Today on the emDOCs cast with Brit Long, MD (@long_brit), we cover tubo-ovarian abscess.
Episode 68: Tuba-Ovarian Abscess
Background:
– TOA is an inflammatory infectious mass including the fallopian tube and ovary. In severe cases it can involve the bowel and bladder.
– TOA most commonly results from ascending infection with STI or vaginal flora, but it may also occur due to a secondary infection from the GI system or pelvic cancer.
– PID is the most common predisposing factor in premenopausal patients. Currently about 2% of PID cases are complicated by TOA.
– TOAs are usually polymicrobial with similar bacteria to those present in uncomplicated PID; however, aerobic, facultative, and anaerobic bacteria can cause TOA. Atypical organisms may affect immunocompromised patients.
– Women between the ages of 15-40 years are most commonly affected.
– Sepsis may occur in 10-20% of patients; TOA may rupture in 15% of cases.
Presentation:
– PID is most common risk factor. Others include presence of IUD, diabetes, recent uterine procedures such as hysteroscopy/endometrial ablation, multiple sexual partners, and immunocompromised states including IBD and HIV.
– Chronic bacterial infection may predispose patients to TOA, with documented TOAs secondary to Brucellosis, Salmonella typhi, and Burkholderia pseudomallei.
– Postmenopausal patients with TOA have a high rate of associated malignancy.
– Lower abdominal pain, chills, fever, vaginal discharge.
- Lower abdominal pain in 89%
- Fever in 50-90%
- Chills in 50%
- Nausea in 26%
- Vaginal discharge in 28%
- Abnormal vaginal bleeding in 21%
– Speculum and bimanual examination may display mucopurulent discharge or cervical motion tenderness. Adnexal/uterine tenderness may suggest TOA but not definitive.
– Consider TOA in those who are acutely ill, have significant abdominal or pelvic tenderness, have an adnexal mass present on examination, or who present after failed therapy for PID.
– Rupture can result in peritonitis and sepsis
Evaluation:
– CBC, electrolytes, inflammatory markers (ESR/CRP), pregnancy testing, STI testing (N. gonorrheae, C. trachomatis). If concern for rupture, obtain blood cultures.
- Leukocytosis may occur
- ESR and CRP sensitivity and specificity are not 100%.
- CRP > 49.3 mg/L in a patient with PID suggests TOA with a sensitivity of 85.4% and a specificity of 93.4%.
- Elevated inflammatory markers are predictive of more severe illness and longer hospital stay
- Procalcitonin has limited utility
– Imaging recommended, including US, CT, or MRI.
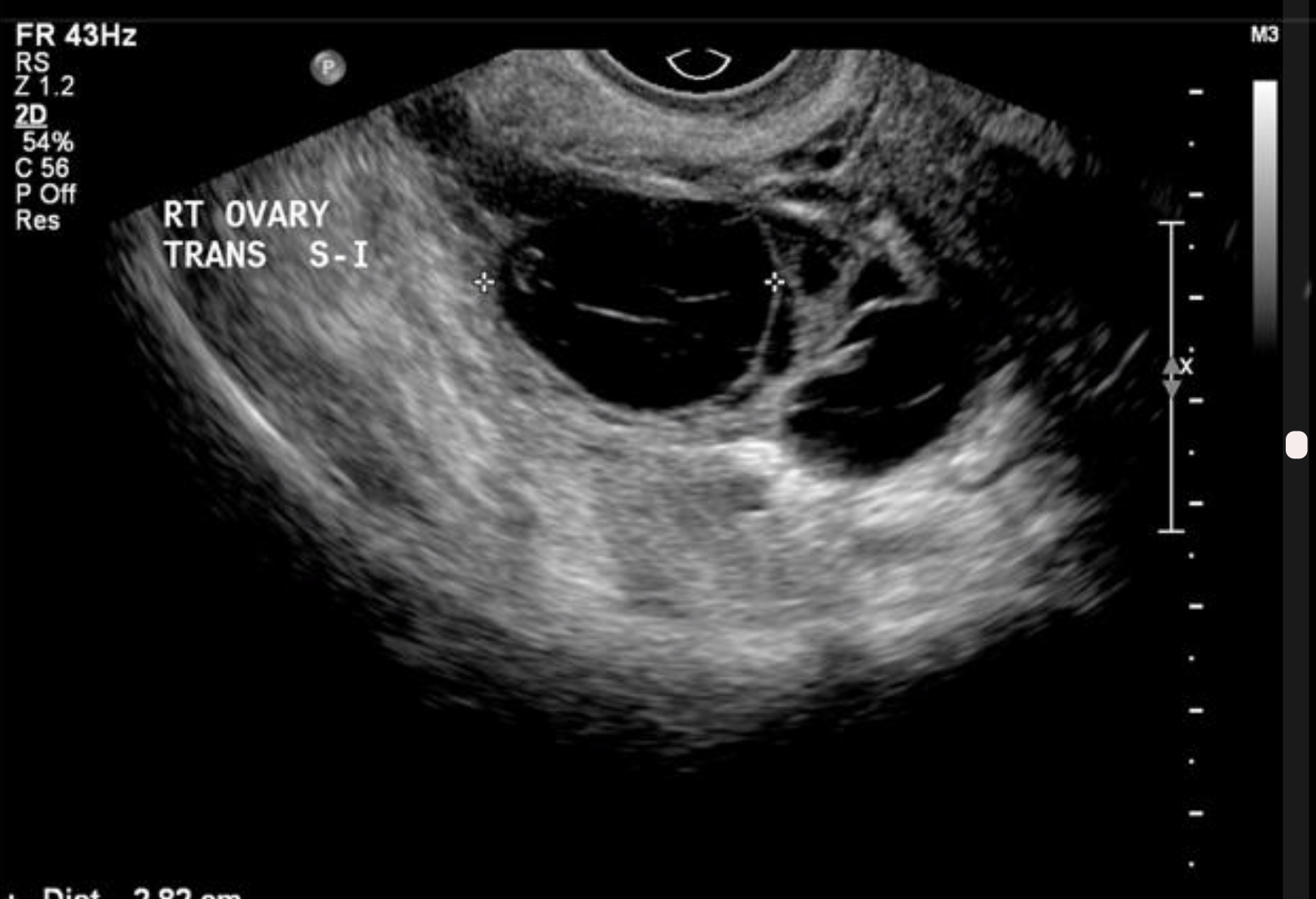
- Transvaginal US is more accurate than transabdominal. Transvaginal US may demonstrate a complex adnexal structure with thick walls and internal echogenicity representing purulent material and cellular debris.
- US sensitivity is 75-90%.
- CT with IV contrast may show fluid collection, enhanced abscess wall, thickened/fluid filled tubes
- CT sensitivity is 78-100%.
- MRI can be used in pregnant patients or if other imaging is inconclusive.

Management:
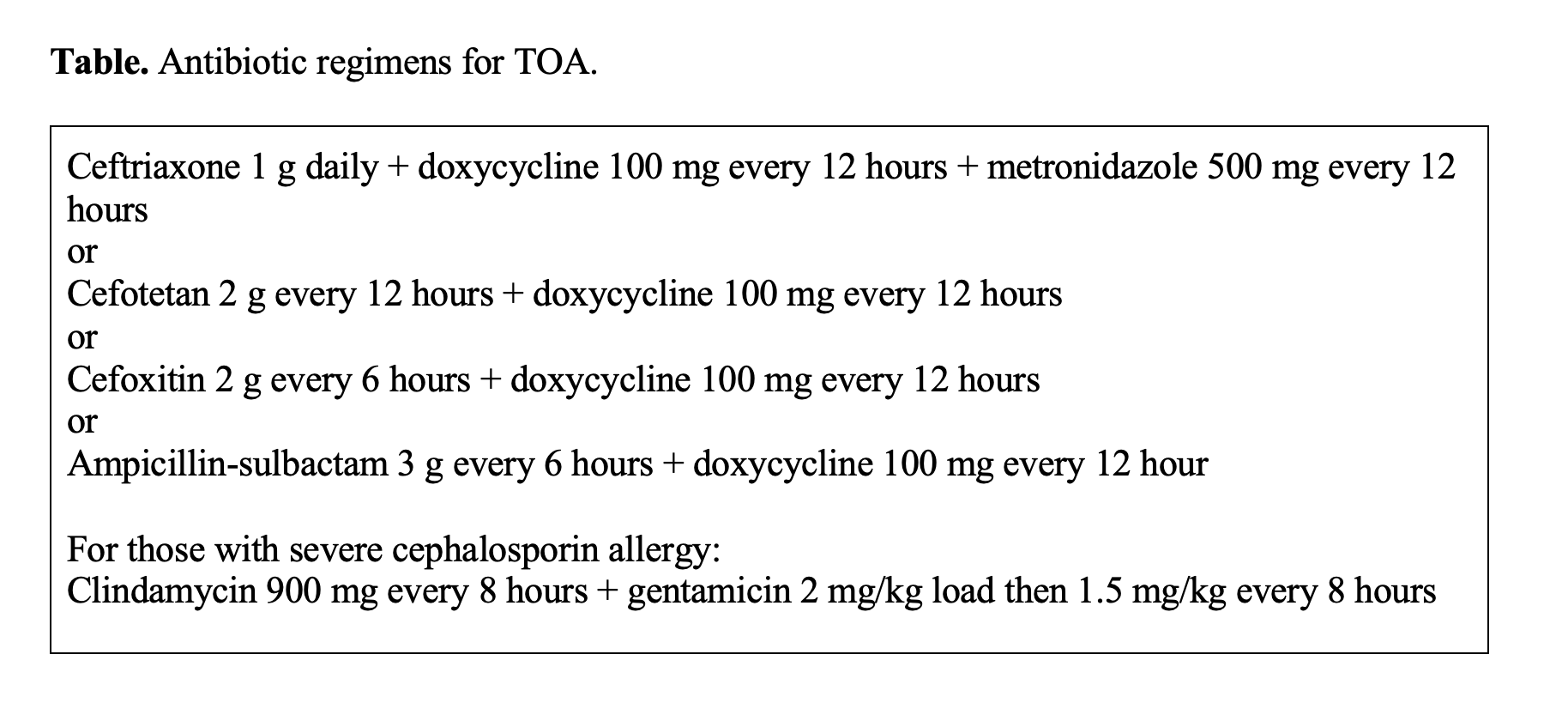
– Consult OBGYN and provide antibiotics.
- Parenteral antibiotics should be rapidly initiated to cover both sexuallytransmitted infections including N. gonorrheae and C. trachomatis as well as polymicrobial GI bacteria including Escherichia coli, Bacterioides fragilis, Prevotella, and anaerobic streptococci species
- IV antibiotics may fail in 25-30% of cases. Risk factors for failure include larger abscess size, bilateral abscesses, fever, older age, parity, and significantly elevated inflammatory markers.
– Drainage of an abscess without rupture can include laparotomy, percutaneous drainage, or colpotomy incision.
– Patients with rupture require emergent operative management.
– Operative intervention often needed for sepsis, rupture, abscess > 5-7 cm.
Special Considerations:
– TOA is rare is pregnancy, but it can lead to adverse outcomes including preterm labor, miscarriage, chorioamnionitis, and fetal or maternal death.
- US or MRI recommended for imaging with OBGYN consultation.
- Delivery may be necessary.
– Intrauterine devices (IUD) are associated with risk of TOA.
- If an IUD is present with a TOA, removal by the OBGYN specialist is often performed; removal is associated with improved short-term outcomes
- There is an association between IUDs and Actinomyces. Tubo-ovarian actinomycosis is associated with the formation of multiple abscesses, granulation tissue, and fibrosis
Key Points:
– Key risk factors to consider for TOA include PID, presence of IUD, multiple sexual partners, DM, and immunocompromised states.
– History and physical examination are non-specific; TOA should be considered in the female patient with lower abdominal pain and fever/chills.
– Elevations in CRP can be a predictor of more severe disease though elevations in inflammatory markers are non-specific.
– US and CT can be used for diagnosis, though CT has higher sensitivity.
– Management includes consultation with the OBGYN specialist and administration of parenteral antibiotics covering sexually transmitted infections and polymicrobial gastrointestinal bacteria.
– Factors associated with failed medical management include larger abscess size or bilateral abscesses, fever, older age, parity, and significantly elevated inflammatory markers on laboratory evaluation.








