Journal Feed Weekly Wrap-Up
- Jun 27th, 2020
- Clay Smith
- categories:
We always work hard, but we may not have time to read through a bunch of journals. It’s time to learn smarter.
Originally published at JournalFeed, a site that provides daily or weekly literature updates.
Follow Dr. Clay Smith at @spoonfedEM, and sign up for email updates here.
#1: Haloperidol for Headache – THE HA Study RCT
Spoon Feed
In patients aged 15 to 55 years with benign headaches, low dose IV haloperidol (2.5mg) improved pain in as little as 30 minutes without significant adverse events such as QT prolongation.
Why does this matter?
Headaches are the fifth leading cause of patients presenting to the emergency department. An estimated 3.8 million annual visits account for patients over 15 years of age. While workup in the emergency department for benign headaches is usually minimal, the length of stay tends to be greater than 2 hours as we await patients to report an improvement in pain satisfactory for discharge.
Haldol for headache? Are you saying this is just all in my head?
This was a randomized, double-blind, placebo-controlled trial performed in a single ED comparing administration of 2.5mg IV haloperidol vs placebo (0.9% NaCl) in 118 patient treated for acute, benign headache. The primary endpoint for this study was pain reduction at 60 minutes. However, a statistically significant improvement in pain was also reported as little as 30 minutes in the haloperidol group (pain scores were documented at 0, 30, 60 and 90 minutes, and at discharge); 34.5% of patients in the treatment group reported >50% reduction in pain at 30 minutes and 63.8% of patients in the treatment group reported >50% reduction in pain at 60 minutes. Notably, 58.6% of patients treated with haloperidol had resolution of their headache prior to discharge. If patients did not have at least a 50% reduction in visual analog scale (VAS) at the 60-minute interval, rescue medications were administered (IV ketorolac or IV metoclopramide). Only 18 patients (31%) in the haloperidol group required rescue therapy as opposed to 48 patients (78.3%) of the placebo group. At 24-hours post discharge, fewer patients treated with haloperidol had return of symptoms, and approximately 75% requested haloperidol in the future! Although this was a small study, the data is promising and haloperidol could certainly be incorporated into our treatment of benign headaches. We could use this in conjunction with other commonly used treatments such as acetaminophen, ketorolac, and IV fluid, which would allow us to avoid potentially sedating medications such as prochlorperazine (somnolence was not observed in the treatment group).
Important exclusion criteria: abnormal blood pressure (>200/100mmHg), sudden or rapid onset, fever, pregnancy, acute trauma, history of brain mass, history of stroke, history of abnormal brain anatomy, QT>450ms, abnormal neurologic exam, GCS<15, or any other clinical concern warranting head CT.
Source
Treatment of Headache in the Emergency Department: Haloperidol in the Acute Setting (THE-HA Study): A Randomized Clinical Trial. J Emerg Med. 2020 May 10;S0736-4679(20)30349-8. doi: 10.1016/j.jemermed.2020.04.018. Online ahead of print.
Open in Read by QxMD
#2: Aortic Dissection Detection Risk Score – Is It Clinically Useful?
Spoon Feed
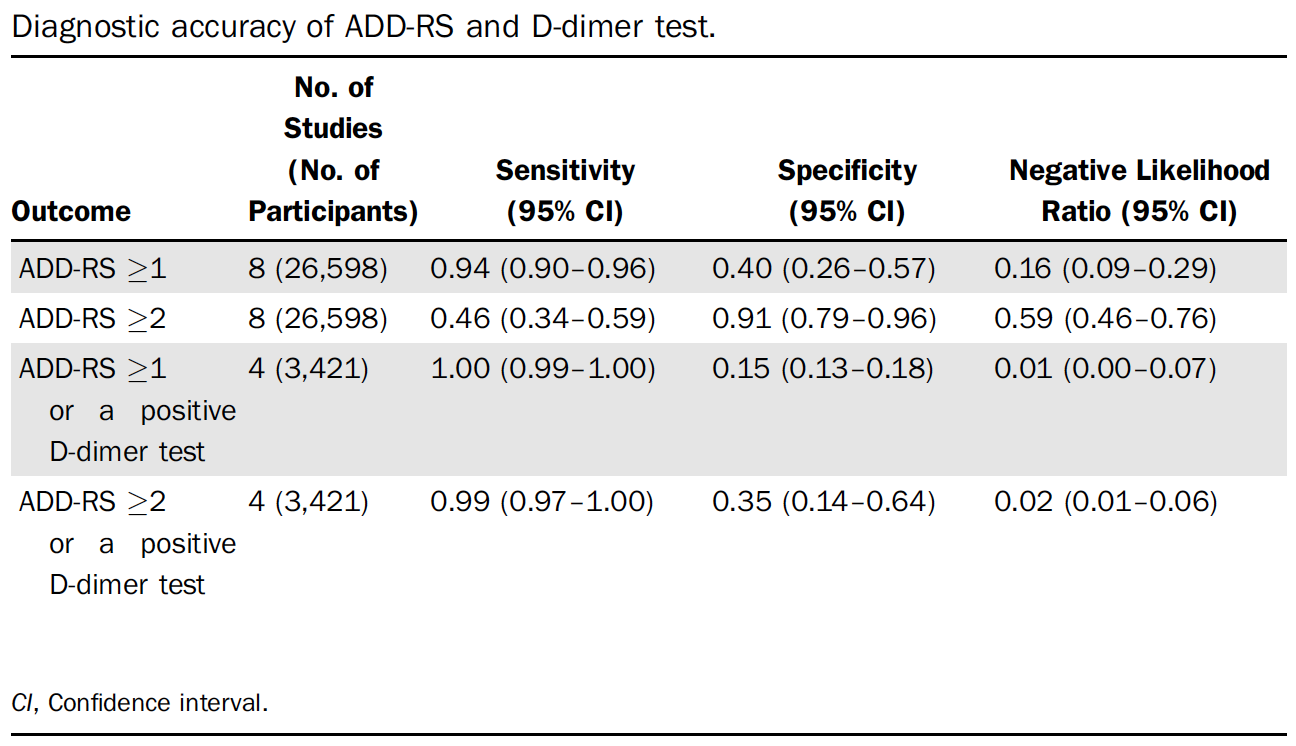
The aortic dissection detection risk score (ADD-RS) is sensitive using a score of ≥1. Adding a D-dimer to the score improves sensitivity even more but at the cost of a slightly lower specificity.
Why does this matter?
Aortic dissection is a “can’t miss” diagnosis. But it is also bad stewardship to scan every person who complains of chest or abdominal pain. Is there a way to decide when to scan or not?
There is always a cost
This was a brief synopsis of a systematic review published elsewhere*. This was a systematic review of 9 studies, 8 of which were retrospective. They found the sensitivity of an ADD-RS ≥1 was 94%; specificity 40%. Just to be clear, this means a score of zero. Adding a D-dimer in addition to a ADD-RS ≥2* improved sensitivity to 99% but dropped specificity to 35%. See Table. Here is my take home. If you practice in a location with a low prevalence of aortic dissection and have a negative ADD-RS and D-dimer, you can stop and not perform CTA. Of course, you still need to workup other etiologies of chest or abdominal pain as usual, but it is very unlikely the pain is due to dissection.
*Amended 6/24/20
From cited article
Source
What Is the Accuracy of the Aortic Dissection Detection Risk Score? Ann Emerg Med. 2020 May 14;S0196-0644(20)30255-9. doi: 10.1016/j.annemergmed.2020.04.005. Online ahead of print.
Open in Read by QxMD
*This Annals of EM Systematic Review Snapshot was a brief synopsis of this original article.
Tsutsumi Y, Tsujimoto Y, Takahashi S, et al. Accuracy of aortic dissection detection risk score alone or with D-dimer: a systematic review and metaanalysis. Eur Heart J Acute Cardiovasc Care. 2020; https:// doi.org/10.1177/2048872620901831.
#3: Major Consensus Statement on IV Contrast Nephropathy
Spoon Feed
This is a summary of the major American College of Radiology/National Kidney Foundation (ACR/NKF) consensus statements.
Why does this matter?
If you work in Emergency Medicine, there is an inevitable phone call (or multiple calls in my case) from the radiology tech to tell you that the CT scan that you ordered three hours ago cannot be done because of the patient’s GFR. After you are finished swearing under your breath, you can now rest easier knowing that the ACR sort of affirms what you have been telling people all along.
Now can you please scan my patient?!
-
Do not withhold contrasted CT exams based on contrast-induced acute kidney injury (CI-AKI) risk if there is no suitable alternative.
-
High-risk patients are those with recent AKI, eGFR < 30 mL/min/1.73 m2, which includes non-anuric patients undergoing dialysis.
-
Perform kidney function screening on patients with a history of kidney disease.
-
There are no clinically relevant differences in CI-AKI risk between iso-osmolality and low-osmolality iodinated contrast.
-
Give IV normal saline prophylaxis to patients not undergoing dialysis who have eGFR < 30 or AKI. You can consider giving this prophylaxis at eGFR of 30-44 if they have high-risk circumstances.
-
Prophylaxis is not indicated for patients with eGFR > 45.
-
Kidney replacement therapy should not be initiated or adjusted solely based on contrast administration.
-
A solitary kidney is not an independent risk factor for CI-AKI.
-
In high-risk patients, use the minimum amount of contrast necessary.
-
Withhold nephrotoxic medications in patients with AKI or eGFR < 30.
Source
Use of Intravenous Iodinated Contrast Media in Patients With Kidney Disease: Consensus Statements From the American College of Radiology and the National Kidney Foundation. Radiology. 2020 Mar;294(3):660-668. doi: 10.1148/radiol.2019192094. Epub 2020 Jan 21.
Open in Read by QxMD
