Authors: Brit Long, MD (@long_brit, EM Attending Physician at SAUSHEC) and Michael D. April, MD, DPhil, MSc (EM Attending Physician at SAUSHEC) // Edited by: Alex Koyfman, MD (@EMHighAK, EM Attending Physician, UT Southwestern Medical Center / Parkland Memorial Hospital)
You’re caring for a 24-year-old male who presents with abdominal pain post MVC at 45 mph. Vital signs are normal, and your exam reveals RUQ and RLQ abdominal pain with no peritoneal signs and negative FAST. The rest of your secondary exam is normal, with no other tenderness or visible injuries. You have provided fentanyl and Zofran, and you ponder your next move. What imaging is needed? Does this patient require the infamous “Pan-scan”, or whole body CT? This post will evaluate the literature surrounding whole body CT in trauma, specifically whether mortality is improved with its use.
Trauma is a primary cause of death in patients under 45 years, and patients with trauma are commonly evaluated and managed in the ED.1-4 These patients may have multisystem injuries requiring life-threatening intervention. Assessment of these patients requires consideration of the ABCs and then secondary exam.5 Studies in trauma are often protocol driven, which may include ultrasound, X-rays, and laboratory testing after initial history and exam. Unfortunately, these tests including chest X-ray, pelvic X-ray, and ultrasound (FAST) have limitations in diagnostic accuracy and sensitivity for detecting injuries requiring further intervention.6-10
Physicians often rely on more advanced imaging to evaluate for dangerous injuries in trauma, such as CT. This test is sensitive and rapid for detecting injuries.11-15 CT use has increased in trauma, and use of whole-body CT (WBCT) is commonly used to assess for traumatic injuries.16-31 Multi-detector CT with its speed and diagnostic accuracy made WBCT feasible. The specific WBCT protocol varies depending on the institution, though it commonly entails CT of the head and C-spine without IV contrast, with CT of the neck, chest, abdomen, and pelvis with IV contrast.29-36 Radiation approximates 20 mSv based on the imaging technology.30,36-38 The alternative is selective imaging, which is based on history, exam, and other tests (US, labs, X-rays).5,12,30 WBCT is indispensable in critical patients in whom history and exam are not reliable. However, what about patients in whom history and exam may allow a selective approach to imaging? Does WBCT impact mortality? What does the literature say?
WBCT Pros:
Supporters of WBCT argue that it allows rapid diagnosis and earlier treatment, while shortening ED and hospital length of stay and improving outcomes (mortality).12,21-31 Proponents also argue decreased patient mortality, decreased time to diagnosis, and decreased time to treatment, as demonstrated in several observational studies.12,21-31
WBCT Cons:
- Those who advocate for selective imaging state WBCT may increase radiation exposure. The association between malignancy risk and radiation exposure is generally accepted, but the specifics of this association are not clear-cut, as most models assume a linear relationship of radiation exposure and cancer risk.36-44 This specific model comes from cancer data and radiation exposure in over 120,000 atomic bomb survivors.40,41 Studies possess different assumptions and calculations evaluating exposure timeline, patient age, type of CT, and technology. The risk of lethal cancer varies from one per 322 to 1250 WBCTs.36-45 Just as an example, WBCT has an average effective dose of 20-24 mSv, while CT head noncontrast provides 1.8 mSv dose and CT chest 4-5 mSv.44,45
- The second consequence is increase in incidental findings on CT. This number approaches 53% in patients undergoing WBCT, compared to 34%-45% for patients undergoing selective imaging.46-50 Do these findings require further evaluation? This varies, ranging from 48%-68%,47-51 and unfortunately, many of these studies do not describe clinical outcomes or clarify the proportion of findings requiring further action. It is also difficult to know whether over-diagnosis is associated with increased cost, patient anxiety, and further radiation for more evaluation.51-53
- Other potential risks include increased time to treatment for dangerous injuries and increased costs, but the primary arguments are above.
Trauma Scoring Systems
Before diving into evaluation of the studies looking at WBCT and mortality, an understanding of trauma scoring systems is needed. Why? Most of these studies do not compare mortality between patients undergoing WBCT versus selective imaging, but rather differences between mortality as predicted by trauma score and measured mortality.
Several scales can be used, which use different components including anatomic and physiologic variables. Let’s face it; many of these are not straightforward. The Trauma and Injury Severity Score (TRISS) is one of the most commonly used, which consists of the Revised Trauma Score (RTS), which measures physiologic variables, and the Injury Severity Score (ISS), which evaluates anatomic injuries.54-59
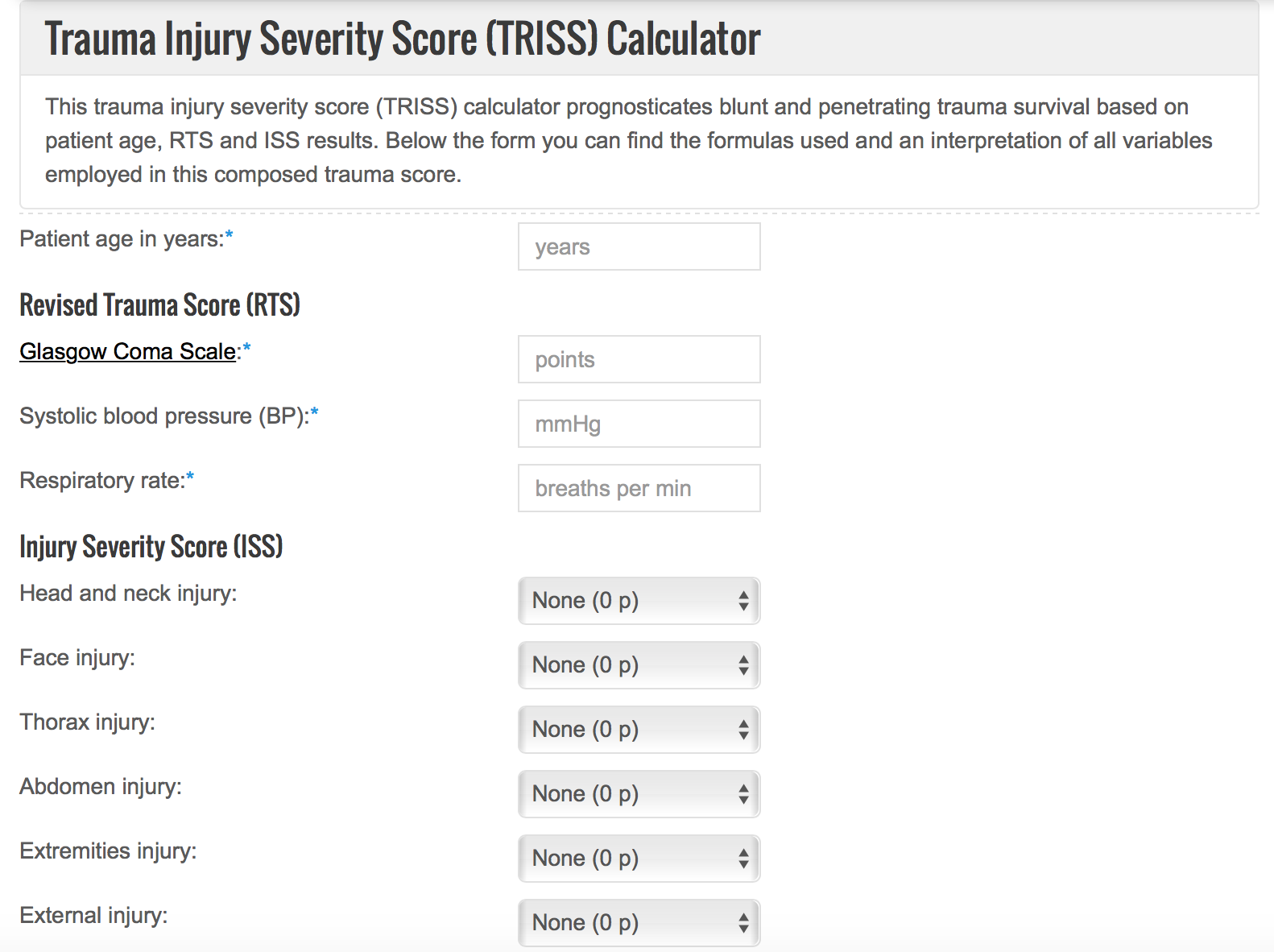
TRISS scoring calculator, from https://www.thecalculator.co/search.php
Many of the studies evaluating WBCT use the ISS, which was first used for automobile injuries in 1971.58 This score divides the body into 6 regions, then ranks injury severity on a 6-point scale, and finally takes the regions with the highest scores and squares and adds them. Points range from 0-72. This score evaluates anatomical injuries, whether or not the patient has symptoms.54-59 By undergoing more imaging, patients have greater scores based on the ISS.
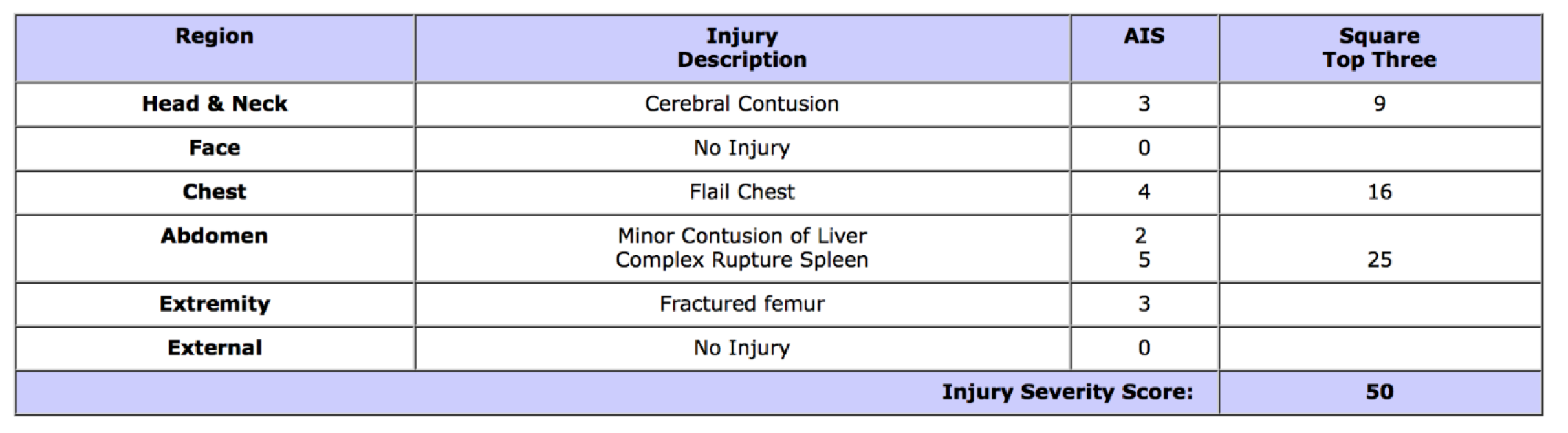
Example ISS, from http://www.trauma.org/archive/scores/iss.html
Several studies have evaluated these scoring systems in trauma.60,61 A study by Gupta et al. evaluated 701 patients undergoing WBCT in a post hoc analysis.61 Physicians indicated which part of the scan desired. The study found WBCT detected non-critical injuries in 92 patients, and the median ISS in these patients with WBCT was 10. If excluding anatomic information provided by the undesired scans which did not require intervention, the median ISS decreased to 5.61 This demonstrates the potential bias present in WBCT ability to decrease mortality based on prediction by ISS. The mortality benefit may be associated with artificial elevation in ISS predicted mortality.
Mortality and WBCT
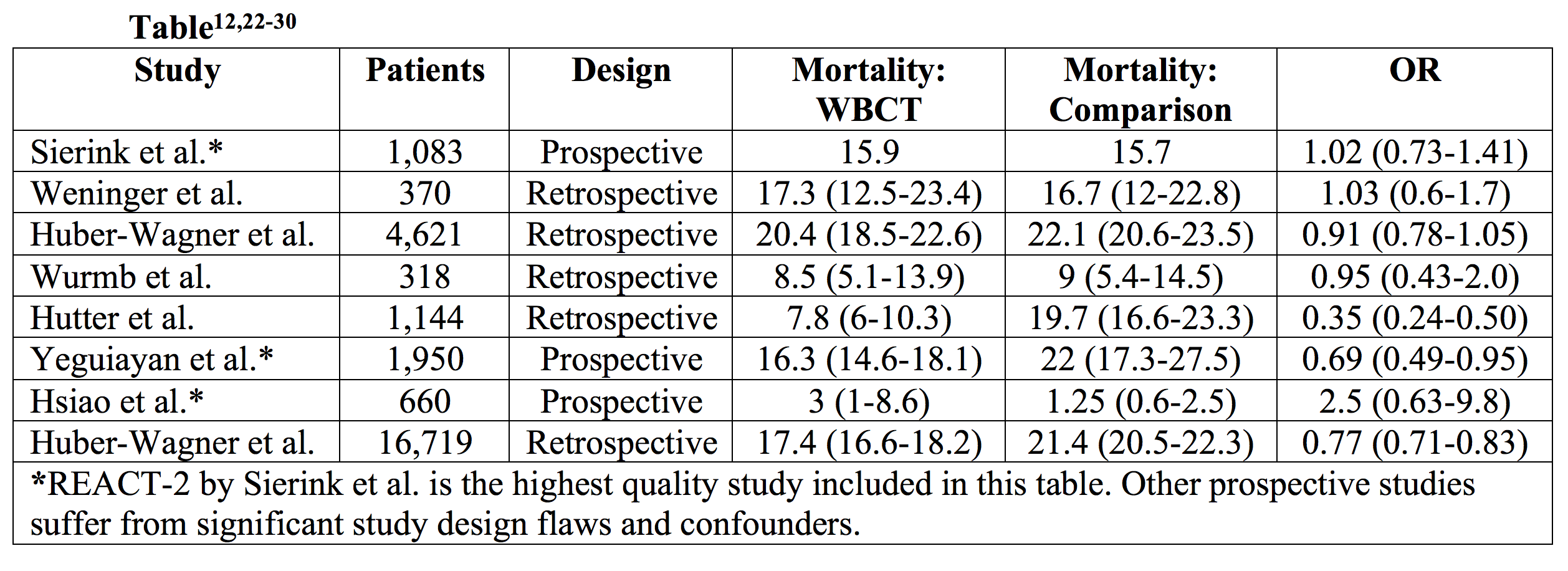
Several studies have evaluated WBCT and mortality, with most observational in design.
– Salim et al. 2006 evaluated 592 trauma patients with significant mechanism of injury, with no visible external injury, finding WBCT changed management in 18.9% of patients. No comparator group was used, and examination of the patients were not well described.11
– Huber-Wagner et al. 2009 retrospectively evaluated 4,621 patients, with a comparison of mortality as predicted by trauma scores. Patients with WBCT had 25% less mortality than that predicted by TRISS. Whoever, overall mortality was similar no matter the imaging strategy.22
– This again suggests WBCT may artificially inflate anatomical trauma scores.
– Huber-Wagner et al. 2013 retrospectively evaluated 16,719 patients (9,233 in the WBCT group). The WBCT had a mortality of 17.4% versus selective scanning mortality of 21.4%, though this study was observational.23
– A meta-analysis by Caputo et al. included 7 studies with 25,782 patients, with 52% undergoing WBCT. Overall ISS was higher in the WBCT though mortality was lower, with odds ratio 0.75 (95% CI 0.7-0.79). Time to diagnosis and treatment were also improved in the WBCT group.62
– Jiang et al. in 2014 conducted a meta-analysis of 11 studies and 26,731 patients, finding decreased mortality (OR 0.66, 95% CI 0.52-0.85) and ED length of stay (27.58 minute difference, 95% CI 12.12-43.04 min) in the WBCT group.63
– Surendran et al. in a systematic review suggested studies suffer from significant confounders and bias, and authors argue a meta-analysis cannot be conducted due to issues with data and study heterogeneity.64
Wait…Bias and Confounders?
These prior studies and meta-analyses are predominantly observational, not randomized, and based on trauma scoring systems. The groups undergoing WBCT and selective imaging often varied in studies, creating a risk of bias. Some have expressed concerns of bias due to studies excluding patients who died within 30 minutes of completing imaging, and patients who survive the WBCT may be healthier (known as “time-immortal bias”). The meta-analyses expressing improved mortality with WBCT suffer from including studies with high risk of bias, as these studies included patients with significant differences in baseline characteristics and incidence of polytrauma.62,63 WBCT is more likely to be used in trauma centers with better manning and ability to treat trauma. The Surrendran et al. systematic review also expressed concern that patients undergoing selective CT may be too unstable to undergo CT.64
So we have a suggestion of mortality benefit from the literature, but high risk of bias with multiple confounders. Are there better designed studies to evaluate?
REACT-2
Few prospective observational studies have evaluated WBCT in trauma, though these have design flaws in patient selection and analysis.26,27 Sierink et al. conducted a prospective, multicenter randomized trial with modified intention to treat analysis in 2016.30
– Patient inclusion criteria:
1) Trauma patients with Respiratory rate > 29/min or < 10/min, pulse > 120/min, SBP < 100 mmHg, estimated exterior blood loss > 500 mL, GCS < 13, abnormal pupillary reaction on site OR
2) Suspected Diagnoses: Fractures from at least two long bones; flail chest, open chest, or multiple rib fractures; pelvic fracture; unstable vertebral fractures; spinal cord compression OR
3) Severe mechanism of injury: Fall from height (> 3 meters), ejection from vehicle, death of occupant in same vehicle, severely injured patient in same vehicle, wedged or trapped chest/abdomen
– Exclusion criteria: Age < 18years, known pregnancy, referred from another hospital, any patient too unstable to undergo CT requiring resuscitation or immediate operation
– 1403 patients were randomized, with 1083 patients included for final analysis.
– WBCT included CT from vertex to pubic symphysis vs. selective scanning following US with chest and pelvic X-ray.
– A randomization stratification protocol was used to ensure equivalent cohorts in patient characteristics, treatments, and prior survival probability.
Results
– Investigators found no difference in 24-hr mortality (WBCT 8% vs. selective imaging 6%, p = 0.23), 30-day mortality (WBCT 17% vs. vs. selective imaging 16%, p = 0.69), or all patient mortality (WBCT 15.9% vs. selective imaging 15.7%, p = 0.92).
– Patients with polytrauma did not demonstrate mortality difference, and neither did patients with traumatic brain injury.
– 46% of patients randomized to selective imaging underwent CT of all body regions (essentially a WBCT).
– 54% of patients avoided WBCT, and this group received slightly less radiation overall (approximately 1 mSv).
Does this change management?
Prior studies have suffered from confounders and bias, with most retrospective and observational. It is not clear whether these studies adequately adjusted for confounders and bias. Also, basing mortality results on trauma scores can have complicating factors. REACT-2 is the best study to date evaluating the question of whether WBCT provides mortality benefit.30
WBCT can decrease time to diagnosis and may improve decisions based on imaging in patients who are unevaluable with history and exam, have multi-system injuries, or severe mechanism of injury, though these subgroups require further study.12,22-30 However, improvement in mortality is not suggested with the highest quality study to date.
Recommendations
There are protocols determining need for WBCT in trauma. Most of these take into account mechanism of injury, patient injuries, hemodynamic status, and other studies such as labs and FAST scan, with recommendation to obtain WBCT in patients with abnormal mental status, hemodynamic instability, and suspicion of critical injury.30,65-67
Ultimately, the physician should go through their trauma ABC’s and conduct a history and exam. US should be a component of this exam. Patients with concern for severe polytrauma or those who are not clinically evaluable may benefit from WBCT. At this point, in patients who are evaluable with no evidence of polytrauma, selective imaging based on history and exam is recommended.
Case Conclusion: The 24-year-old male has improved with your treatments, and his labs and FAST appear normal. You elect for abdominal CT, which is normal. You complete a tertiary, which is also normal. After the patient’s pain improves and he demonstrates PO tolerance, you discharge him with follow up.
For more on REACT-2, please see –
EMNerd: https://emcrit.org/emnerd/case-anatomic-injury-part-ii/
The Bottom Line: http://www.thebottomline.org.uk/summaries/em/react-2/
St. Emlyn’s Blog: http://stemlynsblog.org/jc-always-need-whole-body-ct-trauma-st-emlyns/
Key Points:
– Many centers now use WBCT, which has displayed mortality benefit and decreased time to diagnosis and ED length of stay in observational studies that suffer from significant bias.
– Increased radiation exposure and incidental findings can occur with WBCT.
– Studies evaluating WBCT in trauma suffer from a myriad of potential confounders and biased analyses.
– REACT-2 is the only prospective, randomized controlled trial with intention to treat analysis comparing WBCT to selective imaging in trauma patients, finding no difference in mortality between these two strategies.
– Based on this study, WBCT does appear to decrease time to diagnosis and length of stay in the ED. WBCT did not demonstrate improvement in mortality based on this study.
– In patients with polytrauma or unreliable history and exam, WBCT should be utilized.
– Patients who are evaluable through history and exam with focal trauma should undergo selective imaging.
This post is sponsored by www.ERdocFinder.com, a supporter of FOAM and medical education, who with their sponsorship are making FOAM material more accessible to ER physicians around the world.
References/Further Reading
- National Trauma Institute. Trauma statistics. Website on the Internet 2014; Available from: http://www.nationaltraumainstitute.org/home/trauma_statistics.html. Accessed November 13, 2016.
- European health data. Website on the Internet 2014; Available from: http:// ec.europa.eu/health/data_collection/docs/idb_report_2013_en.pdf. Accessed November 13, 2016.
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS) 2015 [cited 2015 01/02/17]. http://www.cdc.gov/injury/wisqars.
- Rhee P, Joseph B, Pandit V, Aziz H, Vercruysse G, Kulvatunyou N, et al. Increasing trauma deaths in the United States. Annals of Surgery. 2014;260(1):13-21.
- ATLS Subcommittee; American College of Surgeons’ Committee on Trauma; International ATLS working group. Advanced trauma life support (ATLS®): the ninth edition. J Trauma Acute Care Surg. 2013 May;74(5):1363-6.
- Rozycki GS, Ochsner MG, Jaffin JH et al. Prospective evaluation of surgeons’ use of ultrasound in the evaluation of trauma patients. J Trauma. 1993; 34:516-526.
- McElveen TS, Collin GR. The role of ultrasonography in blunt abdominal trauma: a prospective study. Am Surg. 1997; 63:184-188.
- Hoffstetter P, Dornia C, Schafer S et al. Diagnostic significance of rib series in minor thorax trauma compared to plain chest lm and computed tomography. J Trauma Manag Outcomes. 2014; 8:10.
- Elmali M, Baydin A, Nural MS et al. Lung parenchymal injury and its frequency in blunt thoracic trauma: the diagnostic value of chest radiography and thoracic CT. Diagn Interv Radiol. 2007; 13:179-182.
- Duane TM, Tan BB, Golay D et al. Blunt trauma and the role of routine pelvic radiographs: a prospective analysis. J Trauma. 2002; 53:463-468.
- Salim A, Sangthong B, Martin M et al. Whole body imaging in blunt multisystem trauma patients without obvious signs of injury: results of a prospective study. Arch Surg. 2006; 141:468-473.
- Weninger P, Mauritz W, Fridrich P, et al. Emergency room management of patients with blunt major trauma: evaluation of the multislice computed tomography protocol exemplified by an urban trauma center. J Trauma. 2007; 62:584-591.
- Gralla J, Spycher F, Pignolet C, Ozdoba C, Vock P, Hoppe H. Evaluation of a 16-MDCT scanner in an emergency department: initial clinical experience and workflow analysis. AJR Am J Roentgenol. 2005;185:232–238.
- Kanz KG, Paul AO, Lefering R et al. Trauma management incorporating focused assessment with computed tomography in trauma (FACTT) – potential effect on survival. J Trauma Manag Outcomes. 2010; 4:4.
- Oikonomou A, Prassopoulos P. CT imaging of blunt chest trauma. Insights Imaging. 2011; 2:281-295.
- Leidner B, Beckman MO. Standardized whole-body computed tomography as a screening tool in blunt multitrauma patients. Emergency Radiology. 2001; 8:20-8.
- Sampson MA, Colquhoun KB, Hennessy NL. Computed tomography whole body imaging in multi-trauma: 7 years experience. Clinical Radiology. 2006; 61:365-369.
- Saltzherr TP, Goslings JC. Effect on survival of whole-body CT during trauma resuscitation. Lancet. 2009; 374:198-199.
- Ptak T, Rhea JT, Novelline RA. Experience with a continuous, single-pass whole-body multidetector CT protocol for trauma: The three-minute multiple trauma CT scan. Emergency Radiology. 2001; 8(5):250-256.
- Philipp MO, Kubin K, rmann M et al. Radiological emergency room management with emphasis on multidetector-row CT. [Review] [22 refs]. European Journal of Radiology. 2003; 48:2-4.
- Kanz KG, rner M, Linsenmaier U et al. [Priority-oriented shock trauma room management with the integration of multiple-view spiral computed tomography]. [German]. Unfallchirurg. 2004; 107(10):937- 44.
- Huber-Wagner S, Lefering R, Qvick LM et al. Effect of whole-body CT during trauma resuscitation on survival: a retrospective, multicenter study. Lancet. 2009; 373:1455- 1461.
- Huber-Wagner S, Biberthaler P, Haberle S, et al. Whole-body CT in haemodynamically unstable severely injured patients – a retrospective, multicenter study. PLOS One 2013;8(7):e68880.
- Wurmb TE, Quaisser C, Balling H, et al. Whole-body multislice computed tomography (MSCT) improves trauma care in patients requiring surgery after multiple trauma. Emerg Med J 2011;28: 300–04.
- Hutter M, Woltmann A, Hierholzer C, Gartner C, Buhren V, Stengel D. Association between a single-pass whole-body computed tomography policy and survival after blunt major trauma: a retrospective cohort study. Scand J Trauma Resusc Emerg Med 2011; 19: 73.
- Yeguiayan JM, Yap A, Freysz M, et al. Impact of whole-body computed tomography on mortality and surgical management of severe blunt trauma. Crit Care 2012; 16: R101.
- Hsiao KH, Dinh MM, McNamara KP, Bein KJ, Roncal S, Saade C, Waugh RC, Chi KF. Whole-body computed tomography in the initial assessment of trauma patients: is there optimal criteria for patient selection? Emerg Med Australas. 2013;25(2):182Y191.
- Wada D, Nakamori Y, Yamakawa K, et al. Impact on survival of whole-body computed tomography before emergency bleeding control in patients with severe blunt trauma. Crit Care 2013; 17: R178.
- Sierink JC, Saltzherr TP, Beenen LF, et al. A multicenter, randomized controlled trial of immediate total-body CT scanning in trauma patients (REACT-2). BMC Emerg Med 2012; 12: 4.
- Sierink JC, Treskes K, Edwards MJ, Beuker BJ, den Hartog D, Hohmann J, Dijkgraaf MG, et al. Immediate total-body CT scanning versus conventional imaging and selective CT scanning in patients with severe trauma (REACT-2): a randomised controlled trial. 2016 Aug 13;388(10045):673-83.
- Ptak T, Rhea JT, Novelline RA. Radiation dose is reduced with a single-pass whole- body multi-detector row CT trauma protocol compared with a conventional segmented method: initial experience. Radiology. 2003;229:902-905.
- Prokop A, Hötte H, Krüger K, et al. Multislice CT in diagnostic work-up of polytrauma. Unfallchirurg. 2006;109:545-550.
- Rieger M, Czermak B, El Attal R, et al. Initial clinical experience with a 64-MDCT whole- body scanner in an emergency department: better time management and diagnostic quality? J Trauma. 2009;66:648-657.
- Van Vugt R, Deunk J, Brink M, et al. Influence of routine computed tomography on predicted survival from blunt thoracoabdominal trauma. Eur J Trauma Emerg Surg. 2011;37:185-190.
- Stengel D, Ottersbach C, Matthes G, et al. Accuracy of single-pass whole-body computed tomography for detection of injuries in patients with major blunt trauma. CMAJ. 2012;184:869-876.
- Brenner DJ, Elliston CD. Estimated radiation risks potentially associated with full-body CT screening. Radiology 2004; 232:735-738.
- Tien HC, Tremblay LN, Rizoli SB et al. Radiation exposure from diagnostic imaging in severely injured trauma patients. J Trauma. 2007; 62:151-156.
- Winslow JE, et al. Quantitative assessment of diagnostic radiation doses in adult blunt trauma patients. Ann Emerg Med 2008;52:93-97.
- Brenner DJ, Hall EJ. Computed tomography—an increasing source of radiation exposure. N Engl J Med. 2007; 357 (22): 2277–2284.
- Hall EJ, Brenner DJ. Cancer risks from diagnostic radiology. Br J Radiol.2008 May;81(965):362-78.
- Pierce DA, Preston DL. Radiation-related cancer risks at low doses among atomic bomb survivors. Radiat Res.2000 Aug;154(2):178-86.
- Mathews JD, Forsythe AV, Brady Z, Butler MW, Goergen SK, Byrnes GB, et al. Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. Br Med J. 2013; 346: f2360.
- Berrington de GA, Mahesh M, Kim KP et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169:2071-2077.
- Sierink JA. Total-body CT scanning in trauma patients: Benefits and boundaries. Thesis. Available at http://dare.uva.nl/search?metis.record.id=468794. Accessed November 12, 2016.
- ImPACT’s CT Dosimetry Tool. http://www.impactscan.org/ctdosimetry.htm. May 2011. Accessed 14 December 2016.
- Munk MD, Peitzman AB, Hostler DP, Wolfson AB. Frequency and follow-up of incidental findings on trauma computed tomography scans: experience at a level one trauma center. J Emerg Med. 2010;38:346-350.
- Messersmith WA, Brown DF, Barry MJ. The prevalence and implications of incidental findings on ED abdominal CT scans. Am J Emerg Med. 2001;19:479-481.
- Barrett TW, Schierling M, Zhou C et al. Prevalence of incidental findings in trauma patients detected by computed tomography imaging. Am J Emerg Med. 2009;27:428-435.
- Hoffstetter P, Herold T, Daneschnejad M et al. [Non-trauma-associated additional findings in whole-body CT examinations in patients with multiple trauma]. Rofo. 2008;180:120-126.
- Seah MK, Murphy CG, McDonald S, Carrothers A. Incidental findings on whole-body trauma computed tomography: Experience at a major trauma centre. 2016 Mar;47(3):691-4.
- Paluska TR, Sise MJ, Sack DI, Sise CB, Egan MC, Biondi M. Incidental CT findings in trauma patients: incidence and implications for care of the injured. J Trauma. 2007;62:157-161.
- Berlin L. The incidentaloma: a medicolegal dilemma. Radiol Clin North Am. 2011;49:245- 255.
- Brenner DJ. Medical imaging in the 21st century – getting the best bang for the rad. N Engl J Med. 2010;362:943-945.
- Champion HR. Trauma Scoring. Scandinavian Journal of Surgery 2002;91:12-22.
- Champion HR, Copes WS, Sacco WJ, Frey CF, et al. Improved predictions from a severity characterization of trauma (ASCOT) over Trauma and Injury Severity Score (TRISS): results of an independent evaluation. J Trauma. 1996;40(1):42-8.
- Lefering R. Development and validation of the Revised Injury Severity Classification score for severely injured patients. Europ J Trauma Emerg Med. 2009; 35: 437-447.
- Champion HR, Copes WAS, Sacco WJ, et al. The Major Trauma Outcome Study: establishing national norms for trauma care. J Trauma. 1990;30(11):1356-65.
- American Medical Association Committee on the Medical Aspects of Automotive Safety: Rating the severity of tissue damage. I. The abbreviate scale. JAMA 1971;215(2):277-280.
- Baker SP, O’Neill B, Haddon W, et al. The injury severity score: An update. J Trauma 1974;14:187.
- Gupta M, Schriger DL, Hiatt JR, et al. Selective use of computed tomography compared with routine whole body imaging in patients with blunt trauma. Ann Emerg Med. 2011;58:407-416.e15.
- Gupta M, Gertz M, Schriger DL. Injury Severity Score Inflation Resulting From Pan-Computed Tomography in Patients with Blunt Trauma. Ann Emerg Med. 2016;67(1):71-75.e3.
- Caputo ND, Stahmer C, Lim G, Shah K. Whole-body computed tomographic scanning leads to better survival as opposed to selective scanning in trauma patients: a systematic review and meta-analysis. J Trauma Acute Care Surg 2014; 77: 534–39.
- Jiang L, Ma Y, Jiang S, et al. Comparison of whole-body computed tomography vs selective radiological imaging on outcomes in major trauma patients: a meta-analysis. Scand J Trauma Resusc Emerg Med 2014; 22: 54.
- Surendran A, Mori A, Varma DK, Gruen RL. Systematic review of the benefits and harms of whole-body computed tomography in the early management of multitrauma patients: are we getting the whole picture? J Trauma Acute Care Surg 2014; 76: 1122–30.
- Davies RM, Scrimshire AB, Sweetman L, Anderton J, Holt EM. A decision tool for whole-body CT in major trauma that safely reduces unnecessary scanning and associated radiation risks: An initial exploratory analysis. Injury 2016;47:43-49.
- Lecky F, Woodford M, Edwards A, Bouamra O, Coats T. Trauma scoring systems and databases. BJA 2014;113(2):286-94.
- Gordic S, Alkadhi H, Hodel, Simmen HP, Brueesch M, Frauenfelder T, et al. Whole-body CT-based imaging algorithm for multiple trauma patients: radiation dose and time to diagnosis. BJR 2015;88:20140616.











1 thought on “The Reign of the “Pan-Scan”: Whole Body CT vs. Selective Imaging in Trauma”
Pingback: emDOCs.net – Emergency Medicine EducationPedestrian Struck by Vehicle: Pearls and Pitfalls of ED Management - emDOCs.net - Emergency Medicine Education