in ‘t Veld M, Allison M, Bostick D, Fisher K, Goloubeva O, Witting M, Winters M. Ultrasound Use During Cardiopulmonary Resuscitation is Associated with Delays in Chest Compressions. Resuscitation 2017; 119: 95-98.
- Clattenburg E, Wroe P, Brown S, Garner K, Losonczy L, Singh A, Nagdev A. Point-of-care Ultrasound Use in Patients with Cardiac Arrest is Associated Prolonged Cardiopulmonary Resuscitation puases: A prospective Cohort Study. Resuscitation 2018; 122: 65-68
- Clattenburg E, Wroe P, Gardner K, Schultz C, Gelber J, Singh A, Nagdev A. Implementation of the Cardiac Arrest Sonographic Assessment (CASA) Protocol for Patients with Cardiac Arrest is Associated with Shorter CPR Pulse Checks. Resucitation 2018; 131: 69-73.
- Aagarrd R, Lofgren B, Grofte T, Sloth E, Nielsen R, Frederiksen C, Granfeldt A, Botker M. Timing of Focused Cardiac Ultrasound During Advanced Life Support – A Prospective Clinical Study. Resuscitation 2018; 124: 126-131
- Gardner K, Clattenburg E, Wroe P, Singh A, Mantuani D, Nagdev A. The Cardiac Arrest Sonographic Assessment (CASA) Exam – A Standardized Approach to the Use of Ultrasound in PEA.

5 thoughts on “US Probe: Preventing Harmful Delays with POCUS During Cardiac Arrest”