Author: Jamie Santistevan, MD (@jamie_rae_EMdoc – EM Physician, Presbyterian Hospital, Albuquerque, NM) // Edited by: Manpreet Singh, MD (@MPrizzleER – Assistant Professor of Emergency Medicine / Department of Emergency Medicine – Harbor-UCLA Medical Center) and Brit Long (@long_brit – EM Attending Physician, San Antonio, TX)
Welcome to this edition of ECG Pointers, an emDOCs series designed to give you high yield tips about ECGs to keep your interpretation skills sharp. For a deeper dive on ECGs, we will include links to other great ECG FOAMed!
The Case:
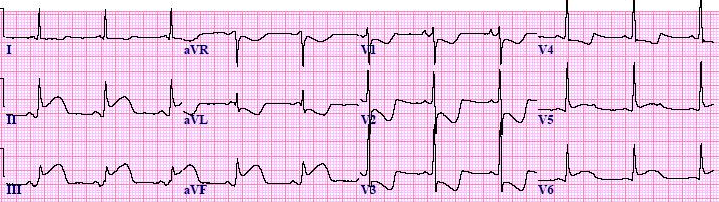
A 35-year-old man presents with sub-sternal chest pain that began during an exercise class 30 minutes prior to arrival.

There is sinus tachycardia, with deep ST depression in V1-V3. There are very large – waves in V2 and V3 such that the R-waves are smaller in V4-6 (abnormal R-wave progression). There may be a hint of ST elevation in lead III with ST depression in I and aVL.
Posterior STEMI:
Each group of leads on an ECG has anatomical significance. Leads V1-3 are overlying the anterior wall of the heart. Given their placement, they are indirectly examining the posterior wall too. Therefore ST-depression in the anterior leads may be confused for anterior wall ischemia, and a posterior STEMI might not be recognized. Posterior wall MI is most commonly associated with an inferior or lateral STEMI (occurring 15-20% percent of the time). However, isolated posterior MI, while less common (3-11% of infarcts2), is important to recognize as it is also an indication for reperfusion and can be missed by the ECG reader.
ECG findings:
- The ECG in posterior STEMI is first characterized by ST-depression in the anterior leads. The ST depression is often deep (>2mm) and flat (horizontal).3
- There will be a large R-wave in V2-3, even bigger than the S-wave.3 Normal R-waves progressively increase in height across the precordial leads. They are small in V1, become larger than the S-wave by V4, and are paired with a small S-wave by V6 (normal R-wave progression). Large R-waves in V2-3 greater than those in V4-6 is an abnormal R-wave balance.
- There are often large and upright anterior T-waves.
- There may be subtle (or overt) signs of an inferior or lateral MI— look for ST elevation in other vascular territories.
- If the anterior leads represent a mirror image of the posterior wall, then the ECG turned upside-down reveals that the tall anterior R-waves become deep posterior Q-waves, the ST-depression becomes ST-elevation, and upright T-wave becomes terminal T-wave inversion. However, you can’t use the upside-down trick to rule out posterior STEMI.

An upside-down mirror image of our patients ECG leads V2 and V3
Posterior extension of inferior or lateral MI:
An isolated posterior MI is less common than the posterior extension of an inferior or lateral MI. Blood supply to the posterior wall in 80-85% of people comes from the right coronary artery (RCA) giving rise to the posterior descending artery (PDA). The remaining 15-20% of hearts are roughly divided between left dominant and codominant. In left dominant hearts, the PDA is supplied by the left circumflex (LCx) or less commonly by the left anterior descending (LAD) coursing around the apex of the heart. In a codominant heart, a single or duplicated PDA is supplied by branches of both the RCA and LAD or LCx. Posterior MI can therefore occur with occlusion of any one of these arteries depending on the patients anatomy. Posterior extension of inferior or lateral infarct indicates a larger area of ischemic myocardium, and these patients are at increased risk of complications related to MI4.
This ECG demonstrates ST elevation in the inferior leads (II, III, and aVF) with reciprocal ST depression in aVL. There is also deep ST depression in the anterior leads (V1-3) with large R-waves in V2-3. This represents an inferior-posterior STEMI. This ECG was originally published at: https://www.healio.com/cardiology/learn-the-heart/blogs/stemi-mi-ecg-pattern
In uncertain cases, a posterior ECG can be obtained by placing posterior leads V7, V8, and V9 below the patients left scapula along the same horizontal plane as V6. At least 0.5mm of ST elevation in one lead indicates posterior STEMI.

Posterior ECG lead placement
Case continued:
The emergency provider recognized this as highly suspicious for posterior STEMI, and posterior leads were obtained.

There is ST-elevation of at least 0.5mm is seen in V7 and V8 posterior leads.
The patient was taken emergently to the cardiac cath lab where he was found to have severe multi-vessel coronary artery disease. The first obtuse marginal branch (OM1) of the left circumflex artery was a large, bifurcated artery, and was 100% occluded with regional wall motion abnormality in this territory. The OM1 was thought to be the artery responsible for the infarct and a stent was placed. Stenting of the LAD was also performed for severe disease (80-90% stenosis). The Troponin I peaked at >40ng/dL, the maximum lab cut-off value. At the time of discharge, the wall motion abnormality had resolved and the patient had normal LV systolic function.
Main ECG pointers for Posterior STEMI:
- Look for deep (>2mm) and horizontal ST-segment depression in the anterior leads and large anterior R-waves (bigger than the S-wave in V2).
- Posterior STEMI often occurs along with an inferior or lateral STEMI, but can also occur in isolation.
- A posterior ECG showing ST elevation of only 0.5mm in is diagnostic for posterior STEMI.
But wait, there’s more ECG FOAMed:
- For a rapid review of posterior MI and several great examples, check out this post from LITFL.
- For discussions on a few cases of isolated posterior STEMI, look HERE from Dr. Smith’s ECG Blog.
- For five ECG patterns you must know, check out the R.E.B.E.L. EM Post.
- How Accurate is the Flipped ECG Trick? Find out from ALiEM.
References/Further Reading:
- Boden E, Kleiger R, Gibson R, Schwartz D, et al. Electrocardiographic evolution of posterior acute myocardial infarction: Importance of early precordial ST-segment depression. Am J Cardiol 1987;59:782-7
- Oraii S, Maleki M, Abbas Tavakolian A, et al. Prevalence and outcome of ST-segment elevation in posterior electrocardiographic leads during acute myocardial infarction. J Electrocardiol 1999;32: 275-8
- Brady W, Erling B, Pollack M, et al. Electrocardiographic manifestations: acute posterior wall myocardial infarction. J Emerg Med 2001;20:391-401
- Matetzky S, Freimark D, Chouraqui P, et al. Significance of ST segment elevations in posterior chest leads (V7 to V9) in patients with acute inferior myocardial infarction: application for thrombolytic therapy. J Am Coll Cardiol 1998;31:506-11






