Journal Feed Weekly Wrap-Up
- May 15th, 2021
- Clay Smith
- categories:
#1: Early Head-to-Pelvis CT for OHCA
Spoon Feed
Obtaining an expedited CT head-to-pelvis after resuscitation from idiopathic out-of-hospital circulatory arrest (OHCA) appears to be safe and may help identify and rule out critical life-threatening diagnoses and change clinical management.
Why does this matter?
Many times, we are simply told “CPR in progress via EMS. ETA 5 minutes.” It’s our job to make sure we assess for reversible causes and perform our job as the experts of resuscitation. However, it is often difficult to obtain a good history and determine the exact cause of cardiac arrest once the patient is resuscitated and return of spontaneous circulation (ROSC) is achieved. Could an early head-to-pelvis CT assist with our workup and safely identify potential causes of OHCA?
“Just send ‘em to the donut of truth”
This was a prospective, observational cohort study of 104 patients who had OHCA without obvious cause (idiopathic OHCA) status post ROSC. These patients were enrolled in an early “sudden-death” CT (SDCT) protocol within 6 hours of hospital arrival that included a non-contrast CT head, an electrocardiogram-gated cardiac and thoracic CT angiogram, and a non-gated venous-phase abdominopelvic CT angiogram. Of note, patients that needed emergent cardiac catheterization or were too hemodynamically unstable for SDCT were excluded from this cohort.
Based on this study, scans occurred within 1.9 +/- 1.0 h of hospital arrival and identified 39% (41/104) of all causes of OHCA and 95% (39/41) of all causes potentially identifiable by SDCT. SDCT was also useful for identifying life-threatening complications of the resuscitation in 16% of patients such as pneumothorax/thoracic organ injury (n=8) and complications from a liver or spleen laceration (n=6). In addition, in 13% of cases, SDCT determined causes of OHCA that would not have been identified by standard of care without CT scanning. Overall, 28% of patients developed acute kidney injury (AKI), but only 1 patient required initiation of dialysis. Of note, transient renal dysfunction is very common after OHCA (40-50%) and so the incidence of AKI in the study may not be related to iodinated contrast exposure from SDCT. No other significant safety outcomes were noted.
What I take from this study is that early head-to-pelvis CT appears to be a safe procedure that can rapidly identify potential causes of OHCA and could significantly change a patient’s management in the post-ROSC scenario.
Edited and Peer Reviewed by Sam Parnell
Source
Early head-to-pelvis computed tomography in out-of-hospital circulatory arrest without obvious etiology. Acad Emerg Med. 2021 Apr;28(4):394-403. doi: 10.1111/acem.14228. Epub 2021 Mar 24.
#2: New Treatment for PID – Should We Add Metronidazole?
Spoon Feed
Adding metronidazole to the current IDSA regimen of ceftriaxone (CTX) and doxycycline for outpatient pelvic inflammatory disease (PID) treatment is generally well tolerated and associated with less-frequent recovery of anaerobic organisms and improved clinical response compared to CTX and doxy.
Why does this matter?
PID is a spectrum of disease that, left untreated, can predispose women to chronic pelvic pain, ectopic pregnancy, abscess formation, sepsis, and infertility. Previous research has found an association between the presence of anaerobic organisms following treatment of pelvic infections and subsequent infectious morbidity when anti-anaerobic therapy has not been administered. These authors sought to identify:
-
Primarily – if adding metronidazole to IDSA recommended outpatient treatment led to a clinical improvement at a 3-day follow up;
-
Secondarily – if anaerobes could be isolated in the endometrium at 30 days following treatment.
Next time you treat a patient with PID why not cef-TRI-axone doxy-nidazole….
This was a randomized, double-blind, placebo-controlled trial that compared current IDSA PID guidelines (a single IM shot of 250mg CTX [now 500mg] and doxy 100mg BID for 14 days) to current treatment PLUS metronidazole 500mg BID or a matching placebo for 14 days. They enrolled a total of 233 women over a 4+ year period at an academic ED and county health STD clinic in Pittsburgh, PA. The researchers followed these women for 30 days, checking a clinical pain score at time of enrollment, 3 days following treatment, and a clinical cure (as defined by >70% improvement in tenderness score) at the 30-day mark. They also measured the presence of anaerobic organisms in the endometrium at 30 days following treatment.
There was no difference in the primary outcome of clinical improvement at day 3. While only 184 (79%) women continued all the study medication (taking >75% of prescribed medication), patients taking metronidazole were less likely to have pelvic organ tenderness a month after enrollment than those who received placebo (9% vs 20%, P=0.037). They also found that BV and Trich were more effectively treated, and the metronidazole group had fewer follow-up endometrial cultures positive for anaerobes (8% vs 21%, P< .05). Lastly, there was no significant difference in adverse events (89.7% vs 80.3%, P = .07), though the metronidazole group did have a higher rate of vulvovaginal candidiasis (15.5% vs 6%, P=.02). GI complaints were similar among the two groups.
Overall, this study, while small in total sample size, supports the routine use of metronidazole with CTX and doxy for the treatment of women with PID and should serve to inform future treatment guidelines.
Source
A Randomized Controlled Trial of Ceftriaxone and Doxycycline, With or Without Metronidazole, for the Treatment of Acute Pelvic Inflammatory Disease. Clinical Infectious Diseases, 2020 72(7), 1181–1189. https://doi.org/10.1093/cid/ciaa101.
Spoon Feed
Point of care ultrasound (POCUS) provides safer, more accurate, and more efficient patient care for the diagnosis and management of peritonsillar abscess (PTA).
Why does this matter?
Common physical exam findings of a PTA include a “hot potato” voice, pharyngeal erythema, and asymmetric edema, causing deviation of the uvula to the contralateral side. Despite these classic findings, the physical exam only has a sensitivity of 78% and a specificity of 50%, and if a patient has trismus, this may be worse. Conventional diagnosis is made using physical exam and/or computed tomography (CT) of the neck, and management involves blind, landmark-based aspiration or I&D. The traditional diagnosis and management of PTAs puts your patients at increased risk for complications and exposes them to radiation.
Don’t play hot potato with your patient’s PTA when you have POCUS
The authors did a retrospective cohort study on the diagnosis and management of patients who presented to the ED with PTA. They reviewed two cohorts of patients: cohort one presented between January 2007 and December 2008 (48 patients), and cohort two presented between January 2013 and December 2014 (114 patients). The data from these cohorts was further divided into patients whose diagnosis and management included POCUS vs. no ultrasound (NUS).
The primary endpoint was POCUS utilization, and the secondary endpoints included: successful aspiration, otolaryngology (ENT) consultation, computed tomography (CT) imaging, unscheduled return visits, and length of stay (LOS). The Fisher’s exact and t-tests analyzed data.
Twelve patients in cohort 1 had a POCUS (25%) vs. 89 in cohort 2 (78%) (p < 0.0001; odds ratio [OR] 0.09 (95% confidence interval [CI] 0.04–0.20). The secondary endpoints of the combined cohorts are listed in study table 3.
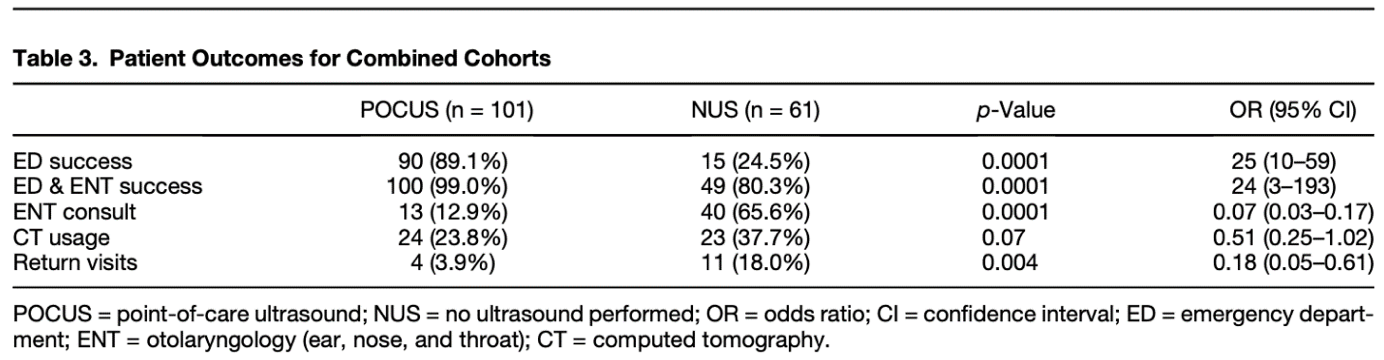
From cited article
Use of POCUS for PTAs has significantly increased since 2007 at the study institution. The data also demonstrates that it improves aspiration success and decreases consultations, radiation exposure, return visits, and ED LOS. For your next hot potato, consider using POCUS to help cool it off.
Source
Evidence-Based Medicine Improves the Emergent Management of Peritonsillar Abscesses Using Point-of-Care Ultrasound. J Emerg Med. 2020 Nov;59(5):693-698. doi: 10.1016/j.jemermed.2020.06.030. Epub 2020 Aug 19.
