EM Cases: Low Risk Chest Pain and High Sensitivity Troponin – A Paradigm Shift
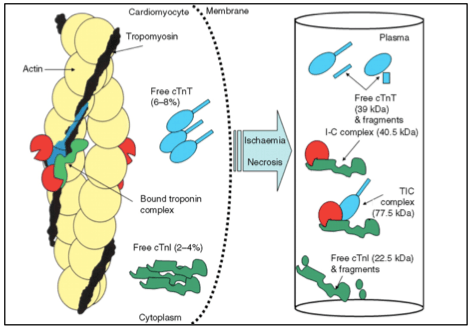
In this podcast with Dr. Eddy Lang and world expert troponin researcher Dr. Andrew McRae, we answer the not-so-simple questions…
EM Cases: Low Risk Chest Pain and High Sensitivity Troponin – A Paradigm Shift Read More »