Author: Charles Cullison, DO (Emergency Medicine Resident at UT San Antonio, TX) // Reviewed by: Skyler Lentz, MD (@skylerlentz); Alex Koyfman, MD (@EMHighAK); and Brit Long, MD (@long_brit)
Case
You are working in the Emergency Department and get called urgently to the room of a patient in respiratory distress. The nurse tells you that he is febrile with an oral temperature of 103.1 F and has a rapid heart rate. You round the corner to the patient’s room and see a middle-aged man who is leaning forward in respiratory distress with accessory muscle use. His respirations are 30 per minute. His pulse ox is 84-88%. He has family at bedside that fill in the story as you call for respiratory therapy.
The patient’s wife tells you that he has been around several other individuals who were sick with suspected COVID-19. He has no other medical problems. The chest x-ray reveals what appears to be bilateral infiltrates in an acute respiratory distress syndrome pattern. You administer empiric antibiotics for community acquired pneumonia, start a sepsis workup, obtain a viral respiratory panel, and admit him to MICU on airborne precautions. His labs show elevated inflammatory markers, an elevated d-dimer, and the CBC differential reveals lymphopenia. Why do some patients with the COVID-19 virus have mild symptoms, while others have profound immune system reaction causing widespread organ damage?

Cytokine Storm
Viruses are simple in design. Their replication cycle is predictable and highly efficient. Our body’s reaction to viruses and other pathogens, although well studied, varies widely from individual to individual. We rely on a system of cellular recognition of invading organisms and then the signaling of the invasion from those cells to our immune system. Cytokines are the signals from our cells to our bodies notifying us that we are under attack. If the cells release an appropriate amount of cytokines, an appropriate immune response can begin against the invading pathogen, giving the best chance of recovery. If there is an inappropriate or excessive cytokine release the systemic effects could be fatal. It can cause multi-system organ damage and even failure. This concept is called “cytokine storm.”1-3
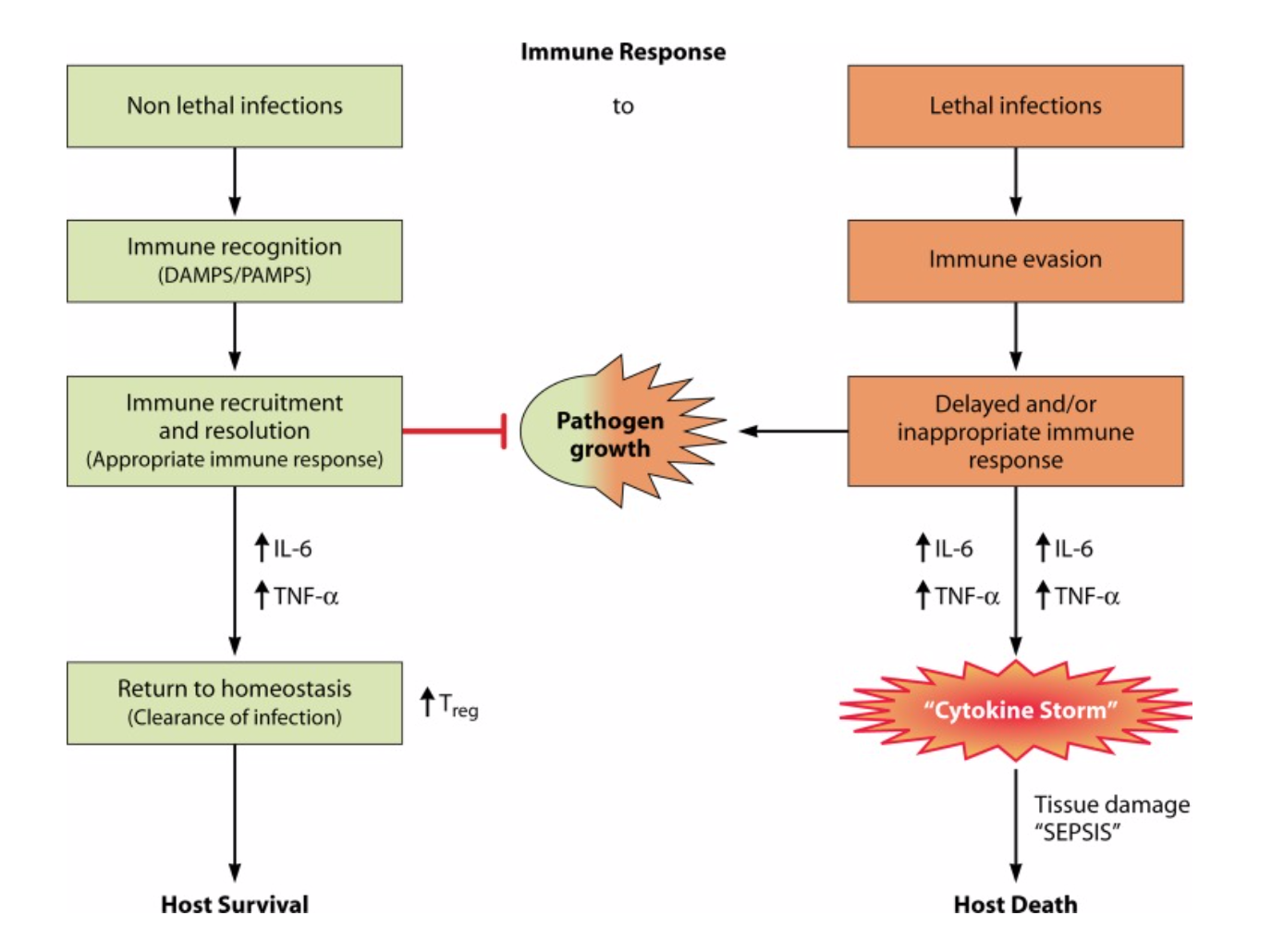
Figure 1: Inflammatory Cascade in Cytokine Storm. Adapted from Targeting the “Cytokine Storm” for Therapeutic Benefit by Riccardo V D’Elia, Kate Harrison, Petra C Oyston, Roman A Lukaszewski, Graeme C Clark 2013, Clin Vaccine Immunol 20 (3), 319-27
Cytokine storm can occur in patients suffering from pancreatitis, bacterial sepsis, multiple sclerosis, and viral respiratory infections. It has been shown to occur rarely in Epstein-Barr virus, swine flu, avian flu, influenza, and SARS-COV.4-8 Cytokine storm is suspected to be a significant cause of mortality in patients with severe disease secondary to COVID-19 infection.9
Mixed Signals
The main cytokines that are involved in cytokine storm related to viral respiratory infections include interleukin-1 (IL-1), interleukin-6 (IL-6), and tumor necrosis factor alpha (TNF-a.) During the initial phase of the viral respiratory infection, acute lung injury occurs. The infected cells release the cytokines IL-1B and TNF-a. These cytokines can be detected in the patient’s bronchoalveolar lavage sample within hours of symptoms starting. IL-6 is produced as a response to the increase of IL-1B and is increased for prolonged periods of time.1
Rapid elevated levels of IL-6 and TNF-a are implicated in cytokine induced cardiac dysfunction and are actively produced by cardiac myocytes in response to ventricular wall strain. This in turn causes cardiac remodeling and reduction in contractile performance.10
Cytokine storm is linked to hypercoagulability. IL-6 is primarily involved in the up-regulation of tissue factors that brings about initiation of coagulation. IL-1β down-regulates thrombomodulin and consequently causes defects in anticoagulant proteins, specifically impairing activation of protein C. IL-6 also binds to both RBCs and platelets causing platelet hyperactivation.11 This causes patients in a cytokine storm to be at risk for the formation of acute deep venous thrombosis and emboli.
Lastly, a subset of patients develop a syndrome called hemophagocytic lymphohistiocytosis (HLH). This is usually a pediatric rheumatological illness. It is rare, but can be acquired in adulthood by cancer, bacterial infections, fungal infections and viral infections. The symptoms of HLH include dyspnea, cough, nausea, vomiting, fever, and jaundice. There is a rapid proliferation of macrophages and cytotoxic T-cells due to hypercytokinemia.12 These macrophages and T-cells then go on to cause systemic tissue damage such as acute respiratory distress syndrome.12 The primary initial diagnostic step to make when considering HLH caused by infection is an elevated serum ferritin.
Dr. Cron, a Rheumatologist from the University of Birmingham, recently published his journal of cytokine storm syndromes and in an interview stated that up to 15 percent of the population could be genetically predisposed to having a cytokine storm syndrome in reaction to an infection.13
Management
The initial infection might be what caused the cytokine storm; however, the pathologic process of the storm can continue long after the virus has been treated and is what causes overall fatality in these patients.1 Management is 2-fold; treat the infection and prevent further self-injury.1,14-16 However, this balance is challenging. If immunomodulatory drugs are used too soon, the immune system is weakened while actively fighting an infection; if used too late, the organ injury has already been done.
Until recently, research on treatment options of cytokine storm has been limited to patients with chemotherapy induced cytokine storm.
Start with your ABCs
These patients can deteriorate rapidly and may require advanced airway and vasopressor support. There are no clinical trials that studied the different vasopressor effects on cytokine storm patients. Remember that if you are starting vasopressors on cytokine storm patients, consider that they may also be developing acute cardiac dysfunction secondary to hypercytokinemia.
Early Detection is Key
What can we do as emergency physicians? It is our job to triage patients. We determine who has mild symptoms and can go home, who needs to be admitted to medical floor with minimal supplemental oxygen, and who needs the intensive care unit.
Early detection of cytokine storm in patients can assist us in identifying patients who may decompensate and need a higher level of care or benefit from advanced therapies. The H scoring system may be useful for the early detection of cytokine storm/HLH. This score incorporates temperature, organomegaly, cytopenias, triglycerides, ferritin, AST, fibrinogen, and immunosuppression. Lymphopenia, hyperferritinemia, high fever are all components of the H-score. Furthermore, elevated LDH and elevated IL-6, have been shown to be early predictors of possible HLH.3 Inflammatory markers to include CRP should also be obtained. Unfortunately, assessing IL-6 is not possible in many centers.

Figure 2: H Score for secondary HLH adapted from COVID-19: Consider Cytokine Storm Syndromes and Immunosuppression by The Lancet
The H score, combined with LDH, CRP, and IL-6 (if available), may identify patients who are at increased risk of having severe systemic inflammation secondary to cytokine storm.3 These are the same lab values recommended by infectious disease journals for prediction of severity in COVID-19 infections after early reports from China suggested an association.17
For ease of use, see MDCalc.
Prevent Cytokine Induced Blood Clots
These patients may be hypercoagulable. It has been shown that this is a significant part of the mortality rates of cytokine storm caused by severe Influenza A infections. The infection causes the cytokine storm, the storm causes an increase in activity of the coagulation pathway, then the randomly forming blood clots further cause even more localized tissue inflammation and edema. 18 In patients with cytokine storm secondary to COVID-19 infection, one study has shown an incidence of thrombotic events as high as 31%.19 In another study on COVID-19 patients with cytokine storm, 28 day mortality rates improved with low molecular weight heparin treatment for patients having a d-dimer score greater than 6 times the normal limit or a sepsis induced coagulopathy score greater than or equal to four.20 Strongly consider starting low molecular weight heparin early in these patients.
Don’t Miss Acute Cardiac Dysfunction
Cytokines have a direct effect on the cardiac myocyte contractile ability.10 Obtain and EKG, troponin, and BNP. Look for JVD on physical exam. Use a bedside ultrasound to scan the ventricles and estimate the ejection fraction.
Treat the Underlying Condition
This cytokine storm has been caused by something—treat the underlying cause. Source control and empiric antibiotics in bacterial sepsis is straightforward. Viral infections present a challenge. There have been no human studies evaluating the use of anti-viral therapies in patients suffering from virus induced cytokine storm but with the current COVID-19 pandemic, trials are underway. New anti-viral medications are being developed and tested for the use against COVID-19 including remdesivir, lopinavir and ritonavir according to the World Health Organization.
Animal models from H5N1 influenza virus showed a combination therapy consisting of zanamivir, celecoxib, and mesalazine increased the survival of mice infected with a H5N1 influenza virus. These studies demonstrated that antiviral treatment was less effective alone than in combination with immunomodulatory therapies that suppressed inflammation.1,14,15
Add Immunomodulatory Therapies
IL-6 is a major player in cytokine storm. Tocilizumab is an IL-6 receptor inhibitor which has been validated and is considered first line therapy in treating cytokine storm in patients undergoing CAR-T-cell therapy.18 Tocilizumab’s utility in cytokine storm caused by pathogens is limited but research is ongoing due to COVID-19 and early data is promising for its use.9
Steroids are considered second line treatment of cytokine storm caused by CAR-T cell therapy but it is used in patients who are not responding to tocilizumab alone. Steroids are generally used on cytokine storm caused by infection and there have been no randomized control trials to compare it to placebo. Initial treatment may include methylprednisolone. For patients with severe neurologic symptoms, consider using dexamethasone to more efficiently penetrate the blood-brain barrier. In patients who are suspicious for adrenal insufficiency, stress doses of hydrocortisone are indicated.21
IL-1 blockade using anakinra, in the subset of patients with a cytokine storm and an HLH syndrome caused by bacterial sepsis, has been shown to have a survival benefit through a randomized control trial.22 There are multiple randomized control trials currently underway to evaluate its usefulness on COVID-19 patients with cytokine storm.
Take Home Points:
1) Cytokine Storm is a serious systemic complication of viral infections such as COVID-19, bacterial infections, rheumatologic disorders, and cancer therapies.
2) Up to 15% of the population can be predisposed to cytokine storm syndrome due to infection.
3) Early detection of cytokine storm syndrome helps triage patients appropriately and begin treatment early which improves overall mortality.
4) Consider ordering the labs tests included in the H score along with an IL-6, CRP and LDH, in admitted patients with cytokine storm.
5) Treatments of critical patients with potential for cytokine storm secondary to COVID-19 are being studied but follow the previously understood treatment regimen including anti-viral therapy, immune-modulation, anti-coagulation, and steroids.
References/Further Reading
1) Tisoncik JR, Korth MJ, Simmons CP, Farrar J, Martin TR, Katze MG. Into the eye of the cytokine storm. Microbiol Mol Biol Rev. 2012;76:16–32. doi: 10.1128/MMBR.05015-11.
2) Shakoory, B., Carcillo, J. A., Chatham, W. W., Amdur, R. L., Zhao, H., Dinarello, C. A., Cron, R. Q., & Opal, S. M. (2016). Interleukin-1 Receptor Blockade Is Associated With Reduced Mortality in Sepsis Patients With Features of Macrophage Activation Syndrome: Reanalysis of a Prior Phase III Trial. Critical care medicine, 44(2), 275–281. https://doi.org/10.1097/CCM.0000000000001402
3) D’Elia RV, Harrison K, Oyston PC, Lukaszewski RA, Clark GC. Targeting the “cytokine storm” for therapeutic benefit. Clin Vaccine Immunol. 2013;20(3):319–327. doi:10.1128/CVI.00636-12
4) Huang KJ, Su IJ, Theron M, et al. An interferon-gamma-related cytokine storm in SARS patients. J Med Virol. 2005;75(2):185–194. doi:10.1002/jmv.20255
5) Imashuku S. Clinical features and treatment strategies of Epstein-Barr virus-associated hemophagocytic lymphohistiocytosis. Crit Rev Oncol Hematol. 2002;44(3):259–272. doi:10.1016/s1040-8428(02)00117-8
6) Link H. The cytokine storm in multiple sclerosis. Mult Scler. 1998;4(1):12–15. doi:10.1177/135245859800400104
7) Makhija R, Kingsnorth AN. Cytokine storm in acute pancreatitis. J Hepatobiliary Pancreat Surg. 2002;9(4):401–410. doi:10.1007/s005340200049
8) Yuen KY, Wong SS. Human infection by avian influenza A H5N1. Hong Kong Med J. 2005;11(3):189–199.
9) Mehta, P., McAuley, D., & al, et. (2020, March 16). COVID-19: consider cytokine storm syndromes and immunosuppression. Retrieved from https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30628-0/fulltext
10) Paulus WJ. Cytokines and heart failure. Heart Fail Monit. 2000;1(2):50–56.
11) Bester, J., & Pretorius, E. (2016). Effects of IL-1β, IL-6 and IL-8 on erythrocytes, platelets and clot viscoelasticity. Scientific reports, 6, 32188. https://doi.org/10.1038/srep32188
12) Shaw, T. Y., & Schivo, M. (2016). Weathering a Cytokine Storm: A Case of EBV-Induced Hemophagocytic Lymphohistiocytosis. Journal of investigative medicine high impact case reports, 4(2), 2324709616647409. https://doi.org/10.1177/2324709616647409
13) Cron, R. (2019). Cytokine Storm Syndrome (Vol. 1).
14) Carey, M. A., Bradbury, J. A., Rebolloso, Y. D., Graves, J. P., Zeldin, D. C., & Germolec, D. R. (2010). Pharmacologic inhibition of COX-1 and COX-2 in influenza A viral infection in mice. PloS one, 5(7), e11610. https://doi.org/10.1371/journal.pone.0011610
15) Zheng, B. J., Chan, K. W., Lin, Y. P., Zhao, G. Y., Chan, C., Zhang, H. J., Chen, H. L., Wong, S. S., Lau, S. K., Woo, P. C., Chan, K. H., Jin, D. Y., & Yuen, K. Y. (2008). Delayed antiviral plus immunomodulator treatment still reduces mortality in mice infected by high inoculum of influenza A/H5N1 virus. Proceedings of the National Academy of Sciences of the United States of America, 105(23), 8091–8096. https://doi.org/10.1073/pnas.0711942105
16) Cron, R. (2020 16). Don’t forget the host: COVID-19 cytokine storm. Retrieved from https://www.the-rheumatologist.org/article/dont-forget-the-host-covid-19-cytokine-storm/
17.) Zhou, F., & al, et. (2020, March 11). Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Retrieved from https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30566-3/fulltext
18) Yang, Y., & Tang, H. (2016). Aberrant coagulation causes a hyper-inflammatory response in severe influenza pneumonia. Cellular & molecular immunology, 13(4), 432–442. https://doi.org/10.1038/cmi.2016.1
19) Klok, F. A., Kruip, M. J. H. A., Meer, N. J. M. van der, Arbous, M. S., Gommers, D. A. M. P. J., Kant, K. M., … Endeman, H. (2020, April 10). Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Retrieved from https://www.sciencedirect.com/science/article/pii/S0049384820301201
20) Tang, N., Bai, H., Chen, X., Gong, J., Li, D., & Sun, Z. (2020). Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. Journal of Thrombosis and Haemostasis, 10.1111/jth.14817. Advance online publication.
21) Lee, D. W., Gardner, R., Porter, D. L., Louis, C. U., Ahmed, N., Jensen, M., Grupp, S. A., & Mackall, C. L. (2014). Current concepts in the diagnosis and management of cytokine release syndrome. Blood, 124(2), 188–195. https://doi.org/10.1182/blood-2014-05-552729
22) Shakoory, B., Carcillo, J. A., Chatham, W. W., Amdur, R. L., Zhao, H., Dinarello, C. A., Cron, R. Q., & Opal, S. M. (2016). Interleukin-1 Receptor Blockade Is Associated With Reduced Mortality in Sepsis Patients With Features of Macrophage Activation Syndrome: Reanalysis of a Prior Phase III Trial. Critical care medicine, 44(2), 275–281. https://doi.org/10.1097/CCM.0000000000001402









1 thought on “The Storm Within: Cytokine Storm and COVID-19”
Pingback: COVID-19: Clinical/Therapeutic Staging Proposal and Treatment - REBEL EM - Emergency Medicine Blog