Today on the emDOCs cast with Brit Long (@long_brit), we start a series on EBM updates for intubation. We cover some background, predicting difficult BVM/intubation/cricothryotomy, physiologic factors associated with peri-intubation decompensation, preoxygenation, and apneic oxygenation.
Episode 127: Intubation EBM Updates Part 1
Background:
- Indications for intubation: airway obstruction (e.g., anaphylaxis, thermal injury, neck trauma), failure of oxygenation or ventilation, and severe obtundation or weakness resulting in inability to protect one’s airway (1-3).
- ED challenges: Patients are critically ill, they have limited respiratory reserve, multiple comorbidities, and external complicating factors (e.g., limited mouth opening, cervical spine injury).
- Goal is first pass success. Failure to pass the endotracheal tube (ETT) on first attempt is associated with a 33% higher likelihood of adverse outcomes (1-12).
What can we use to predict a difficult airway?
- Difficult airways are more common in the ED compared to the OR, and they are more challenging to predict.
- Difficult airway can result in a “can’t ventilate, can’t intubate” scenario, which may lead to brain injury, hemodynamic compromise, death. Overall ETI failure rates are less than 1% of attempts (2,3,9-15).
- Multiple tools available to predict difficult bag-valve-mask (BVM) ventilation, intubation, and cricothyrotomy, which incorporate several anatomic and physiologic features.
- Difficult BMV: MOANS (mask seal, obesity, age, no teeth, and stiffness) and ROMANS.

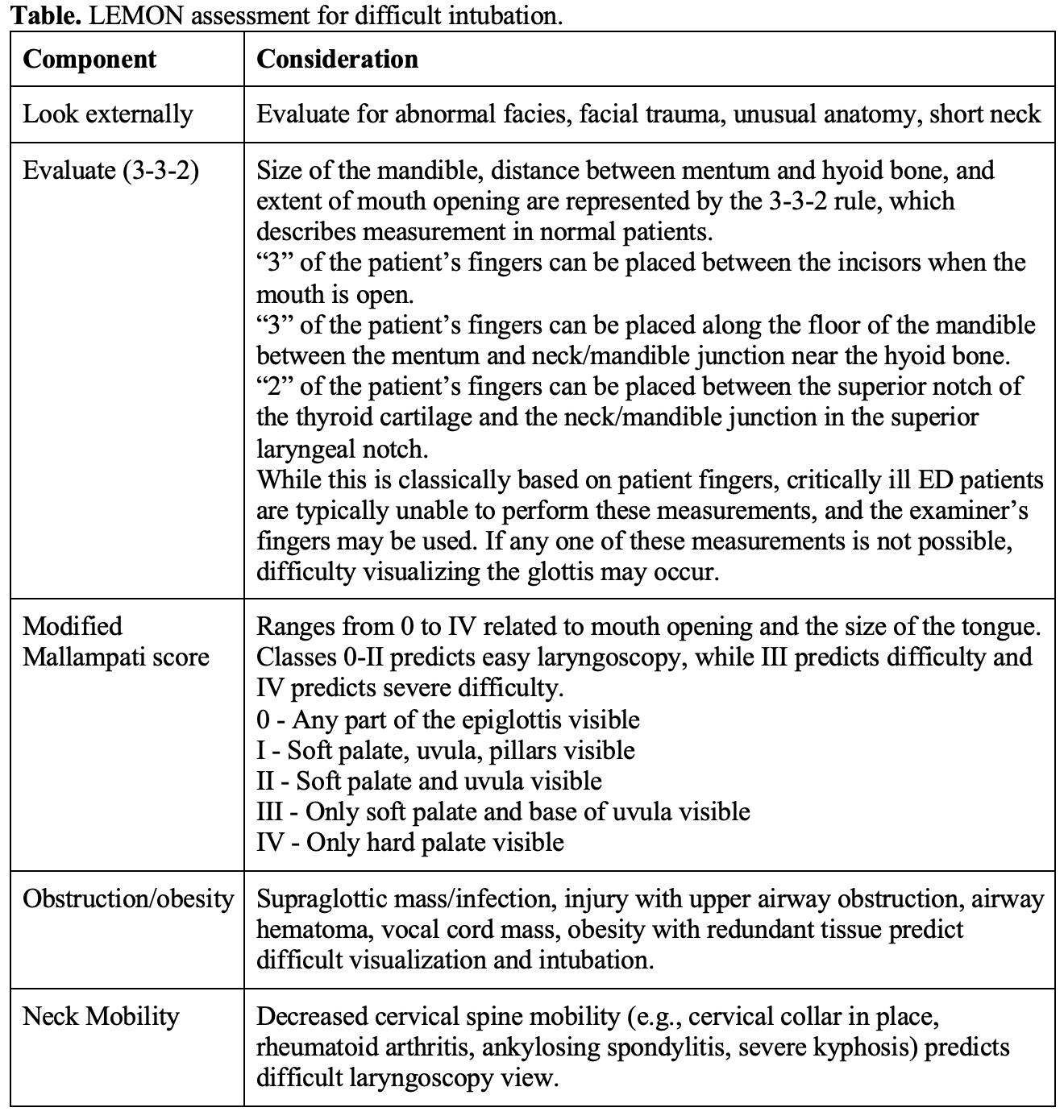
- Difficult intubation: LEMON assessment is a commonly utilized tool to predict difficult intubation).
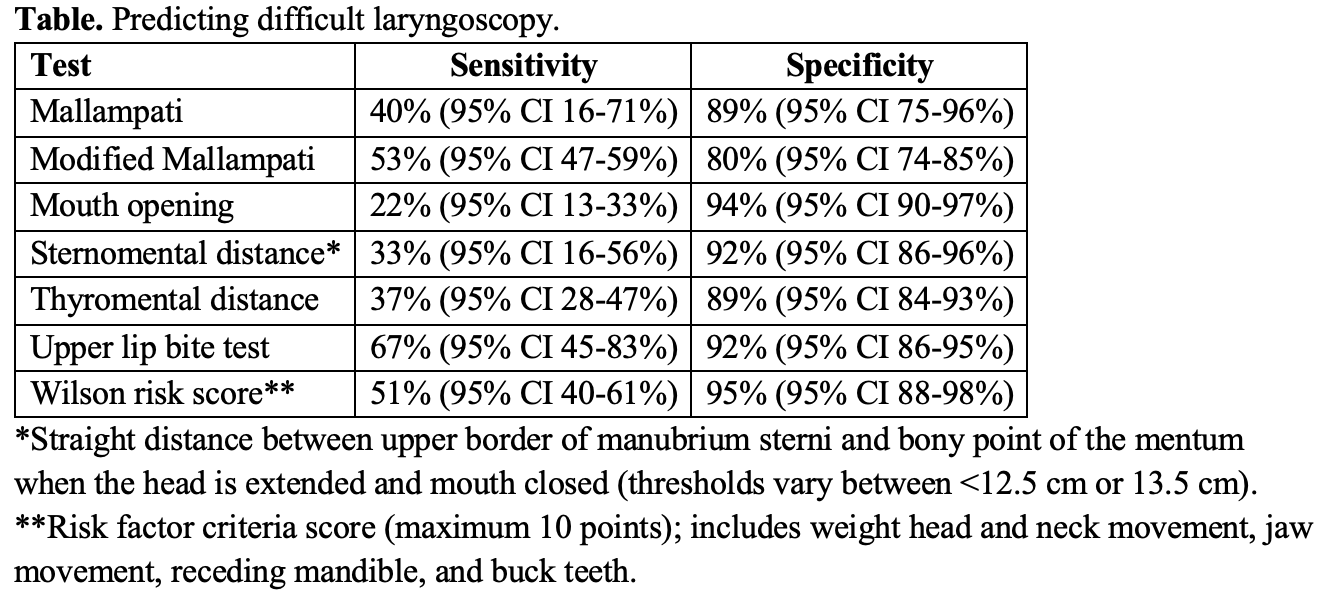
- Difficult laryngoscopy: upper lip bite test is a predictor of difficult laryngoscopy. Have the patient extend their jaw and attempt to cover the upper lip with the lower incisors.
- Meta-analysis of 27 studies found specificity > 85% and sensitivity > 70% with the upper lip bite test for predicting difficult laryngoscopy (34).
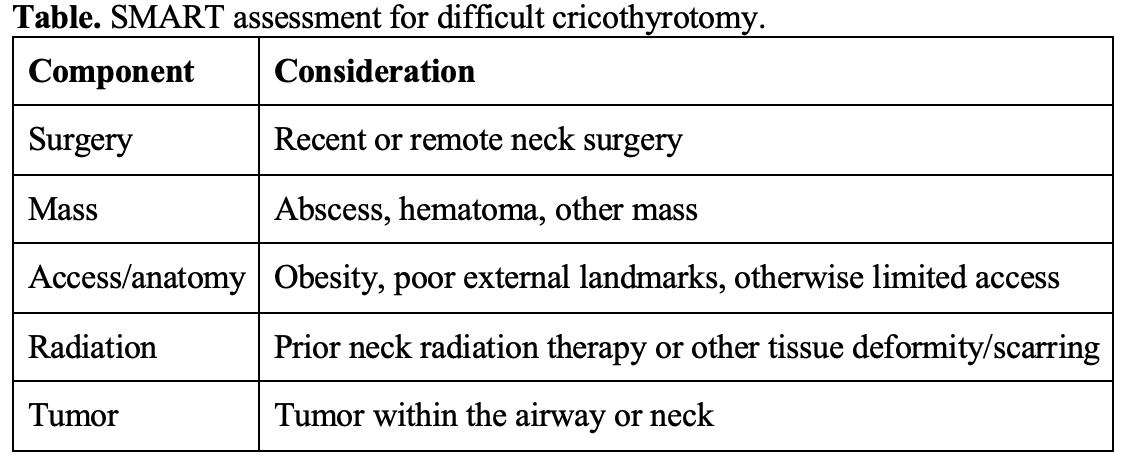
- Difficult cricothyrotomy: The SMART criteria is a tool for predicting difficult cricothyrotomy (35,36).
- 2018 Cochrane review evaluated tools for predicting difficult face mask ventilation, difficult laryngoscopy, and difficult ETI in patients without previously known anatomic abnormalities. Found the Mallampati test, modified Mallampati test, Wilson score, thyromental distance, sternomental distance, mouth opening test, and upper lip bite test had sensitivity 22-67%, specificity 80-93% (30).
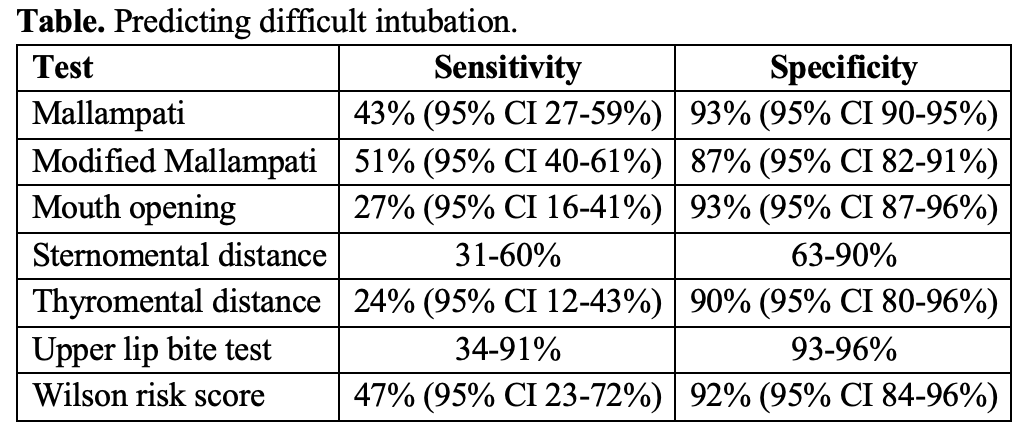
- 2019 systematic review found the upper lip bite, shorter hyomental distance (< 3-5.5 cm), retrognathia (mandible < 9 cm from the angle of the jaw to the tip of the chin), abnormal Wilson score, and modified Mallampati score ≥ 3 to be associated with difficult ETI (25).
- POCUS: distance from the skin to epiglottis (DSE), distance from skin to vocal cord (DSVC), hyomental distance (HMD), and tongue thickness. Sensitivities and specificities between 70-100%, but this is not a routine use for POCUS. May also use POCUS to identify the cricothyroid membrane for cricothyrotomy (43,44).
- Summary: Based on the literature, do not use any single clinical or sonographic tool in isolation. Consider every ED intubation to be difficult and have an airway plan involving multiple approaches. Verbalize plan to team.
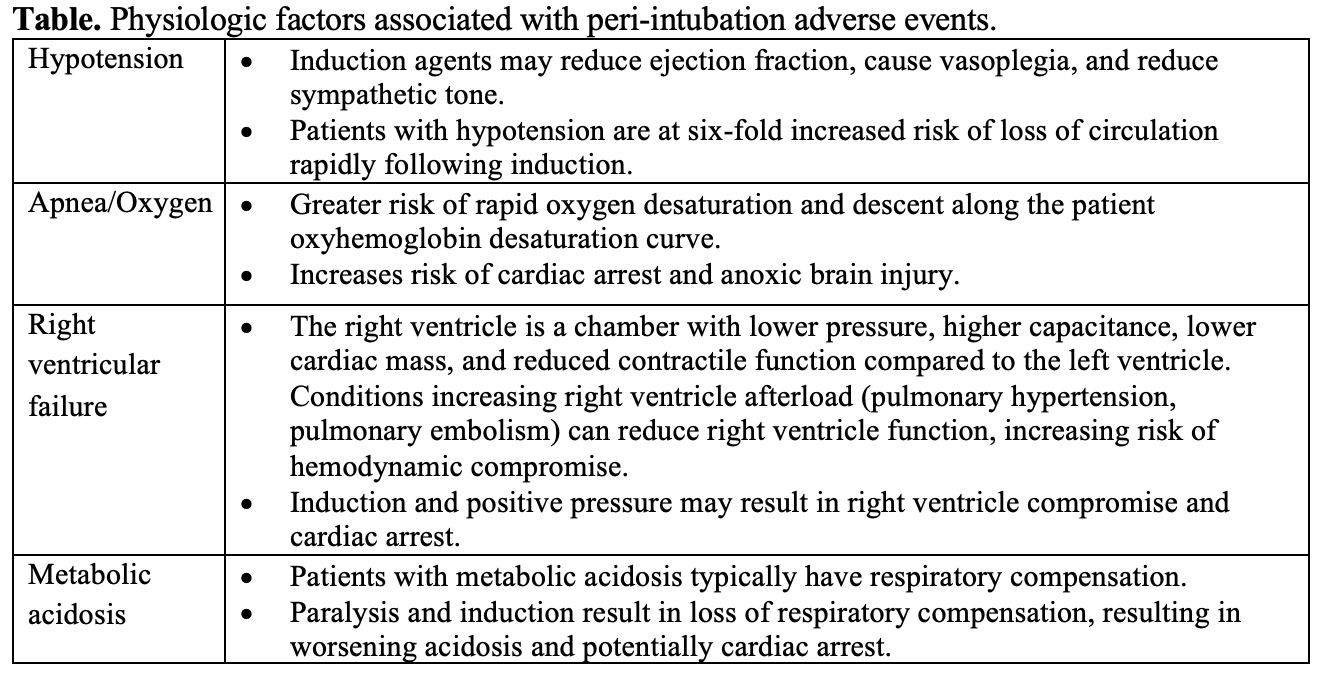
What physiologic factors are associated with peri-intubation adverse events?
- Peri-intubation adverse events: hypoxia, hypotension, and cardiac arrest; occur in up to 17% of ETIs in the ED setting based on a 2023 meta-analysis. Other literature suggests these can occur in up to 45% of intubations performed in critically ill patients (45,46).
- Hypoxia, tachycardia, hypotension before induction and ETI strongly associated with increased risk of peri-intubation adverse events, as are RV failure and metabolic acidosis. (45-50). Other major issues are right ventricular failure and metabolic acidosis (51).
- HARM: hypotension, apnea/oxygen, right ventricular failure, metabolic acidosis.
What’s the evidence behind preoxygenation?
- The peri-intubation period is high risk for hypoxemia. Once the oxygen saturation reaches 88-90%, patients can rapidly desaturate, and that can lead to cardiac arrest (47-50).
- Preoxygenation can prolong the safe apnea period and reduce the risk of desaturation.
- Options: nasal cannula with facemask or BVM with positive end-expiratory pressure (PEEP) valve, high flow nasal cannula (HFNC), or noninvasive positive pressure ventilation (NIPPV) with continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BPAP).
- First option is nasal cannula with a non-rebreather mask at > 15 L/min. Use flush rate for the NRB.
- Second option is HFNC. Provides heated and humidified air, higher flow rates, and is likely more comfortable than nasal cannula alone.
- Final and most effective option is NIPPV with CPAP or BPAP.
- Best means of preoxygenation for critically ill patients, obese patients, those who do not achieve oxygen saturation > 93-95% after 3 minutes or 8 vital capacity breaths with other preoxygenation methods (shunt physiology likely).
- BPAP is more helpful in patients needing ventilatory support or lung recruitment, especially critically ill patients or obesity (49,50,52-54).
- 2024 PREOXI study published in NEJM included 1,301 critically ill adult patients in the ED or intensive care unit (ICU) undergoing intubation (54). Found hypoxemia occurred in 9.1% of patients receiving preoxygenation with noninvasive ventilation for 3 minutes vs. 18.5% in those receiving preoxygenation with facemask; absolute difference of 9.4% and NNT of 11. No difference in aspiration (0.9% vs 1.4%; difference, −0.4%; 95% CI −1.6 to 0.7).
- If using NIPPV, titrate the PEEP to 5-15 cm H2O to maintain an oxygenation saturation > 99%.
- Another option if ventilator for NIPPV is not available is using a nasal cannula with BVM and PEEP valve at flush rate (48,49).
- If the patient has emergent respiratory failure, start supplemental oxygen and intubate. Delaying intubation to set up NIPPV for preoxygenation for these patients can result in cardiac arrest.
- Optimal time for preoxygenation is likely 3 minutes of tidal volume breathing or 8 vital capacity breaths with a high oxygen source.
- Critically ill patients with impending respiratory failure will not be able to perform 8 vital capacity breaths. Instead, administer breaths via BPAP with a mandatory rate or BVM.
- ACEP supports using NIV. Level B recommendation states that when feasible, optimize preoxygenation using noninvasive ventilation (NIV)∗over conventional oxygen therapy (COT) for patients being intubated in the ED.
What’s the evidence behind apneic oxygenation?
- Patients can desaturate due to the absence of gas exchange, even with preoxygenation, following induction and paralysis.
- In healthy preoxygenated patients, safe apnea time of up to 8-9 minutes before desaturation. This is not the typical ED patient, who can desaturate within seconds.
- Several factors associated with increased risk of desaturation: airway occlusion, increased oxygen consumption, pulmonary shunt, critical illness, pregnancy, children, and inadequate preoxygenation (47-49,52,54).
- Apneic oxygenation can reduce the risk of desaturation: patient receives supplemental oxygen throughout induction and the ETI attempt (55-60).
- This can prolong the safe apnea time and reduce the risk of desaturation.
- Alveoli can absorb oxygen at 250 mL/minute without lung expansion or diaphragmatic movements (55-60).
- Keep the patient on the preoxygenation strategy during induction and the initial apneic period.
- Provide breaths during the apneic period with either BPAP or BVM with a rate of at least 10 breaths per minute.
- Once ready for the ETI attempt, remove the BVM or NIPPV mask but the keep a nasal cannula in place at maximum flow rate. May also perform a jaw thrust to keep the airway patent during the apneic period (48,49,54).
- Several studies have evaluated the use of apneic oxygenation, but many limitations with this literature.
- 2023 Cochrane review with 23 RCTs found no difference in severe hypoxemia, first-pass success, and other adverse events (arrhythmia, aspiration, hypotension, oral trauma, pneumonia, and cardiac arrest), with insufficient evidence on any effect on the incidence of hypoxemia (59).
- Major limitation is that most trials focused on patients without severe hypoxemia.
- Guidelines:
- 2023 Society of Critical Care Medicine (SCCM) Clinical Practice guidelines do not routinely recommend apneic oxygenation, unless the laryngoscopy is expected to be challenging and in patients with severe hypoxemia (61).
- European Society for Emergency Medicine states apneic oxygenation should be used whenever possible to prolong safe apnea time (62).
- ACEP provides a level C recommendation supporting apneic oxygenation.
- Apneic oxygenation should likely be used in the ED, especially for patients with limited ability for preoxygenation, or critical illness, thypoxic despite preoxygenation, and anticipating a difficult airway and there may be a prolonged attempt for intubation.
Stay tuned for Part 2, where we cover induction medications, paralytics, VL vs. DL, using the bougie, confirming ETT placement, and post intubation sedation.
References:
- National Hospital Ambulatory Medical Care Survey. 2018 emergency department summary tables; 2018.
- Brown CA 3rd, Bair AE, Pallin DJ, Walls RM; NEAR III Investigators. Techniques, success, and adverse events of emergency department adult intubations. Ann Emerg Med. 2015 Apr;65(4):363-370.e1.
- Brown CA 3rd, Kaji AH, Fantegrossi A, et al; National Emergency Airway Registry (NEAR) Investigators. Video Laryngoscopy Compared to Augmented Direct Laryngoscopy in Adult Emergency Department Tracheal Intubations: A National Emergency Airway Registry (NEAR) Study. Acad Emerg Med. 2020 Feb;27(2):100-108.
- Centers for Disease Control and Prevention. Emergency Department Visits.Available at https://www.cdc.gov/nchs/fastats/emergency-department.htm. Accessed May 28, 2024.
- Xia M, Ma W, Zuo M, et al. Expert consensus on difficult airway assessment. Hepatobiliary Surg Nutr. 2023 Aug 1;12(4):545-566.
- Park L, Zeng I, Brainard A. Systematic review and meta-analysis of first-pass success rates in emergency department intubation: Creating a benchmark for emergency airway care. Emerg Med Australas. 2017 Feb;29(1):40-47.
- Maguire S, Schmitt PR, Sternlicht E, Kofron CM. Endotracheal Intubation of Difficult Airways in Emergency Settings: A Guide for Innovators. Med Devices (Auckl). 2023 Jul 18;16:183-199.
- Kim C, Kang HG, Lim TH, et al. What factors affect the success rate of the first attempt at endotracheal intubation in emergency departments? Emerg Med J. 2013 Nov;30(11):888-92.
- Koh W, Kim H, Kim K, et al Encountering unexpected difficult airway: relationship with the intubation difficulty scale. Korean J Anesthesiol. 2016 Jun;69(3):244-9.
- Jaber S, Amraoui J, Lefrant JY, et al. Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Crit Care Med 2006;34:2355-61.
- Schwartz DE, Matthay MA, Cohen NH. Death and other complications of emergency airway management in critically ill adults. A prospective investigation of 297 tracheal intubations. Anesthesiology 1995;82:367-76.
- Griesdale DE, Bosma TL, Kurth T, et al. Complications of endotracheal intubation in the critically ill. Intensive Care Med 2008;34:1835-42.
- Sakles JC, Douglas MJK, Hypes CD, Patanwala AE, Mosier JM. Management of Patients with Predicted Difficult Airways in an Academic Emergency Department. J Emerg Med. 2017 Aug;53(2):163-171. d
- Martin LD, Mhyre JM, Shanks AM, Tremper KK, Kheterpal S. 3,423 emergency tracheal intubations at a university hospital: airway outcomes and complications. Anesthesiology. 2011 Jan;114(1):42-8.
- Bair AE, Caravelli R, Tyler K, Laurin EG. Feasibility of the preoperative Mallampati airway assessment in emergency department patients. J Emerg Med. 2010 Jun;38(5):677-80.
- Langeron O, Masso E, Huraux C, et al. Prediction of difficult mask ventilation. 2000 May;92(5):1229-36.
- Kheterpal S, Han R, Tremper KK, et al. Incidence and predictors of difficult and impossible mask ventilation. Anesthesiology. 2006 Nov;105(5):885-91.
- Kheterpal S, Martin L, Shanks AM, Tremper KK. Prediction and outcomes of impossible mask ventilation: a review of 50,000 anesthetics. Anesthesiology. 2009 Apr;110(4):891-7.
- Nørskov AK, Wetterslev J, Rosenstock CV, et al; Collaborators. Prediction of difficult mask ventilation using a systematic assessment of risk factors vs. existing practice – a cluster randomised clinical trial in 94,006 patients. Anaesthesia. 2017 Mar;72(3):296-308.
- Moon TS, Fox PE, Somasundaram A, et al. The influence of morbid obesity on difficult intubation and difficult mask ventilation. J Anesth. 2019 Feb;33(1):96-102.
- Lundstrøm LH, Møller AM, Rosenstock C, et al. High body mass index is a weak predictor for difficult and failed tracheal intubation: a cohort study of 91,332 consecutive patients scheduled for direct laryngoscopy registered in the Danish Anesthesia Database. Anesthesiology. 2009 Feb;110(2):266-74.
- Juvin P, Lavaut E, Dupont H, et al. Difficult tracheal intubation is more common in obese than in lean patients. Anesth Analg. 2003 Aug;97(2):595-600.
- Connor CW, Segal S. The importance of subjective facial appearance on the ability of anesthesiologists to predict difficult intubation. Anesth Analg. 2014 Feb;118(2):419-427.
- Naguib M, Scamman FL, O’Sullivan C, et al. Predictive performance of three multivariate difficult tracheal intubation models: a double-blind, case-controlled study. Anesth Analg. 2006 Mar;102(3):818-24.
- Detsky ME, Jivraj N, Adhikari NK, et al. Will This Patient Be Difficult to Intubate?: The Rational Clinical Examination Systematic Review. JAMA. 2019 Feb 5;321(5):493-503.
- Lundstrøm LH, Vester-Andersen M, Møller AM, Charuluxananan S, et al; Danish Anaesthesia Database. Poor prognostic value of the modified Mallampati score: a meta-analysis involving 177 088 patients. Br J Anaesth. 2011 Nov;107(5):659-67.
- Samsoon GL, Young JR. Difficult tracheal intubation: a retrospective study. Anaesthesia. 1987 May;42(5):487-90.
- Mallampati SR, Gatt SP, Gugino LD, et al. A clinical sign to predict difficult tracheal intubation: a prospective study. Can Anaesth Soc J. 1985 Jul;32(4):429-34.
- Lee A, Fan LT, Gin T, et al. A systematic review (meta-analysis) of the accuracy of the Mallampati tests to predict the difficult airway. Anesth Analg. 2006 Jun;102(6):1867-78.
- Roth D, Pace NL, Lee A, et al. Airway physical examination tests for detection of difficult airway management in apparently normal adult patients. Cochrane Database Syst Rev. 2018 May 15;5(5):CD008874.
- Green SM, Roback MG. Is the Mallampati Score Useful for Emergency Department Airway Management or Procedural Sedation? Ann Emerg Med. 2019 Aug;74(2):251-259.
- Crosby ET. Considerations for airway management for cervical spine surgery in adults. Anesthesiol Clin. 2007 Sep;25(3):511-33, ix.
- Crosby ET. Airway management in adults after cervical spine trauma. Anesthesiology. 2006 Jun;104(6):1293-318.
- Faramarzi E, Soleimanpour H, Khan ZH, et al. Upper lip bite test for prediction of difficult airway: A systematic review. Pak J Med Sci. 2018 Jul-Aug;34(4):1019-1023.
- Bair AE, Chima R. The inaccuracy of using landmark techniques for cricothyroid membrane identification: a comparison of three techniques. Acad Emerg Med. 2015 Aug;22(8):908-14.
- Aslani A, Ng SC, Hurley M, et al. Accuracy of identification of the cricothyroid membrane in female subjects using palpation: an observational study. Anesth Analg. 2012 May;114(5):987-92.
- Gottlieb M, O’Brien JR, Ferrigno N, Sundaram T. Point-of-care ultrasound for airway management in the emergency and critical care setting. Clin Exp Emerg Med. 2024 Mar;11(1):22-32.
- Carsetti A, Sorbello M, Adrario E, et al. Airway ultrasound as predictor of difficult direct laryngoscopy: a systematic review and meta-analysis. Anesth Analg 2022; 134:740-50.
- Andruszkiewicz P, Wojtczak J, Sobczyk D, et al. Effectiveness and validity of sonographic upper airway evaluation to predict difficult laryngoscopy. J Ultrasound Med 2016; 35:2243-52.
- Petrisor C, Szabo R, Constantinescu C, et al. Ultrasound-based assessment of hyomental distances in neutral, ramped, and maximum hyperextended positions, and derived ratios, for the prediction of difficult airway in the obese population: a pilot diagnostic accuracy study. Anaesthesiol Intensive Ther 2018; 50:110-6.
- Yadav NK, Rudingwa P, Mishra SK, Pannerselvam S. Ultrasound measurement of anterior neck soft tissue and tongue thickness to predict difficult laryngoscopy: an observational analytical study. Indian J Anaesth 2019; 63:629-34.
- Yao W, Wang B. Can tongue thickness measured by ultrasonography predict difficult tracheal intubation? Br J Anaesth 2017; 118:601-9.
- Alerhand S. Ultrasound for identifying the cricothyroid membrane prior to the anticipated difficult airway. Am J Emerg Med. 2018 Nov;36(11):2078-2084.
- Rai Y, You-Ten E, Zasso F, et al. The role of ultrasound in front-of-neck access for cricothyroid membrane identification: A systematic review. J Crit Care. 2020 Dec;60:161-168.
- Downing J, Yardi I, Ren C, et al. Prevalence of peri-intubation major adverse events among critically ill patients: A systematic review and meta analysis. Am J Emerg Med. 2023 Sep;71:200-216.
- Russotto V, Myatra SN, Laffey JG, et al; INTUBE Study Investigators. Intubation Practices and Adverse Peri-intubation Events in Critically Ill Patients From 29 Countries. JAMA. 2021 Mar 23;325(12):1164-1172.
- Mosier JM, Hypes CD, Sakles JC. Understanding preoxygenation and apneic oxygenation during intubation in the critically ill. Intensive Care Med. 2017;43:226-8.
- Mosier JM, Joshi R, Hypes C, Pacheco G, Valenzuela T, Sakles JC. The Physiologically Difficult Airway. West J Emerg Med. 2015 Dec;16(7):1109-17.
- Weingart SD. Preoxygenation, reoxygenation, and delayed sequence intubation in the emergency department. J Emerg Med. 2011 Jun;40(6):661-7.
- Weingart SD, Levitan RM. Preoxygenation and prevention of desaturation during emergency airway management. Ann Emerg Med. 2012 Mar;59(3):165-75.e1.
- Kostura M, Smalley C, Koyfman A, Long B. Right heart failure: A narrative review for emergency clinicians. Am J Emerg Med. 2022 Aug;58:106-113.
- Gleason JM, Christian BR, Barton ED. Nasal Cannula Apneic Oxygenation Prevents Desaturation During Endotracheal Intubation: An Integrative Literature Review. West J Emerg Med. 2018 Mar;19(2):403-411.
- Futier E, Constantin JM, Pelosi P, et al. Noninvasive ventilation and alveolar recruitment maneuver improve respiratory function during and after intubation of morbidly obese patients: a randomized controlled study. Anesthesiology. 2011 Jun;114(6):1354-63.
- Gibbs KW, Semler MW, Driver BE, et al, for the PREOXI Investigators and the Pragmatic Critical Care Research Group. Noninvasive Ventilation for Preoxygenationduring Emergency Intubation. N Engl J Med. DOI: 10.1056/NEJMoa2313680.
- Binks MJ, Holyoak RS, Melhuish TM, et al. Apnoeic oxygenation during intubation in the intensive care unit: A systematic review and meta-analysis. Heart Lung. 2017 Nov-Dec;46(6):452-457.
- Binks MJ, Holyoak RS, Melhuish TM, et al. Apneic oxygenation during intubation in the emergency department and during retrieval: A systematic review and meta-analysis. Am J Emerg Med. 2017 Oct;35(10):1542-1546.
- Pavlov I, Medrano S, Weingart S. Apneic oxygenation reduces the incidence of hypoxemia during emergency intubation: A systematic review and meta-analysis. Am J Emerg Med. 2017 Aug;35(8):1184-1189.
- White LD, Melhuish TM, White LK, Wallace LA. Apnoeic oxygenation during intubation: a systematic review and meta-analysis. Anaesth Intensive Care. 2017 Jan;45(1):21-27. d
- White LD, Vlok RA, Thang CY, et al. Oxygenation during the apnoeic phase preceding intubation in adults in prehospital, emergency department, intensive care and operating theatre environments. Cochrane Database Syst Rev. 2023 Aug 2;8(8):CD013558.
- Oliveira J E Silva L, Cabrera D, Barrionuevo P, et al. Effectiveness of Apneic Oxygenation During Intubation: A Systematic Review and Meta-Analysis. Ann Emerg Med. 2017 Oct;70(4):483-494.e11. Chua MT, Ng WM, Lu Q, et al. Pre- and apnoeic high-flow oxygenation for rapid sequence intubation in the emergency department (the Pre-AeRATE trial): a multicentre randomised controlled trial. Ann Acad Med Singap 2022; 51:149–160.
- Acquisto NM, Mosier JM, Bittner EA, et al. Society of Critical Care Medicine Clinical Practice Guidelines for Rapid Sequence Intubation in the Critically Ill Adult Patient. Crit Care Med. 2023 Oct 1;51(10):1411-1430.
- Hohenstein C, Merz S, Eppler F, et al; European Society for Emergency Medicine. Emergency airway management: an EUSEM statement with regard to the guidelines of the Society of Critical Care Medicine. Eur J Emerg Med. 2024 Apr 1;31(2):83-85.
- Gottlieb M, Chien N, Long B. Managing Alcohol Withdrawal Syndrome. Ann Emerg Med. 2024 Mar 25:S0196-0644(24)00105-7.
- American College of Emergency Physicians Clinical Policies Subcommittee (Writing Committee) on Airway Management; Godwin SA, Hahn SA, Friedman BW, et al. Clinical Policy: Critical Issues in the Management of Adult Patients Requiring Endotracheal Intubation in the Emergency Department. Ann Emerg Med. 2025 Aug;86(2):e29-e68.
- Long B, Gottlieb M. Emergency medicine updates: Endotracheal intubation. Am J Emerg Med. 2024 Nov;85:108-116.






