Authors: Brit Long, MD (@long_brit) and Manpreet Singh, MD (@MprizzleER) // Reviewed by: Alex Koyfman, MD (@EMHighAK)
COVID-19 is here. While one of our primary goals is to provide the best patient care we can during this pandemic, we must also care for ourselves. This includes ensuring we safely evaluate and manage patients. The recommendations concerning Personal Protective Equipment (PPE) keeps changing. What’s the most up to date information concerning use of PPE in the ED for COVID-19? Lets review together!
Background
To understand PPE, first we need to cover transmission. COVID-19 transmission can occur via droplet transmission and contact transmission primarily, similar to influenza. The risk of transmission via respiratory droplet primary occurs with coughing and is approximately 6 feet.1
Contact is another common means of transmission. This type is often overlooked but vital to prevention. Basically a droplet coughed by a patient lands on a surface. The viral particles persist, depending on the surface. A recent study found viral particles persisted on copper for 4 hours, cardboard for 24 hours, steel for up to 3 days, and plastic for up to 3 days.2
Airborne route transmission may occur with procedures that result in aerosolization. These particles may remain aloft for 3 hours, though this is controversial. Airborne precautions require the use of an N95 mask, compared to a surgical mask. Currently, the World Health Organization (WHO) and Canadian guidelines recommend airborne precautions for procedures that are aerosol-generating. These include nebulizer therapy, endotracheal intubation, noninvasive positive pressure ventilation (NIPPV), high flow nasal cannula (HFNC), CPR, bag-mask ventilation, cricothyrotomy or tracheostomy, and bronchoscopy. While the CDC previously recommended using airborne precautions for all patients with suspected COVID-19, currently providers caring for patients not undergoing an aerosol-generating procedure may use droplet precautions.3
Prevention
With these points in mind, let’s move to prevention. The first goal is hand hygiene, whether washing with soap and water for 20 seconds or alcohol-based hand sanitizer (60-95% alcohol). Personally, we recommend you remove any ring, jewelry and watch before working clinically.
The face, including eyes, nose, and mouth, should not be touched. While this is extremely difficult, wearing a mask may assist you in remembering not to touch the face.
Cleaning of environmental surfaces on a routine basis, including medical equipment, with a 70% ethanol or 0.5% sodium hypochlorite solution is recommended.
Limit the providers entering the room, and also try to limit contact with the patient. One provider who is able to assess the patient, perform a history and exam, and test if needed is recommended. Speaking through a glass door or using a phone to obtain a history can limit exposure.
Masks
From JAMA Network
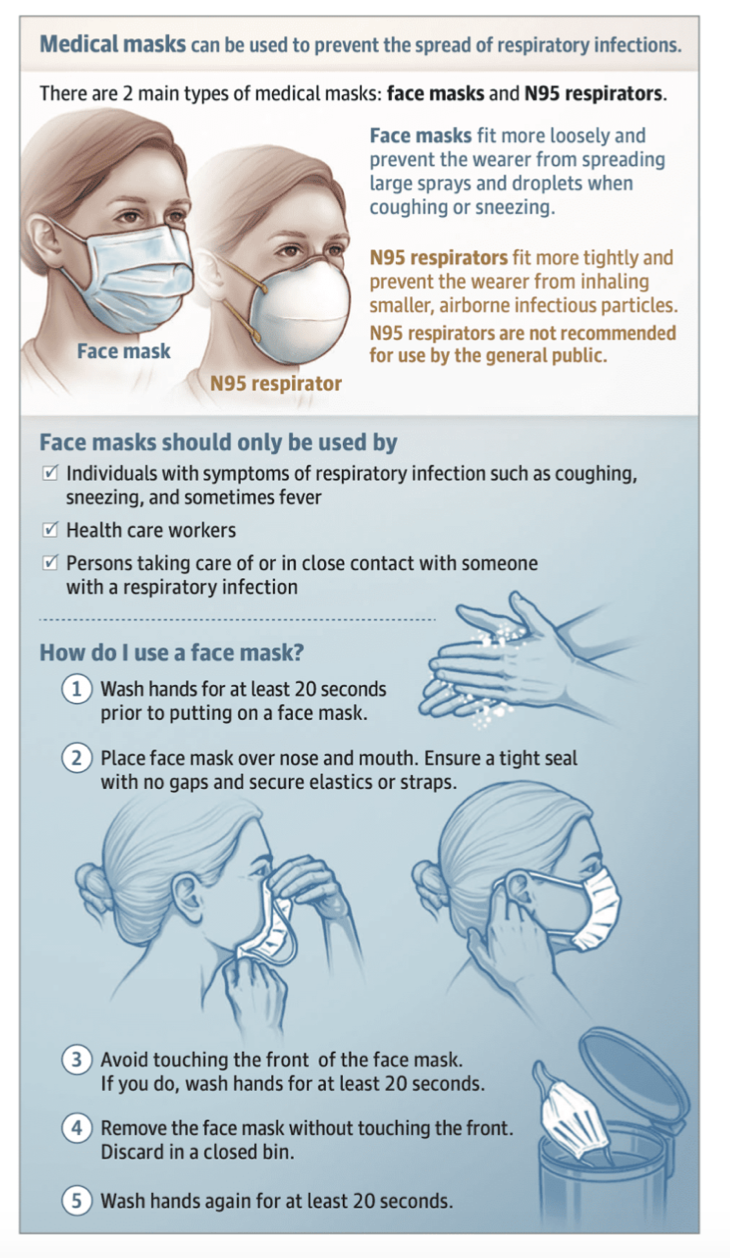
Surgical/Medical Mask
A surgical mask is loose fitting mask that should be worn by the patient and provider caring for the patient (not performing an aerosol-generating procedure).
Unfortunately there have been significant shortages in masks, both surgical and N95. A recent study evaluated medical masks, cloth masks, and standard practice. Authors found cloth masks were associated with higher rates of infection (cloth mask 7.8% vs. medical mask 4.8% for clinical respiratory infection, cloth mask 2.3% vs. medical mas 0.2% for influenza like illness, and cloth mask 5.4% vs. medical mask 3.3% for laboratory confirmed viral infection).4
Respirator Mask
A N95 mask is tight fitting that prevents inhalation of smaller particles. However, this mask is not helpful in children or those with beards. In this situation, the provider should wear a power air purifying respirator (PAPR). These should be worn for aerosol generating procedures, such as intubations.
N95 masks are not resistant to oil (denoted by ‘N’) and remove at least 95% of airborne particles that are 0.3 microns or larger. The coronavirus is approximately 0.06-0.14 microns in size, but these particles are typically found in droplets of much greater size. N95 masks can provide protection against particles 0.08-0.2 microns in size based on one study.5
Can you reuse an N95 that has been sterilized in some manner? There is a means of using ultraviolet germicidal irradiation (UVGI). This inactivates microorganisms but can also degrade the mask material, decreasing its effectiveness in filtering particles. There is not consistent or reliable way of determining the number of safe reuses unfortunately. One study found filter penetration increased by up to 1.25% after one UVGI application, though resistance to flow was unchanged.6 If times become dire, you can also make your own respirator mask if necessary with supplies at the hospital:
A second respirator mask is a PAPR, which should be worn by providers with beards and certain types of facial hair (CDC recommendation). A PAPR should be cleaned and disinfected if utilized. It is important to refer to the make / model of the specific PAPR at your institution so you are aware of all the details.

PPE
- Contact precautions = a waterproof gown + gloves.
- Droplet precautions = contact precautions + surgical mask + eye protection (goggles or disposable face shield).
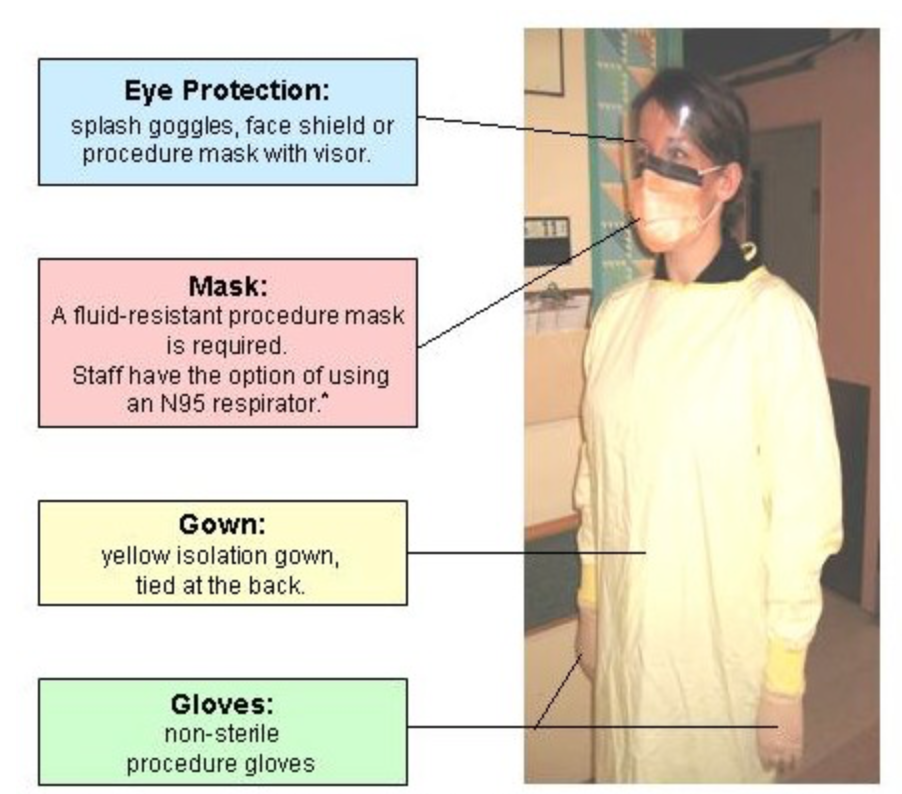
Airborne precautions are similar but include respiratory mask such as N95 or a PAPR in place of a surgical mask. A hair cover or hood should also be used for aerosol-generating procedures with a N95.

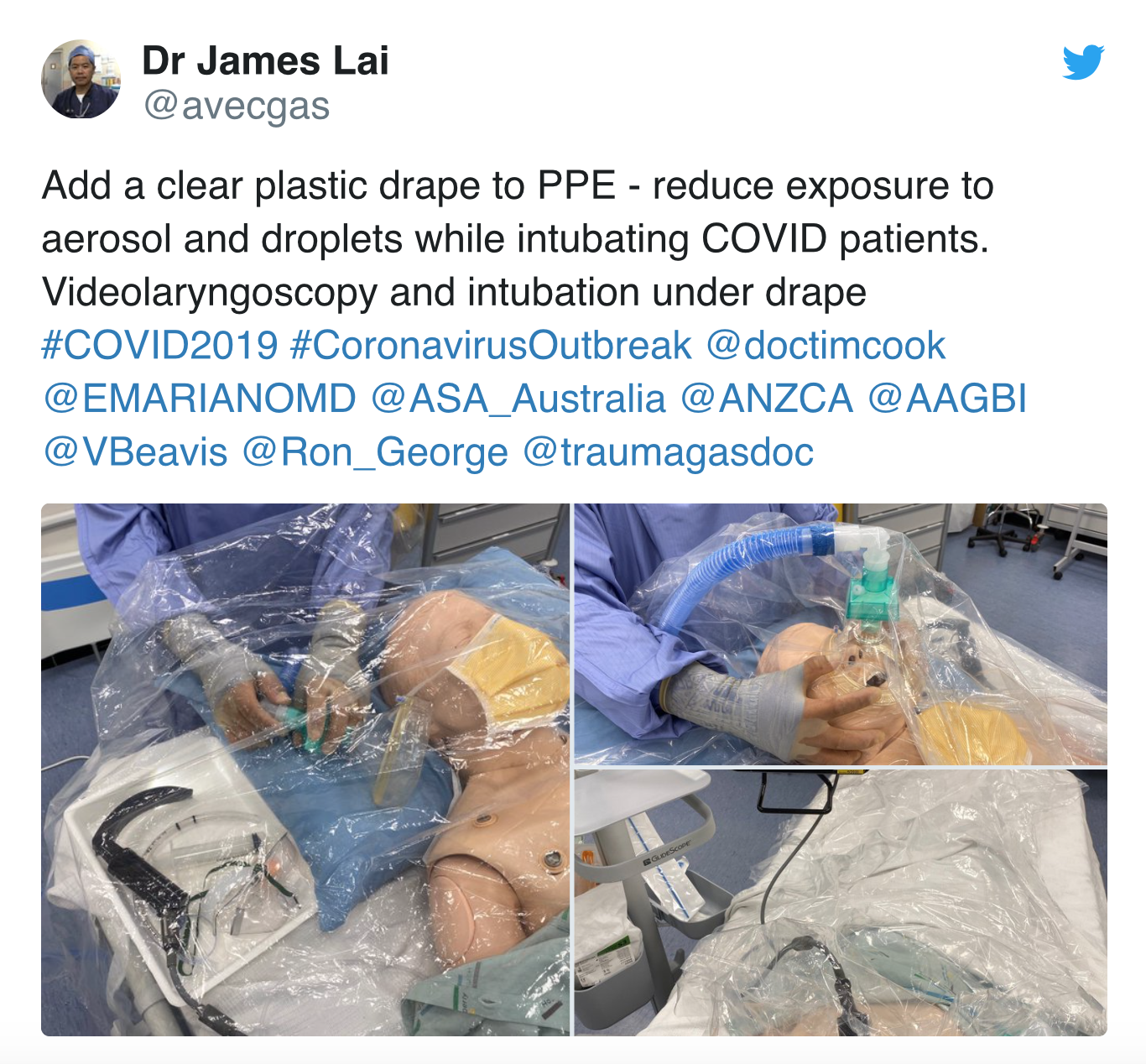
For intubation, we recommend the following if able: N95 with surgical mask over it (later step controversial to some with limited PPE) or PAPR, goggles surrounding the eyes or face shield, bunny suit with hood or disposable fluid proof gown, 2 pairs of gloves (1 pair underneath sleeves of gown and 1 over the under layer that are longer cuffed). If a hooded suit is unavailable, use a sterile disposable cap. A clear plastic drape should be placed over the equipment and patient during intubation, along with use of video laryngoscopy. This may reduce aerosol and droplet contamination.
Shoe covers are NOT recommended, as they increase risk of exposure during removal.
How do you don and doff your PPE?
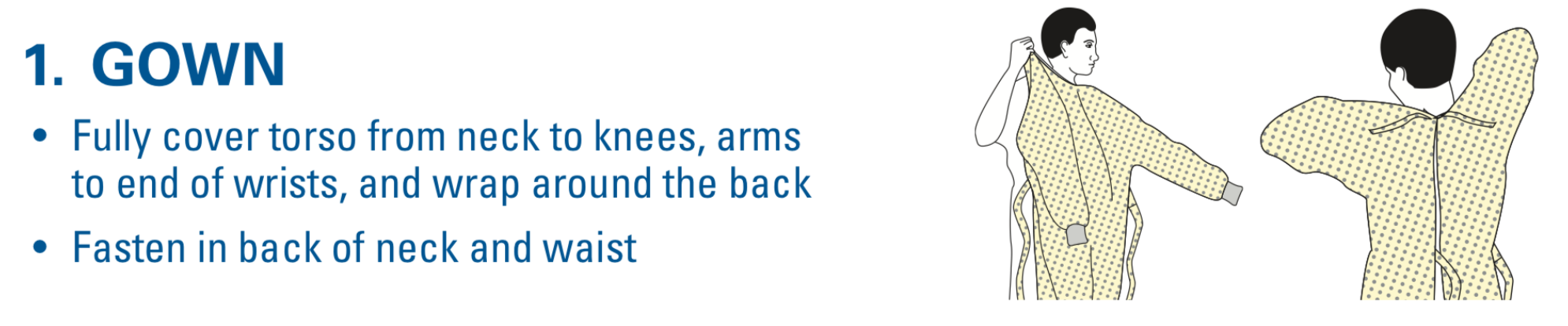
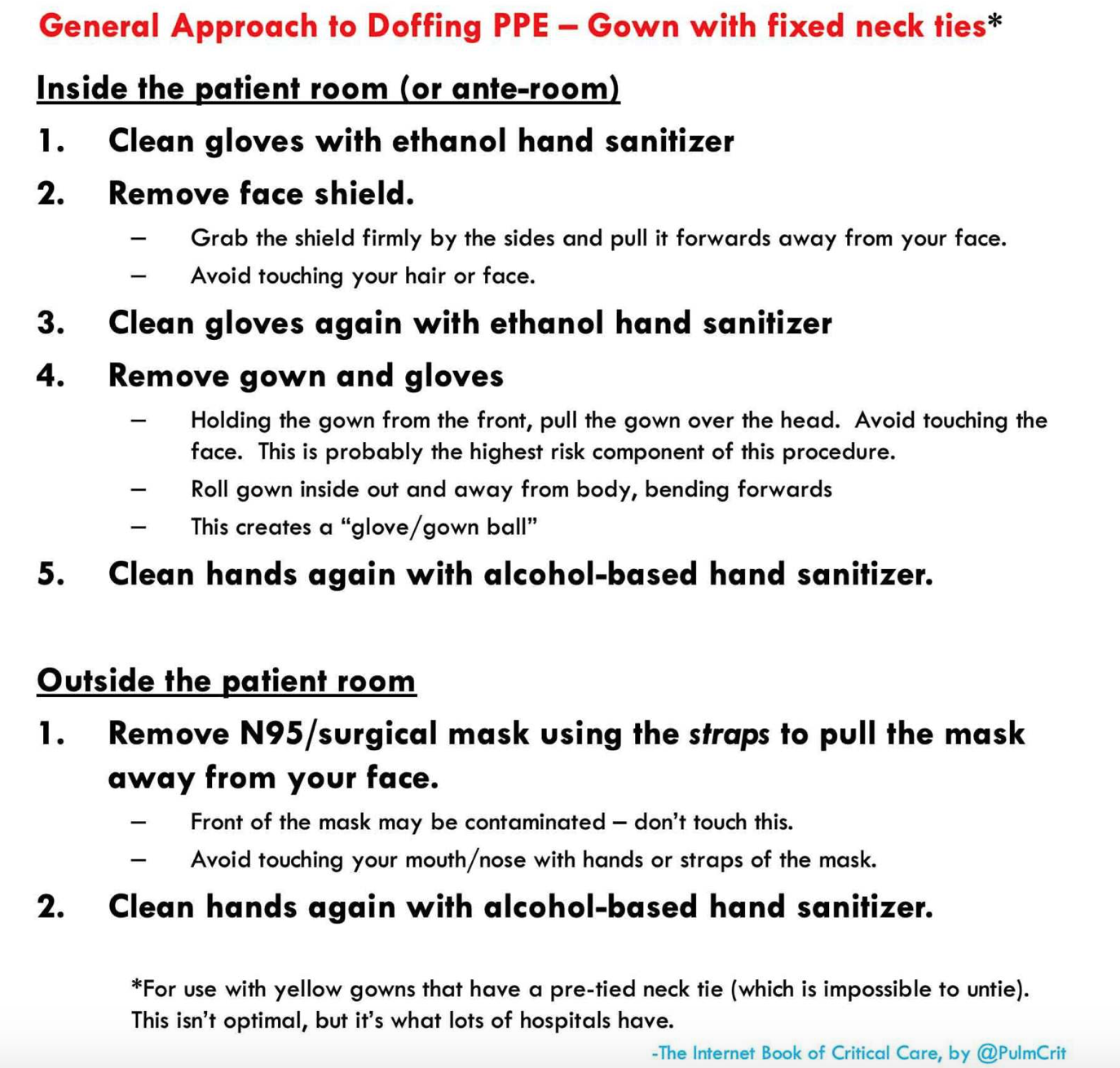
These steps are essential to reducing the risk of contact transmission. The hardest component is removing the gear, and there are many ways where this goes wrong. The best technique is to have a partner assist you in both donning and doffing utilizing a checklist. A tear away gown and gloves that go over the sleeve are advised.
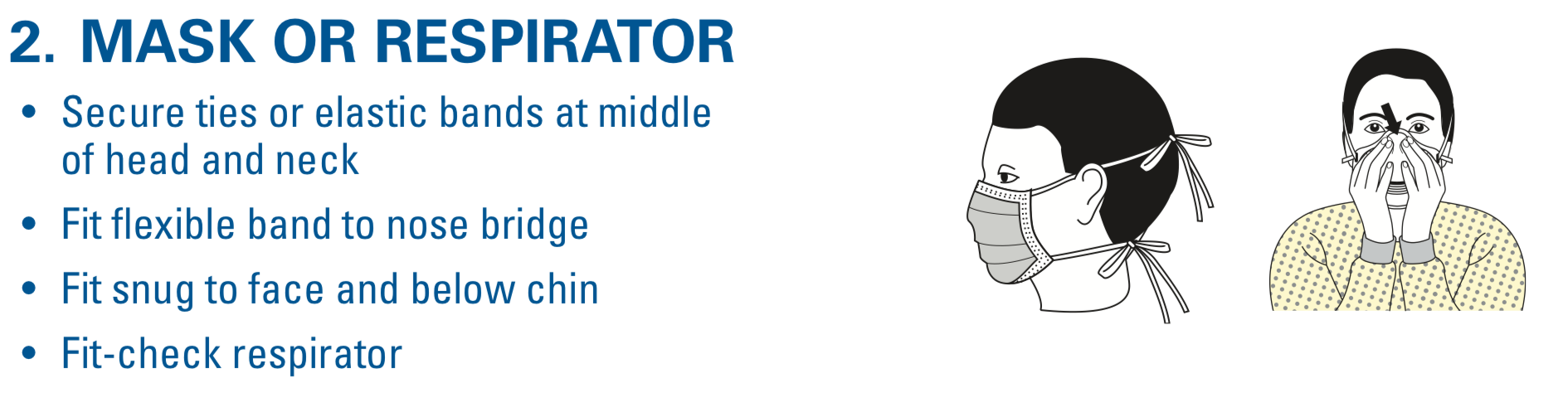
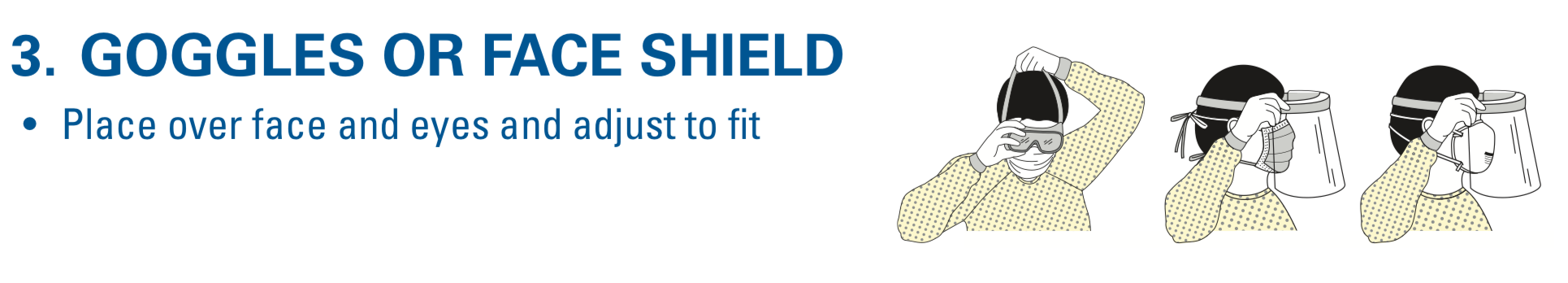
The CDC has a great handout that takes you through step by step for donning:
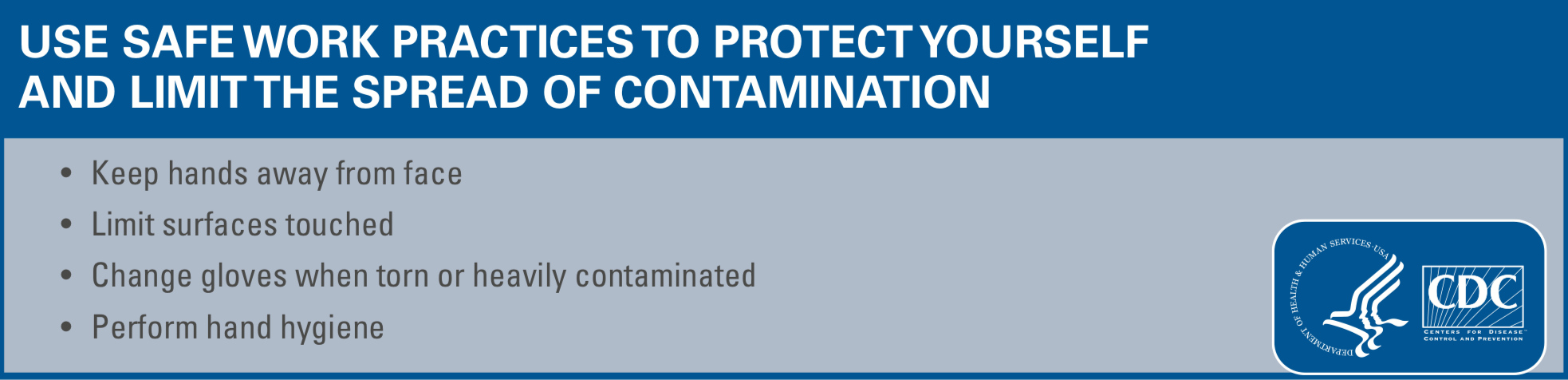
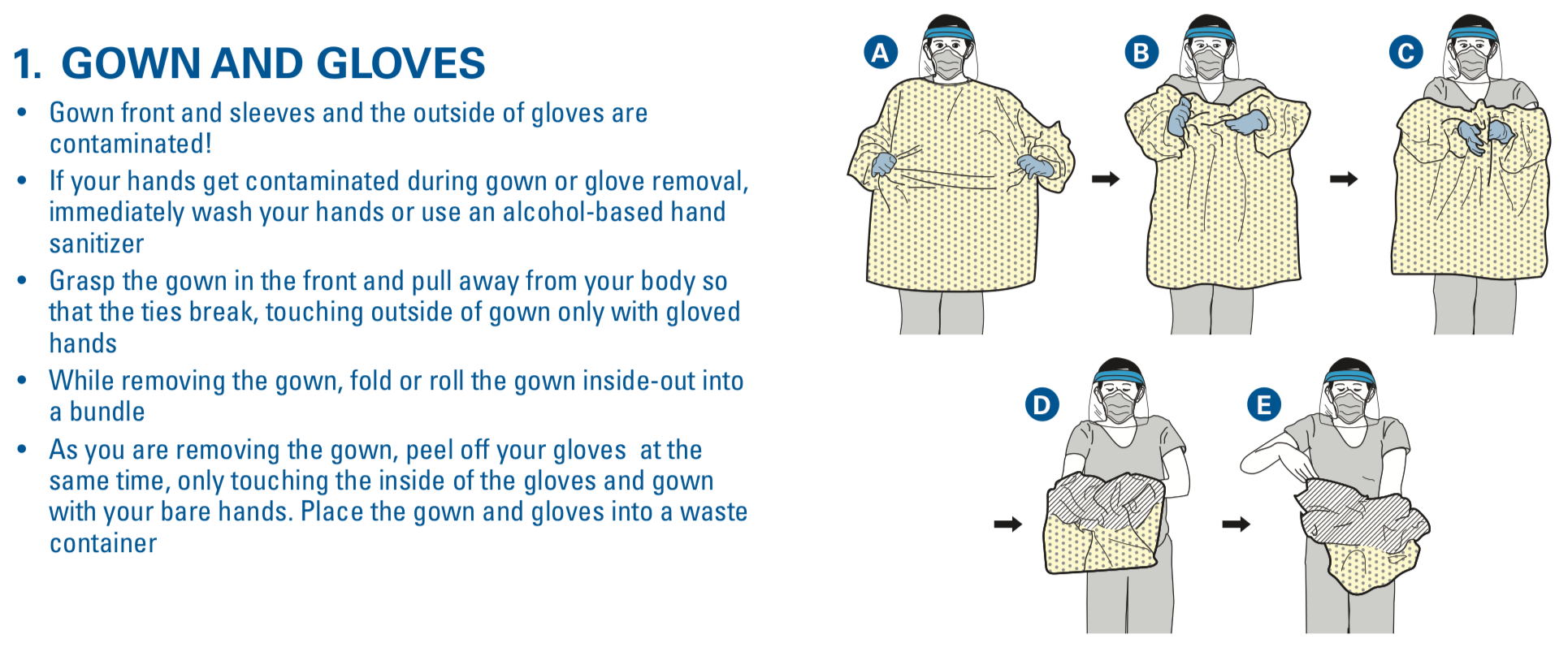
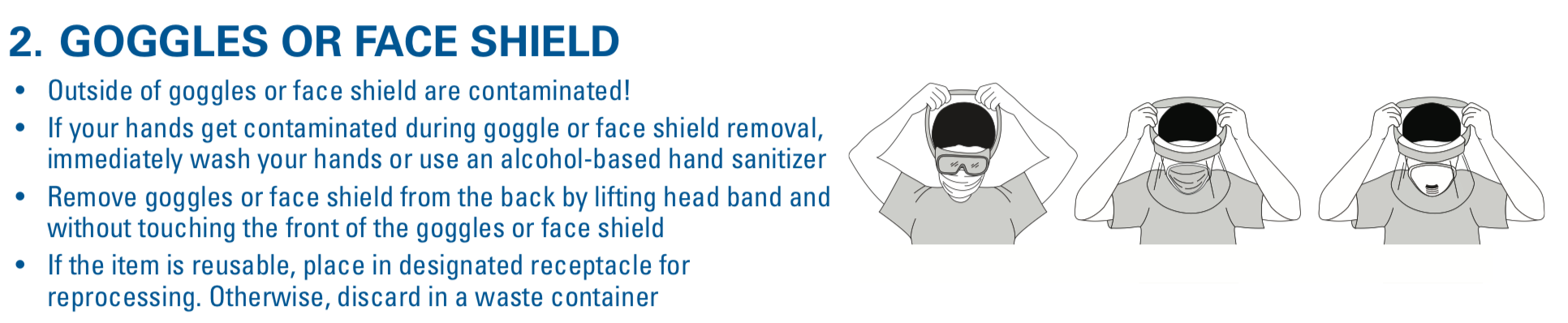
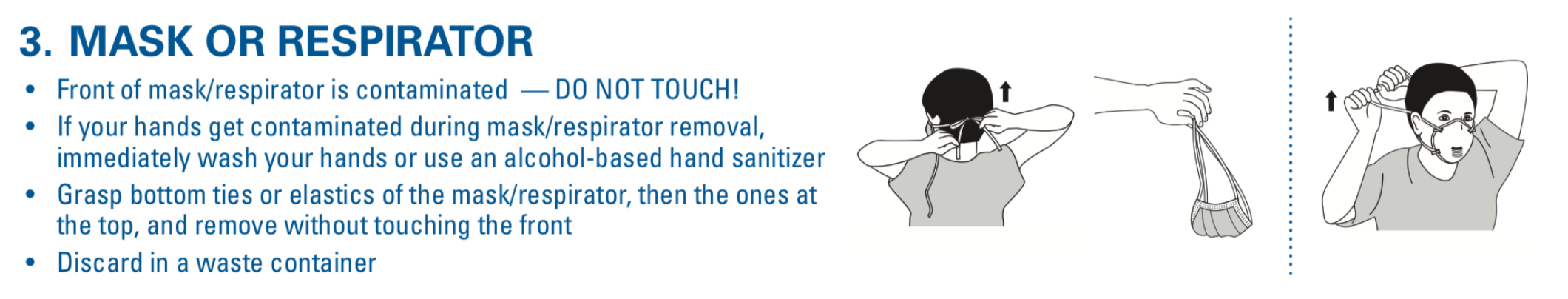
The CDC also has two methods for doffing. Of note, we only demonstrate one, in which the gown and gloves are removed in the first step. Make sure to sanitize before step 1 below, as well as between each step if able. Make sure to dispose of the gown, gloves, and if disposable, the eye protection, within the room. The face mask should be removed outside the room.


Here is a great handout from the IBCC courtesy of Josh Farkas:
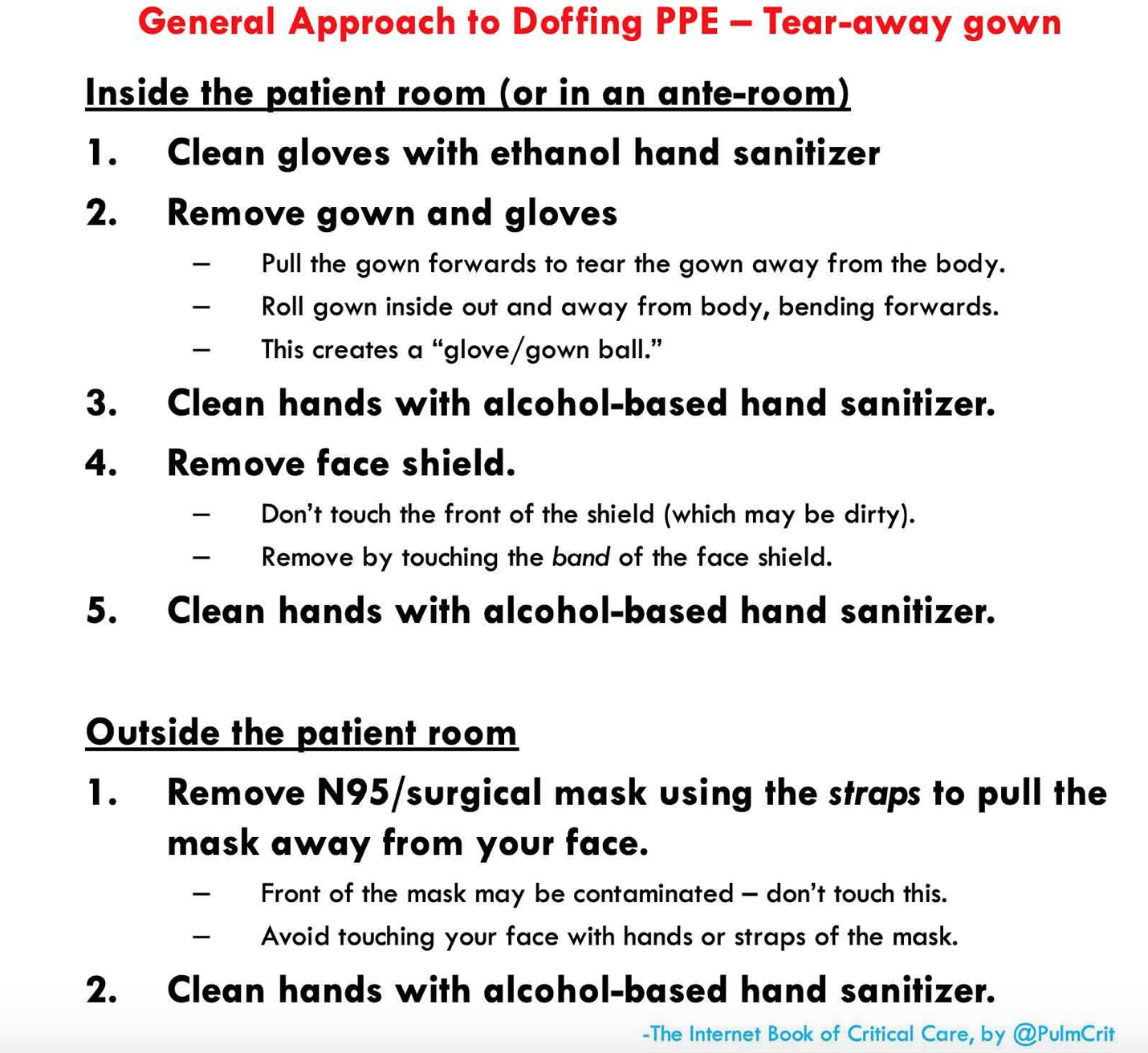
A fixed gown with a tie at the back of the neck is more difficult. You can use double gloves as well, with removing the top layer of gloves first before removing anything else.
This video from NETEC walks you through donning and doffing (donning begins at 5:00 and doffing at 11:14):
Sunnybrook Hospital also has a great video:
Many centers are having issues with PPE supplies. The CDC has recommendations pertaining to optimizing PPE supplies: https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/index.html
Post Shift Decontamination
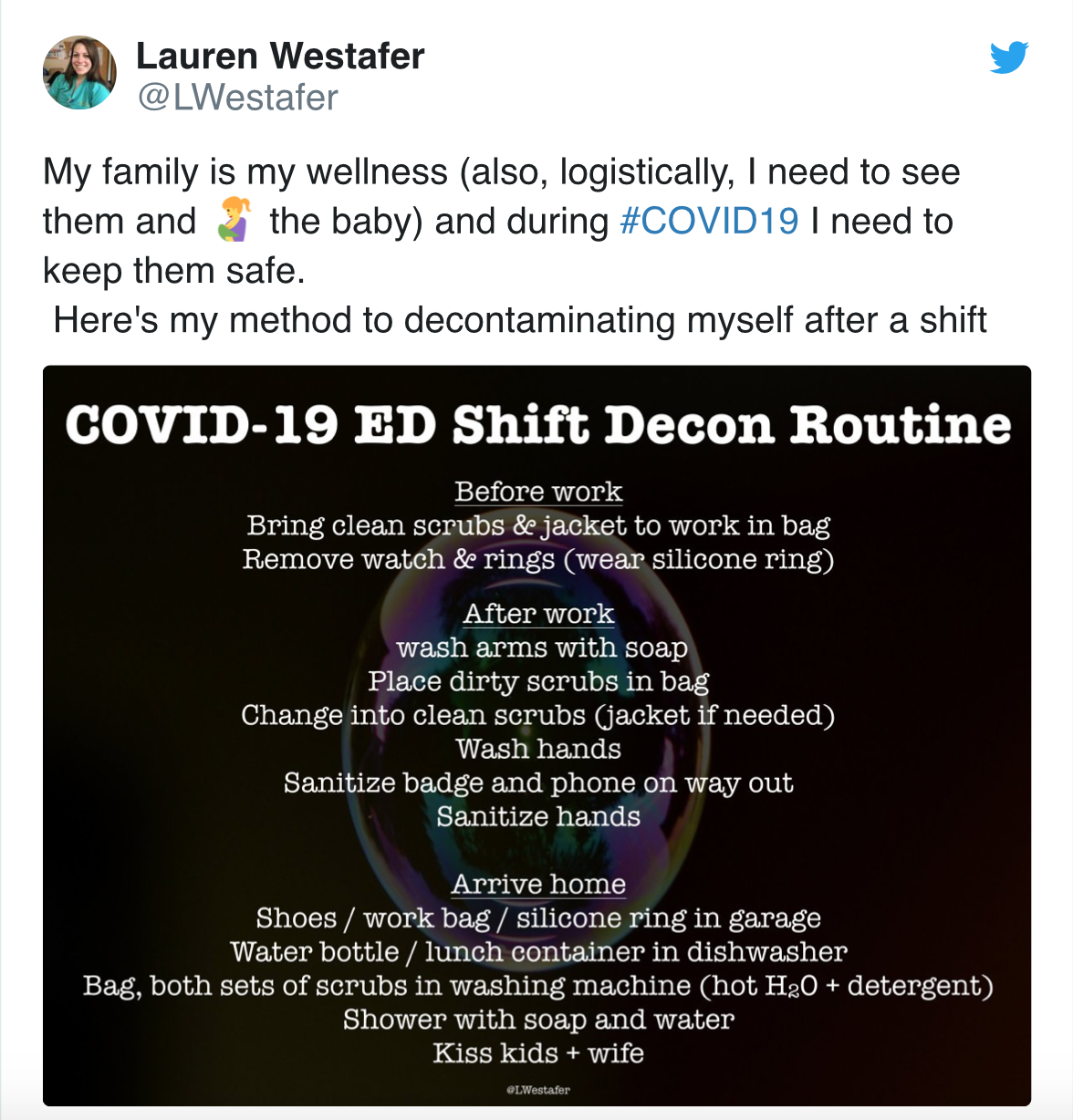
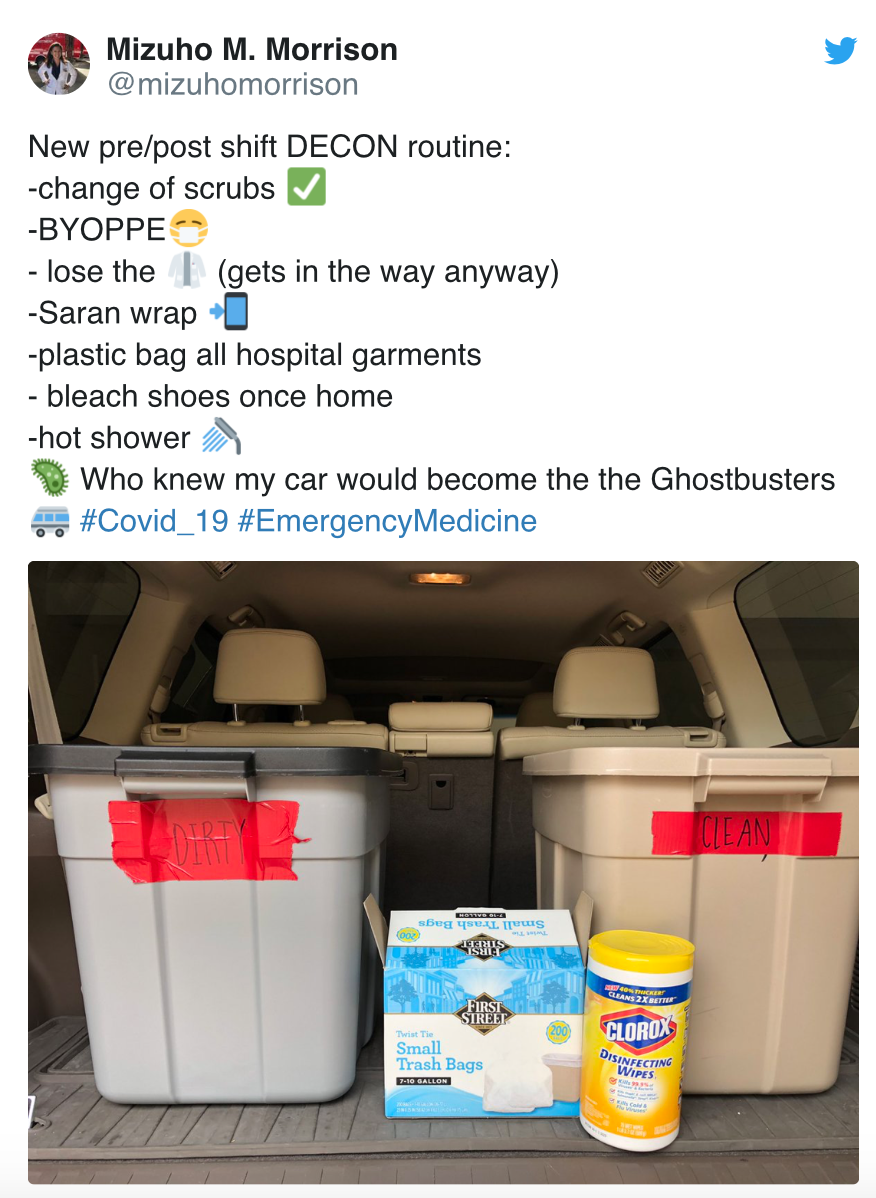
Lauren Westafer and Mizuho Morrison have a great set of tips for decontamination after shift to protect our loved ones:
Pearls:
- Limit exposure to the patient (limited number of providers in the room) and remove watches and jewelry on the upper extremities before starting your shift.
- Use a constructed checklist and a partner to assist in donning and doffing.
- If no partner is available, use a checklist and don and doff in front of a mirror if able.
- Ensure the cuff is tucked into the gloves. The gloves should cover the gown, and there should be no gaps. Longer cuffed gloves are preferable, as they allow you to remove the gown and gloves in a single motion.
- Aerosol generating procedures are high risk. Wear a respiratory mask with hood or cap.
- Sanitize before donning and before each step when doffing. Clean your gloved hands before doffing (We recommend in between steps of the doffing process).
- Have a decontamination process when you leave your shift (to include cleaning your phone and badge).
Thanks for reading, and please comment if you have found ways of reusing PPE or tips in donning and doffing PPE. Let’s all learn together so we are safe and healthy as we deal with this pandemic!
References:
- del Rio C, Malani PN. COVID-19—New Insights on a Rapidly Changing Epidemic. Published online February 28, 2020. doi:10.1001/jama.2020.3072
- Van Doremalen N, Morris DH, Holbrook MG, et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N Engl Jour Med. DOI: 10.1056/NEJMc2004973
- Coronavirus Disease 2019. https://www.cdc.gov/coronavirus/2019-ncov/hcp/index.html
- MacIntyre CR, Seale H, Dung TC, et al. A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ Open. 2015;5(4):e006577. Published 2015 Apr 22. doi:10.1136/bmjopen-2014-006577
- Lee SA, Grinshpun SA, Reponen T. Respiratory Performance Offered by N95 Respirators and Surgical Masks: Human Subject Evaluation with NaCl Aerosol Representing Bacterial and Viral Particle Size Range. Annals of Occupational Hygiene. 2008;52(3):177-185.
- Lindsley WG, Martin SB Jr, Thewlis RE, et al. Effects of Ultraviolet Germicidal Irradiation (UVGI) on N95 Respirator Filtration Performance and Structural Integrity. J Occup Environ Hyg. 2015;12(8):509–517.







1 thought on “Personal Protective Equipment (PPE) Pearls – COVID-19”
Pingback: COVID-19: Prevention - REBEL EM - Emergency Medicine Blog