Author: Brit Long, MD (@long_brit) // Reviewed by Alex Koyfman, MD (@EMHighAK)
The American Heart Association/American Stroke Association (AHA/ASA) 2026 Guideline for early management of acute ischemic stroke was recently released. This post will first cover the key parts of the guideline that affect ED evaluation and management, followed by the in-depth recommendations.

Background
Stroke is a significant cause of death and disability worldwide. Ischemic stroke makes up over 80% of all strokes in the U.S. Over 600,000 patients suffer a first ischemic stroke in the U.S. every year, with 200,000 having a recurrent stroke. The prevalence of stroke in the U.S. has increased with the aging population. There is a disproportionately higher rate of stroke in those with adverse socioeconomic circumstances or social determinants of health, including economic instability, lower education, residing in stressed neighborhoods, and those in the U.S. stroke belt.
The remainder of this post will provide a brief synopsis of the guidelines, first on the key updates, followed by detailed recommendations.
The Recommendations
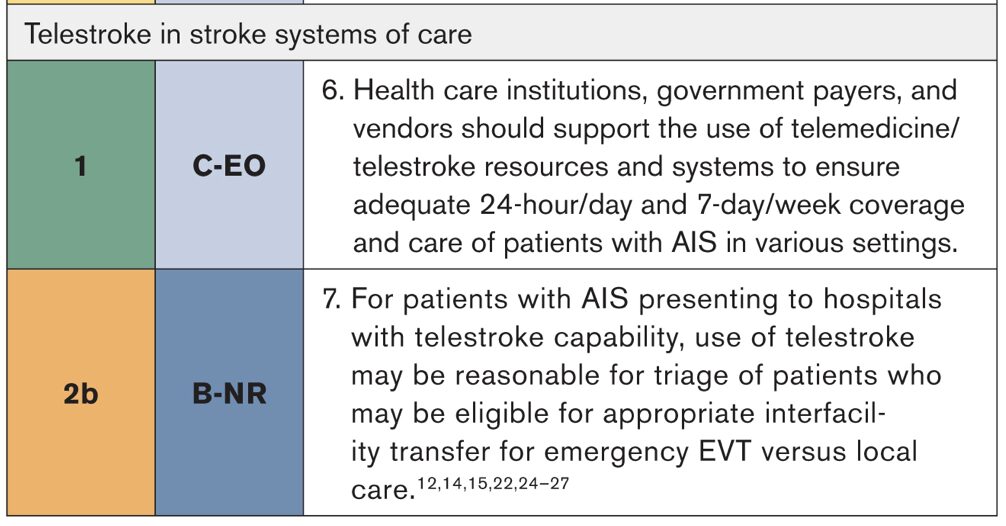
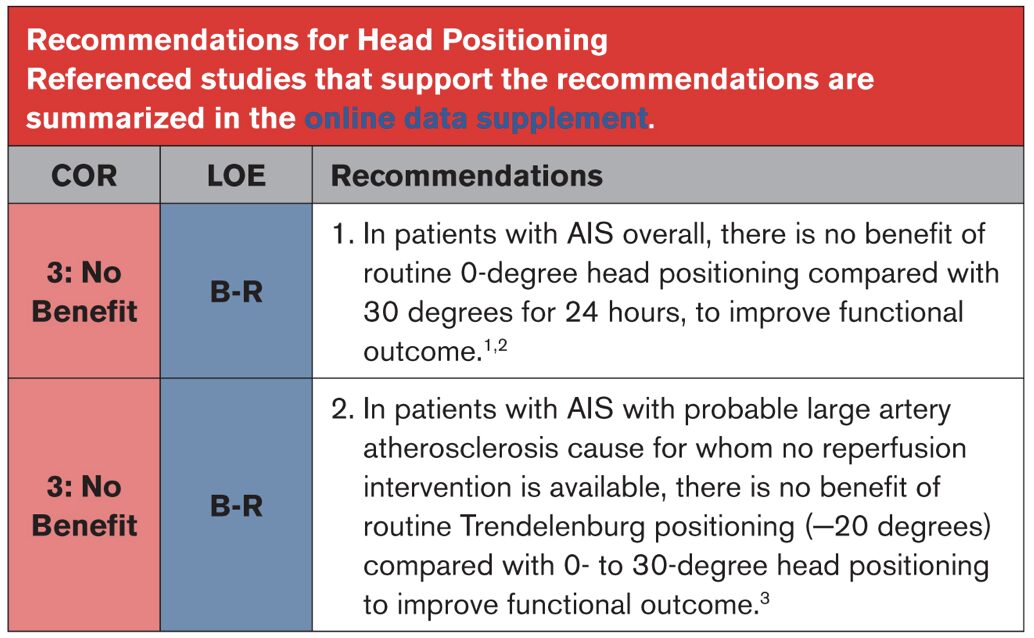
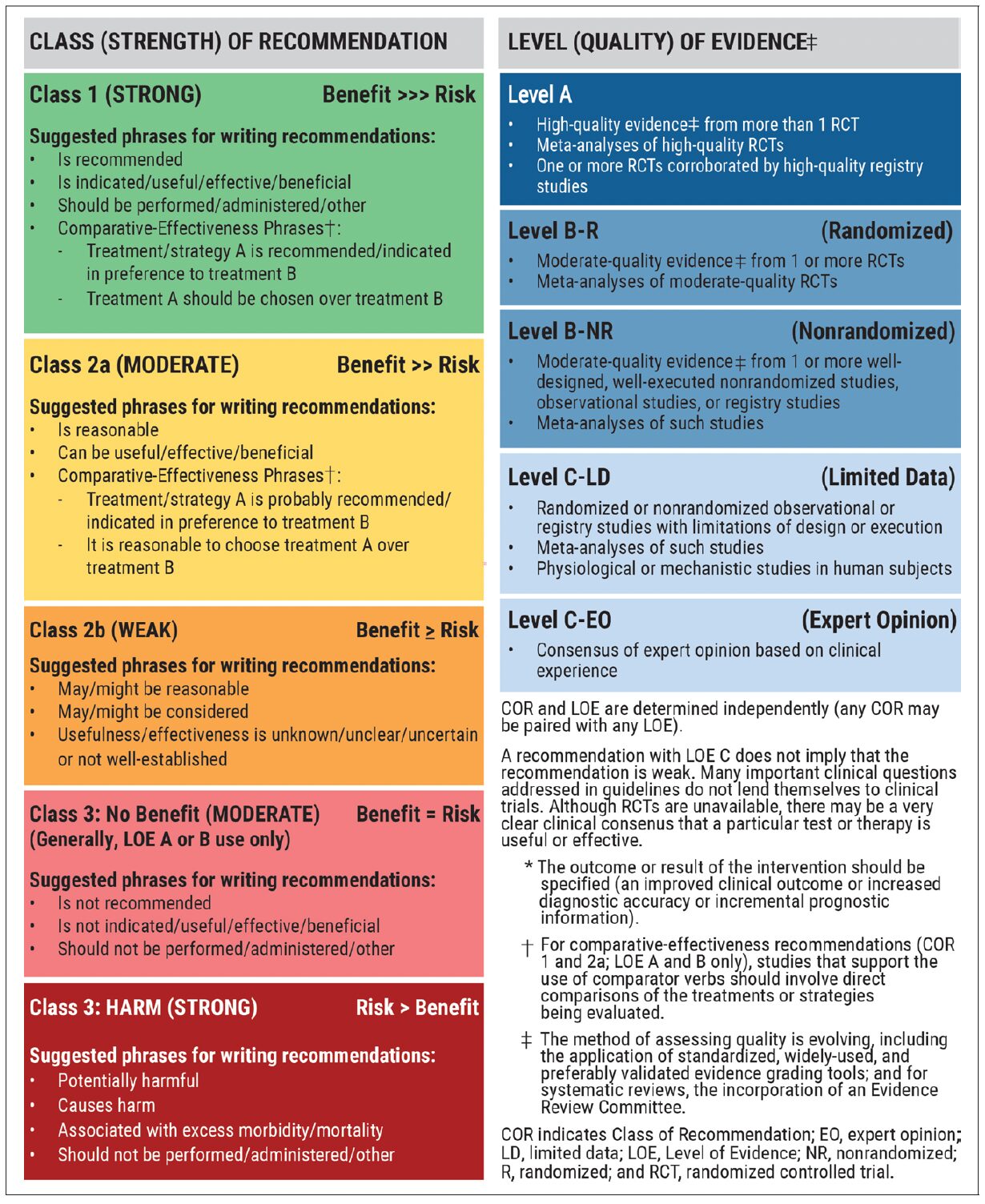
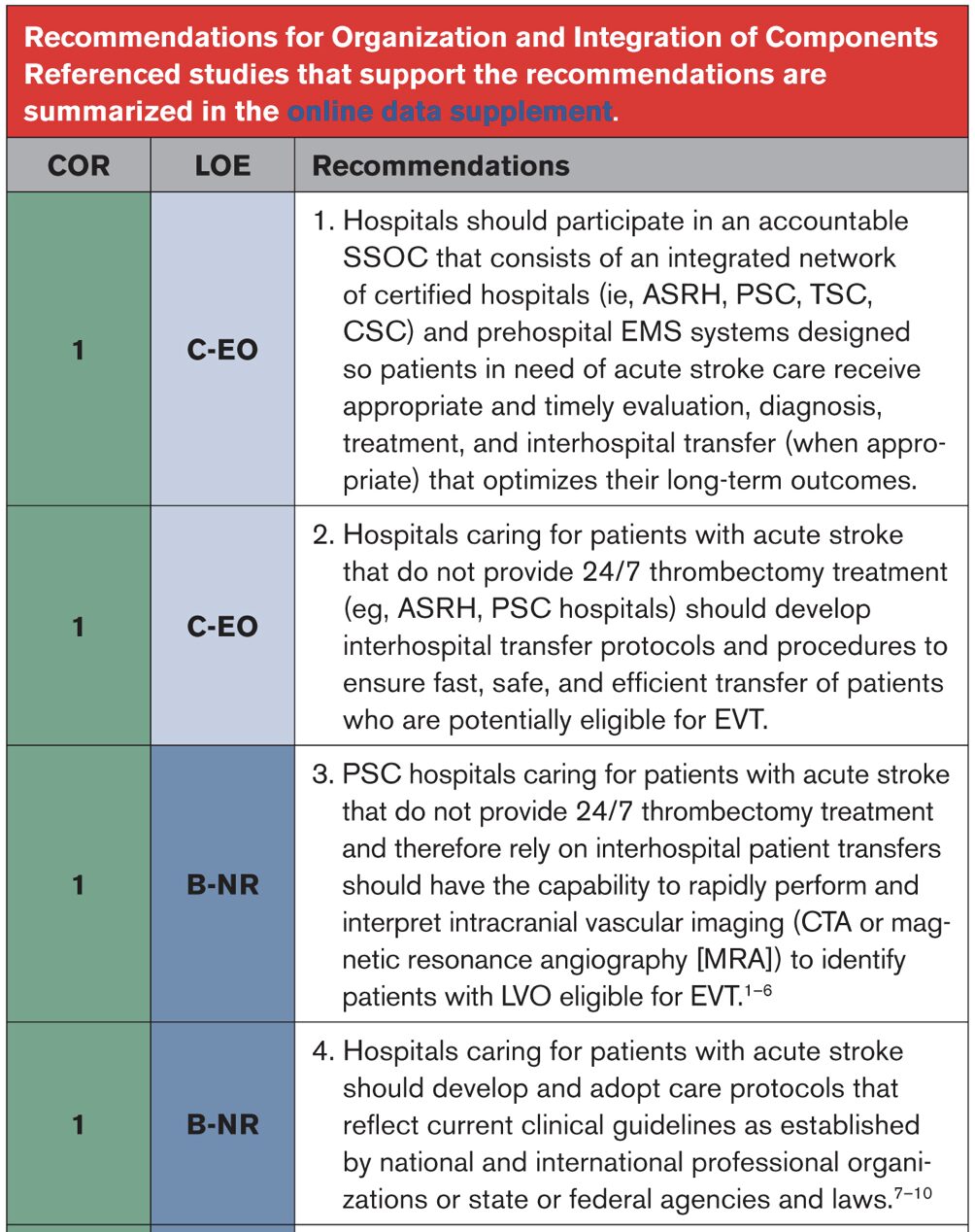
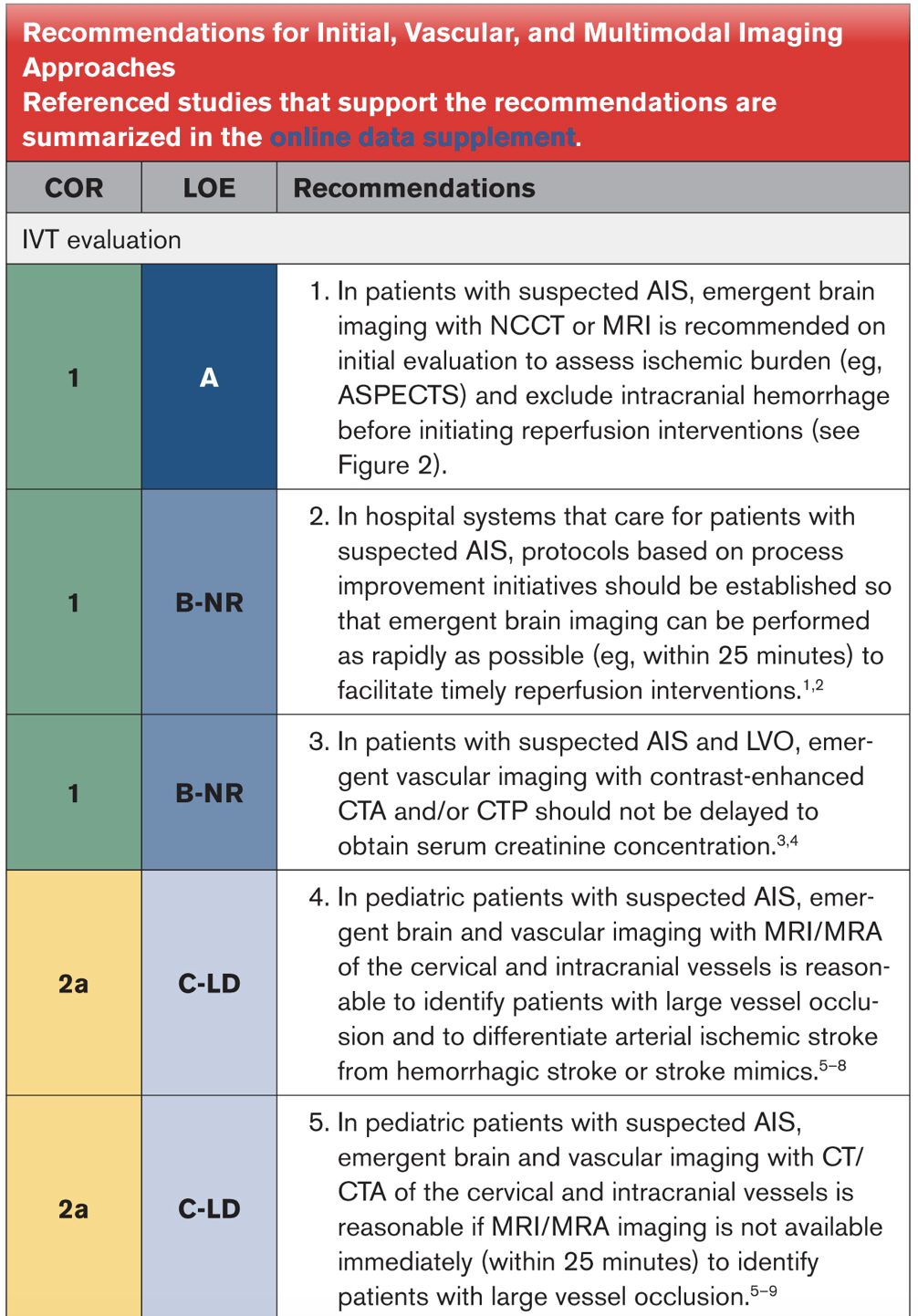
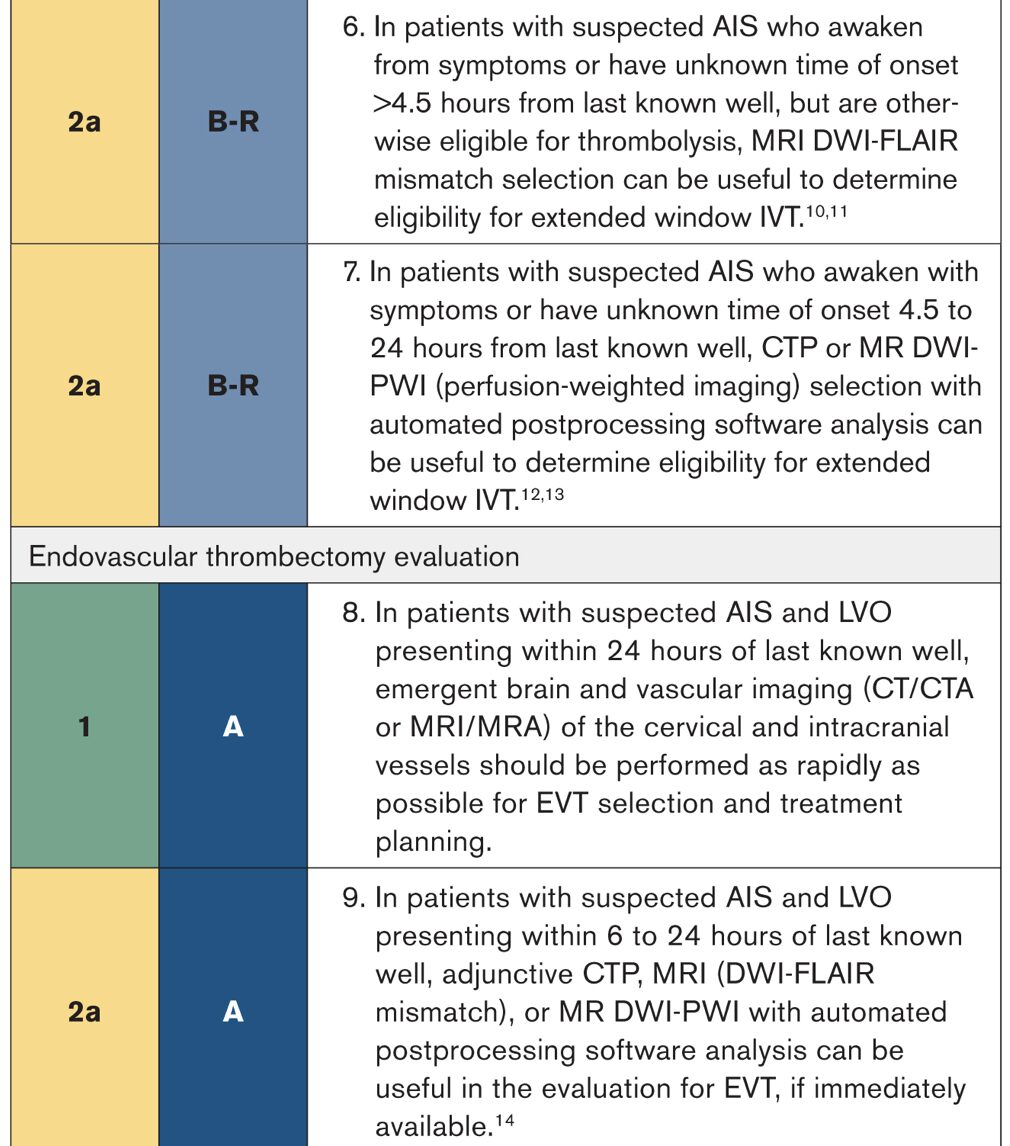
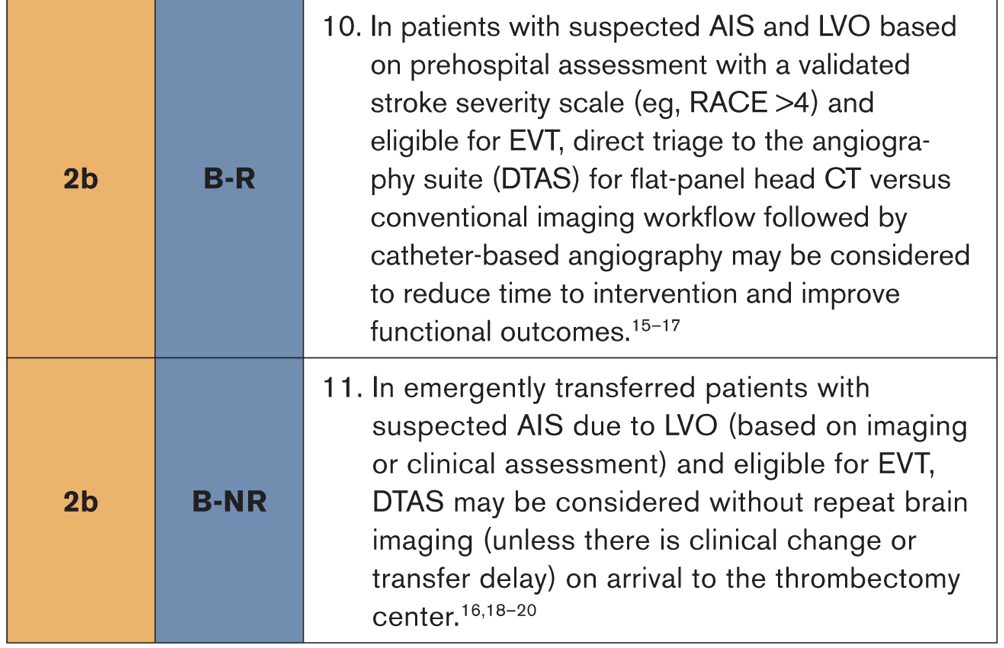
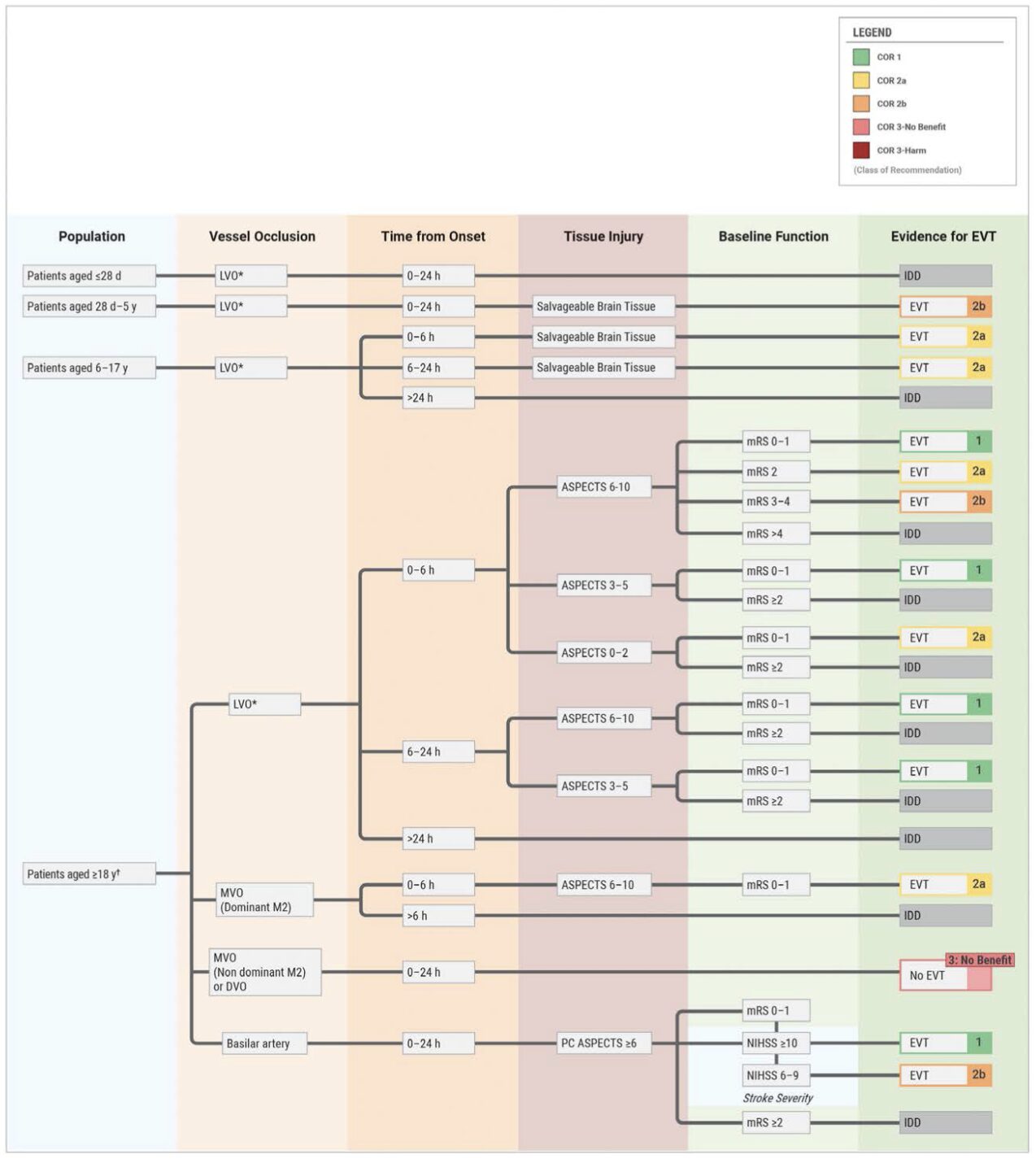
All recommendations are designated with a class of recommendation (COR) and level of evidence (LOE). COR is the strength of the recommendation, while the LOE is the quality of scientific evidence.
Key Updates
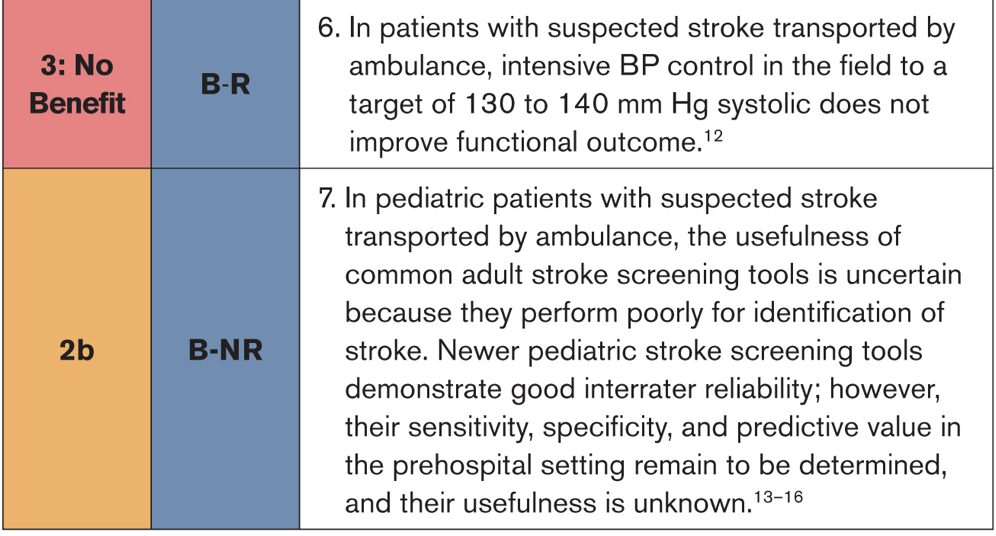
- 2.3. Prehospital Assessment and Management: COR 2b. In pediatric patients with suspected stroke transported by ambulance, the usefulness of common adult stroke screening tools is uncertain because they perform poorly for identification of stroke. Newer pediatric stroke screening tools demonstrate good interrater reliability; however, their sensitivity, specificity, and predictive value in the prehospital setting remain to be determined, and their usefulness is unknown.
- 3.2. Initial, Vascular, and Multimodal Imaging Approaches: COR 2a. In pediatric patients with suspected AIS, emergent brain and vascular imaging with MRI/MRA of the cervical and intracranial vessels is reasonable to identify patients with large vessel occlusion and to differentiate arterial ischemic stroke from hemorrhagic stroke or stroke mimics.
- 3.2. Initial, Vascular, and Multimodal Imaging Approaches: COR 2a. In pediatric patients with suspected AIS, emergent brain and vascular imaging with CT/CTA of the cervical and intracranial vessels is reasonable if MRI/MRA imaging is not available immediately (within 25 minutes) to identify patients with large vessel occlusion.
- 4.6.1. Thrombolysis Decision-Making: COR 2b. In pediatric patients aged 28 days to 18 years with confirmed AIS presenting within 4.5 hours of symptom onset and disabling deficits, IVT with alteplase may be considered as it is safe, but efficacy is uncertain.
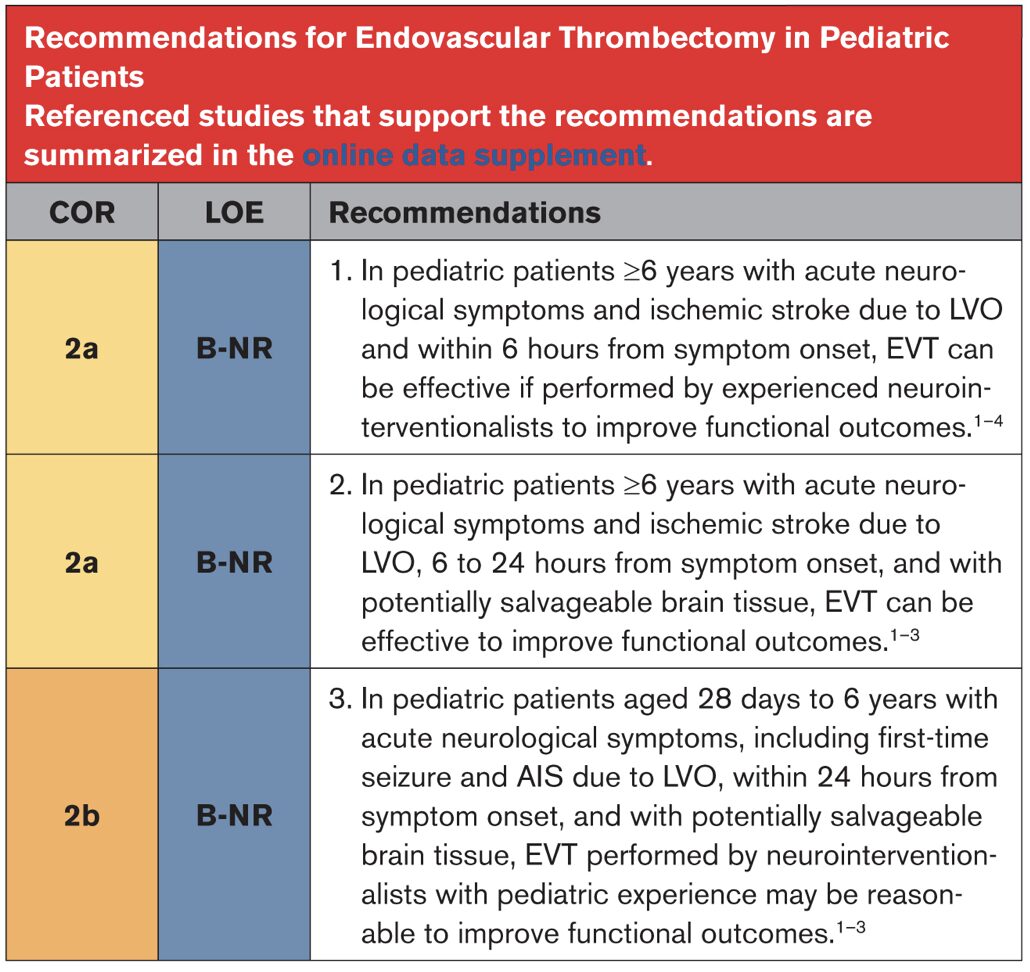
- 4.7.5. Endovascular Thrombectomy in Pediatric Patients: COR 2a. In pediatric patients ≥6 years with acute neurological symptoms and ischemic stroke due to LVO and within 6 hours from symptom onset, EVT can be effective if performed by experienced neurointerventionalists to improve functional outcomes.
- 4.7.5. Endovascular Thrombectomy in Pediatric Patients: COR 2a. In pediatric patients ≥6 years with acute neurological symptoms and ischemic stroke due to LVO, 6 to 24 hours from symptom onset, and with potentially salvageable brain tissue, EVT can be effective to improve functional outcomes.
- 4.7.5. Endovascular Thrombectomy in Pediatric Patients: COR 2b. In pediatric patients aged 28 days to 6 years with acute neurological symptoms, including first-time seizure and AIS due to LVO, within 24 hours from symptom onset, and with potentially salvageable brain tissue, EVT performed by neurointerventionalists with pediatric experience may be reasonable to improve functional outcomes.
General guideline updates:
- 2.9. Organization and Integration of Components: COR 1. Hospitals caring for patients with acute stroke that provide EVT (ie, TSC, CSC hospitals) should develop a system to comprehensively track key time metrics and other care processes relevant to thrombectomy (eg, door-to-puncture time, successful reperfusion), as well as long-term patient outcomes.
- 2.9. Organization and Integration of Components: COR 1. Hospitals caring for patients with acute stroke that provide EVT (ie, TSC, CSC hospitals) should credential neurointerventionalists using established and agreed upon training and certification standards.
- 3.2. Initial, Vascular, and Multimodal Imaging Approaches: COR 1: In patients with suspected AIS and LVO, emergent vascular imaging with contrast-enhanced CTA and/or CTP should not be delayed to obtain serum creatinine concentration.
- 3.2. Initial, Vascular, and Multimodal Imaging Approaches: COR 2a: In patients with suspected AIS who awaken from symptoms or have unknown time of onset >4.5 hours from last known well, but are otherwise eligible for thrombolysis, MRI DWI-FLAIR mismatch selection can be useful to determine eligibility for extended window IVT.
- 3.2. Initial, Vascular, and Multimodal Imaging Approaches: COR 1: In patients with suspected AIS and LVO presenting within 24 hours of last known well, emergent brain and vascular imaging (CT/CTA or MRI/MRA) of the cervical and intracranial vessels should be performed as rapidly as possible for EVT selection and treatment planning.
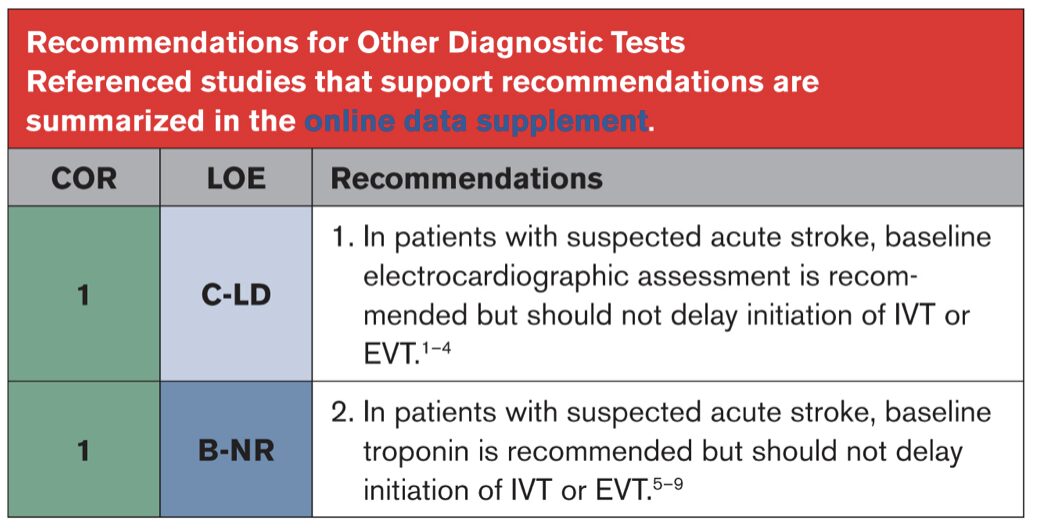
- 3.3. Other Diagnostic Tests: COR 1: In patients with suspected acute stroke, baseline electrocardiographic assessment is recommended but should not delay initiation of IVT or EVT.
- 3.3. Other Diagnostic Tests: COR 1: In patients with suspected acute stroke, baseline troponin is recommended but should not delay initiation of IVT or EVT.
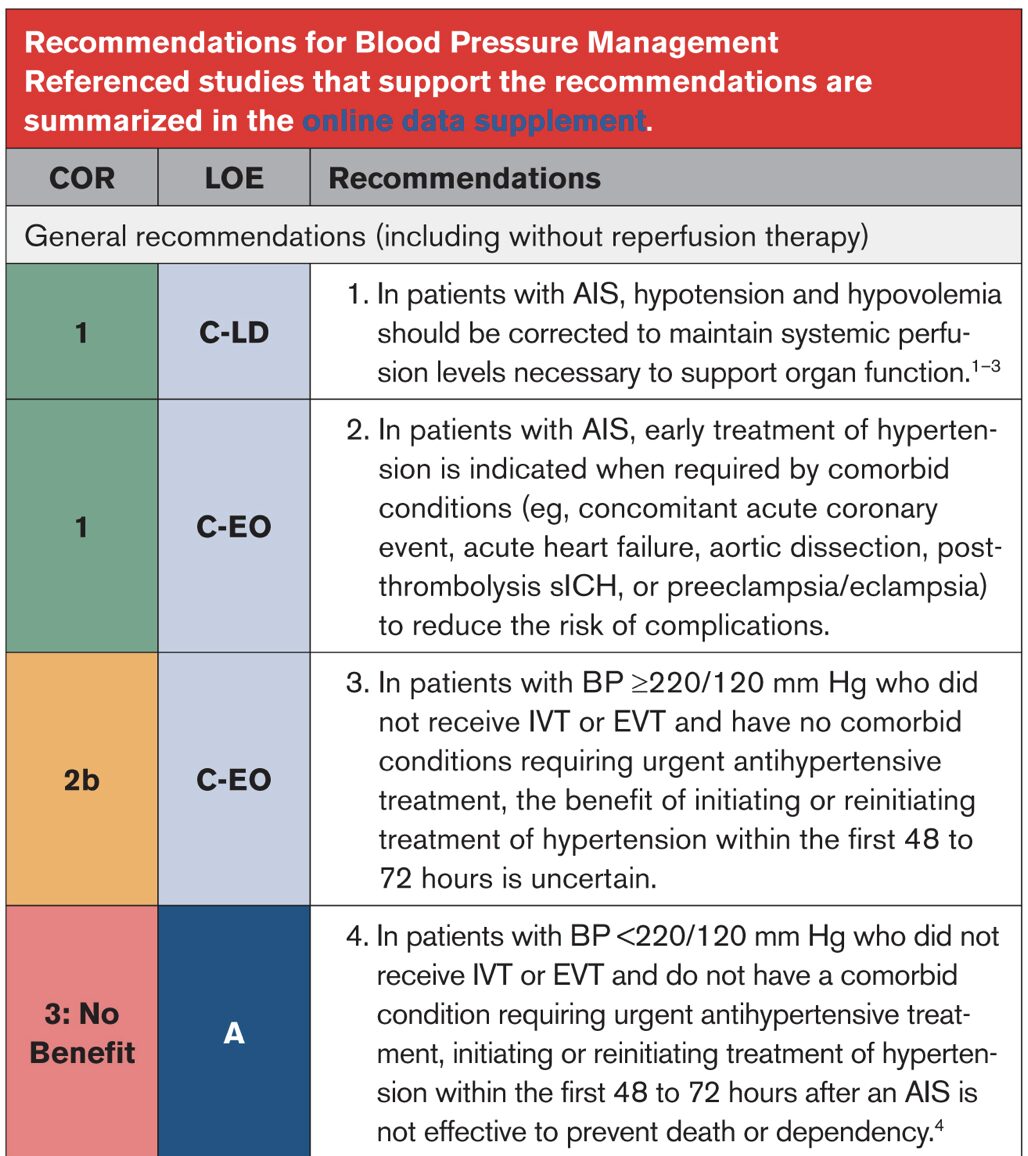
- 4.3. Blood Pressure Management: COR 3: No Benefit. In patients with mild to moderate severity AIS who have been treated with IVT, intensive SBP reduction (target of <140 mm Hg compared with <180 mm Hg) is not recommended because it is not associated with an improvement in functional outcome.
- 4.3. Blood Pressure Management: COR 3: Harm. In patients with AIS with LVO of the anterior circulation who have been successfully recanalized by endovascular therapy (mTICI 2b, 2c, or 3) and without other indication for blood pressure management target, intensive SBP reduction target of <140 mm Hg for the first 72 hours is harmful and not recommended.
- 4.5. Blood Glucose Management: COR 3: No Benefit. In hospitalized patients with AIS with hyperglycemia, treatment with IV insulin to achieve blood glucose levels in the range of 80 to 130 mg/dL is not recommended to improve 3-month functional outcomes.
- 4.6.1. Thrombolysis Decision-Making: COR 1. In adult patients with AIS who are eligible for IVT within 4.5 hours of symptom onset, treatment should be initiated as quickly as possible, assuring safe administration and avoiding potential delays associated with additional multimodal neuroimaging, such as CTA/MRA, and CT/MR perfusion imaging.
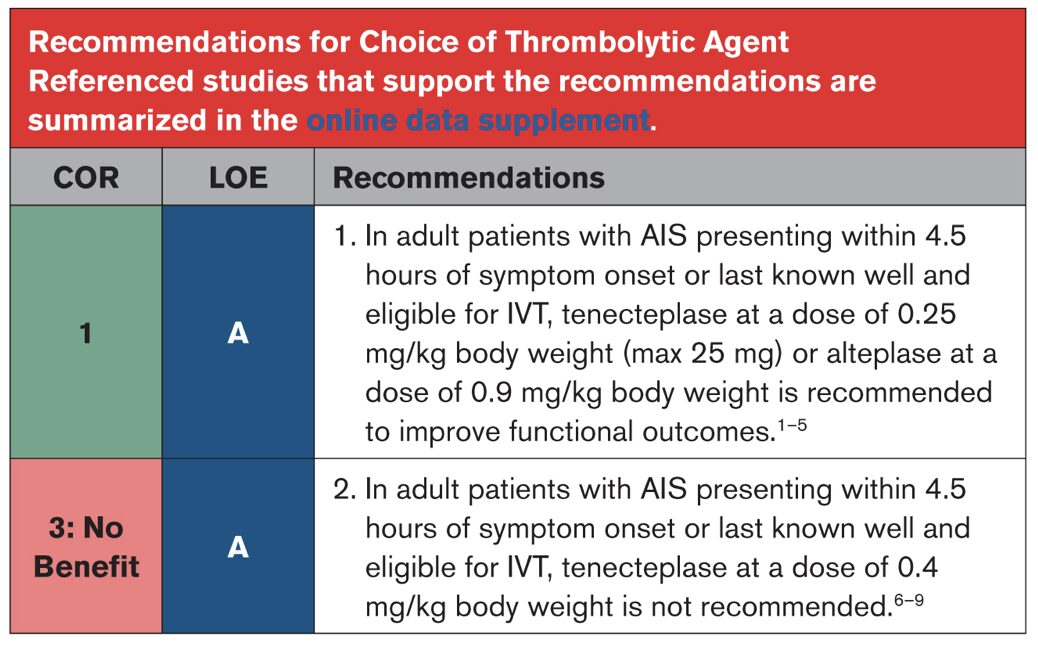
- 4.6.2. Choice of Thrombolytic Agent: COR 1. In adult patients with AIS presenting within 4.5 hours of symptom onset or last known well and eligible for IVT, tenecteplase at a dose of 0.25 mg/kg body weight (max 25 mg) or alteplase at a dose of 0.9 mg/kg body weight is recommended to improve functional outcomes.
- 4.6.3. Extended Time Windows for Intravenous Thrombolysis: COR 2a. In patients with AIS who have salvageable ischemic penumbra detected on automated perfusion imaging and who (a) awake with stroke symptoms within 9 hours from the midpoint of sleep or (b) are 4.5–9 hours from last known well, IV thrombolysis may be reasonable to improve functional outcomes.
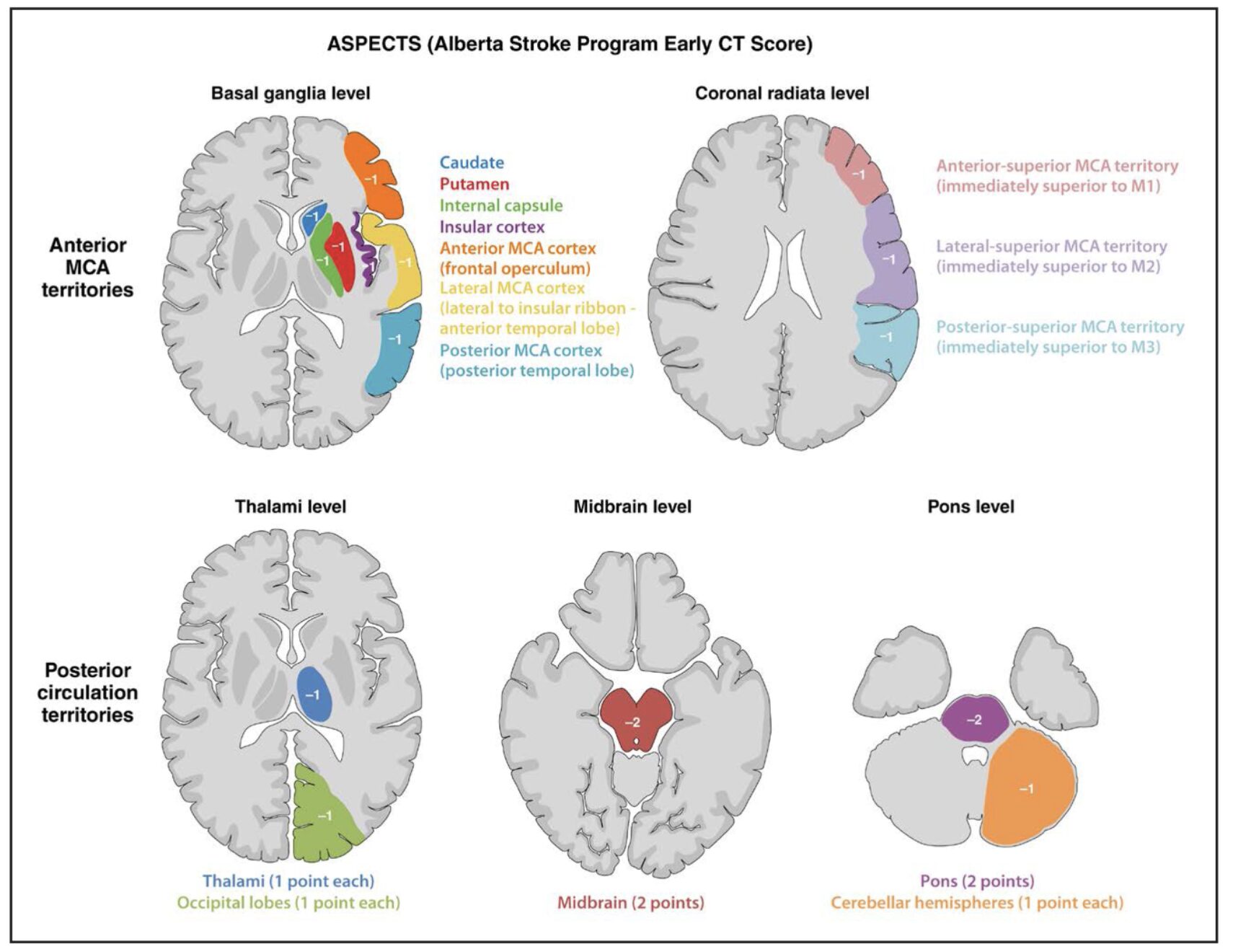
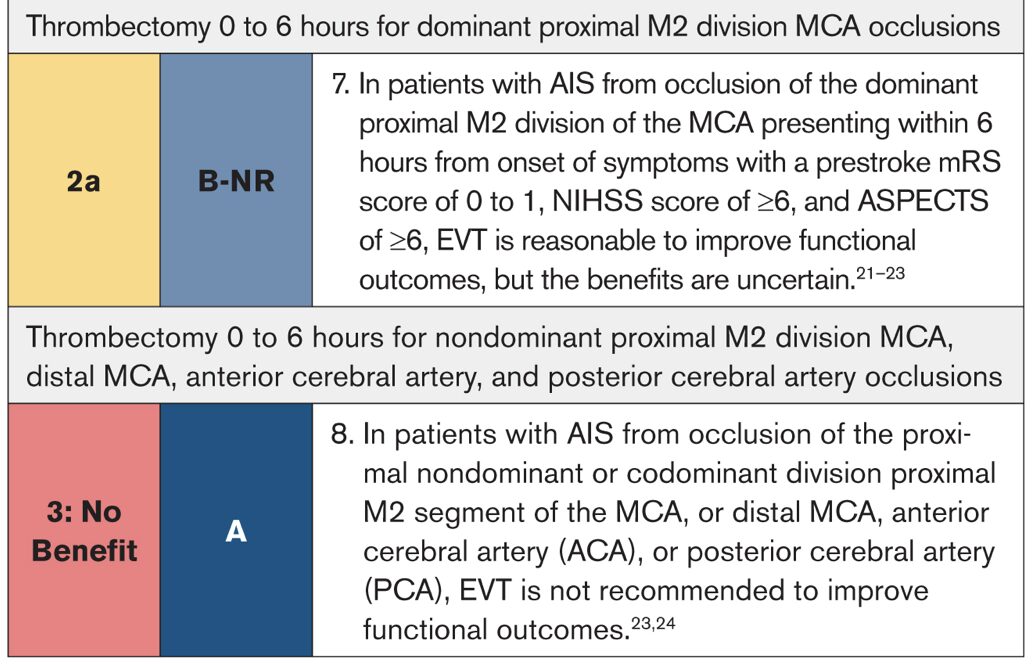
- 4.7.2. Endovascular Thrombectomy for Adults: COR 1. In patients with AIS from anterior circulation proximal LVO of the ICA or M1, presenting within 6 hours from onset of symptoms, with NIHSS score ≥6, prestroke mRS score of 0 to 1, and ASPECTS 3 to 10, EVT is recommended to improve functional clinical outcomes and reduce mortality.
- 4.7.2. Endovascular Thrombectomy for Adults: COR 1. In selected patients* with AIS from anterior circulation proximal LVO of the ICA or M1, presenting between 6 and 24 hours from onset of symptoms, with age <80 years, NIHSS score ≥6, prestroke mRS score 0 to 1, ASPECTS 3 to 5, and without significant mass effect on imaging, EVT is recommended to improve functional clinical outcomes and reduce mortality.
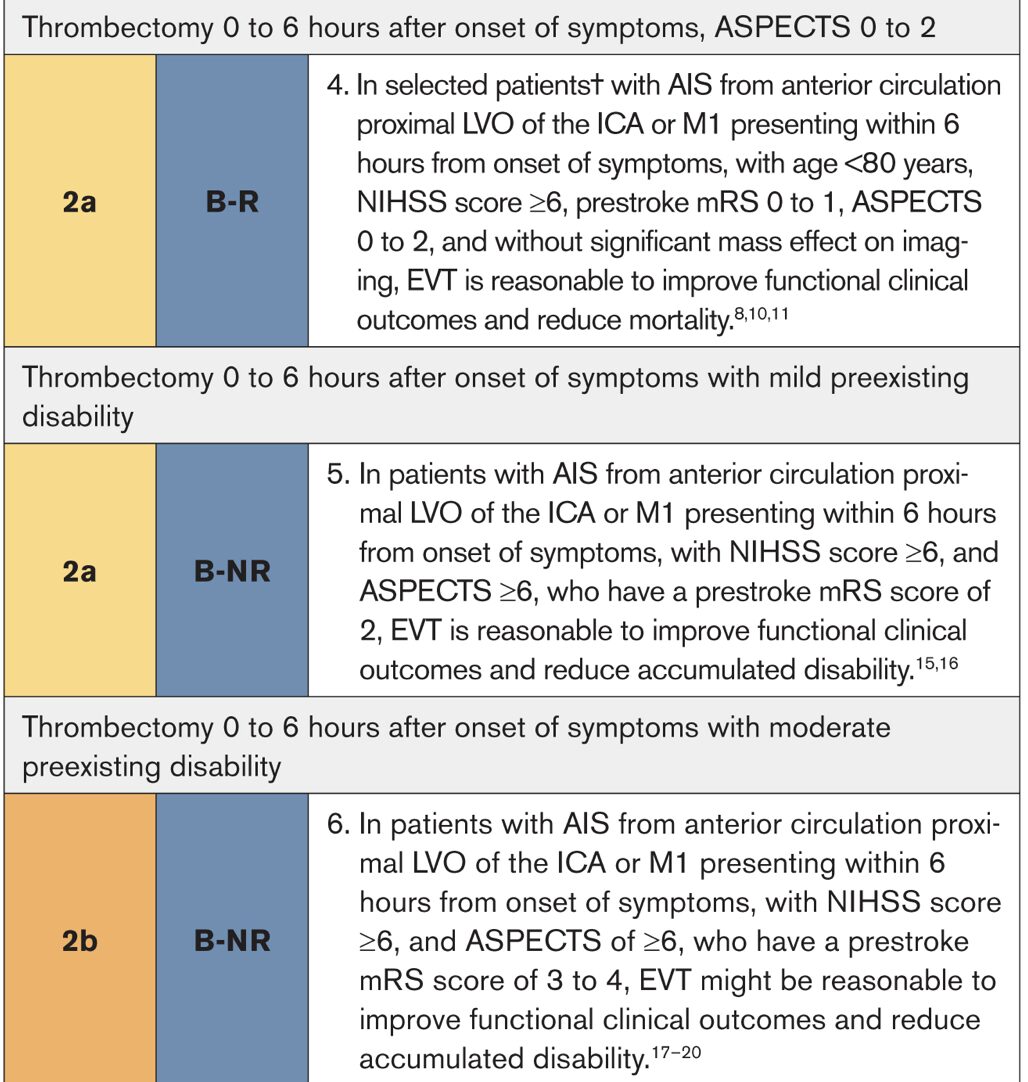
- 4.7.2. Endovascular Thrombectomy for Adults: COR 2a. In selected patients† with AIS from anterior circulation proximal LVO of the ICA or M1 presenting within 6 hours from onset of symptoms, with age <80 years, NIHSS score ≥6, prestroke mRS 0 to 1, ASPECTS 0 to 2, and without significant mass effect on imaging, EVT is reasonable to improve functional clinical outcomes and reduce mortality.
- 4.7.2. Endovascular Thrombectomy for Adults: COR 2a. In patients with AIS from anterior circulation proximal LVO of the ICA or M1 presenting within 6 hours from onset of symptoms, with NIHSS score ≥6, and ASPECTS ≥6, who have a prestroke mRS score of 2, EVT is reasonable to improve functional clinical outcomes and reduce accumulated disability.
- 4.7.3. Posterior Circulation Stroke: COR 1. In patients with AIS, with basilar artery occlusion, a baseline mRS score of 0 to 1, NIHSS score ≥10 at presentation, and PC-ASPECTS ≥6 (mild ischemic damage), EVT within 24 hours from onset of symptoms is recommended to achieve better functional outcome and reduce mortality.
- 4.7.4. Endovascular Techniques: COR 3: No Benefit. In the management of patients with AIS in the setting of LVO, preoperative administration of tirofiban before EVT is not useful to improve 90-day functional outcome.
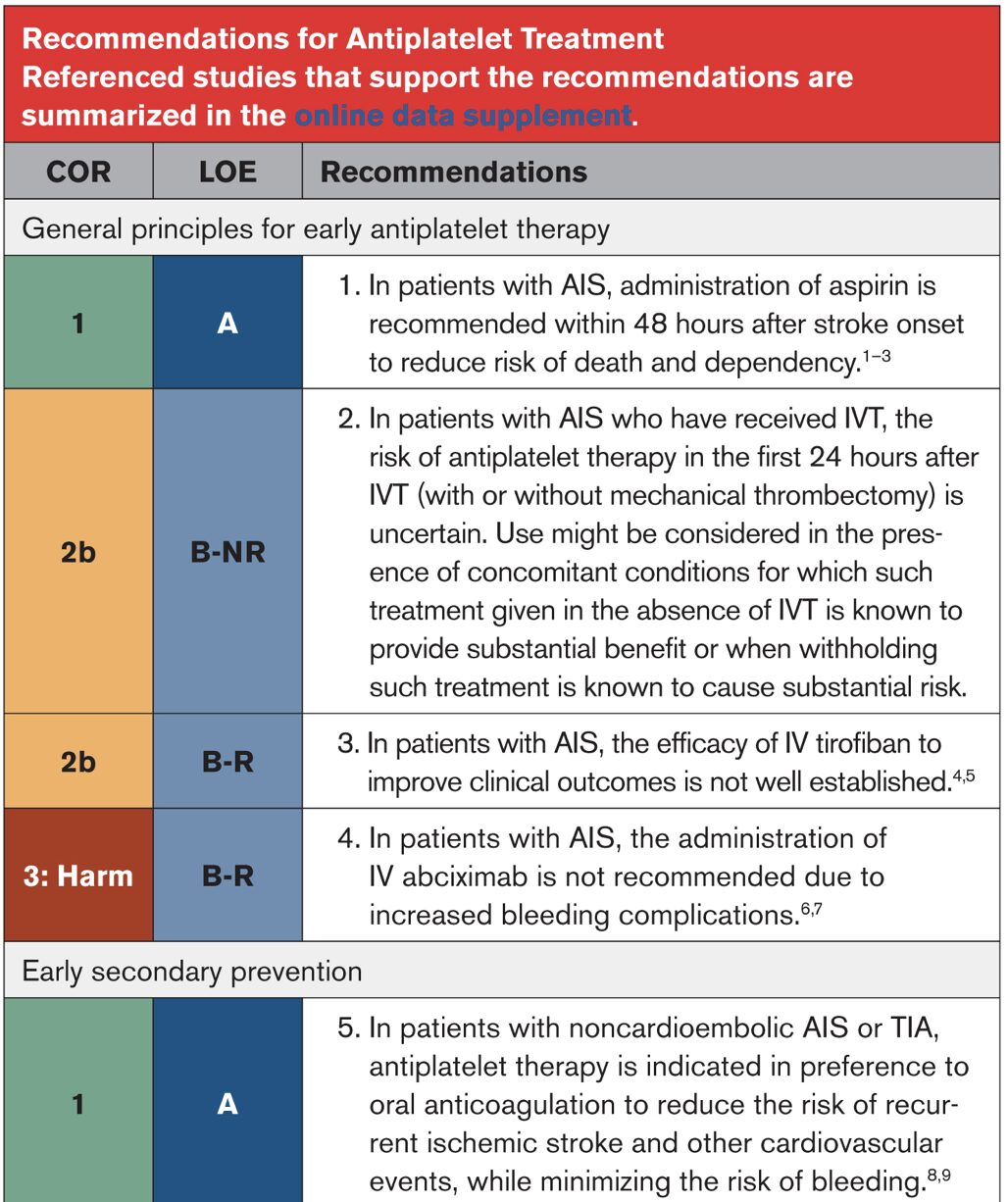
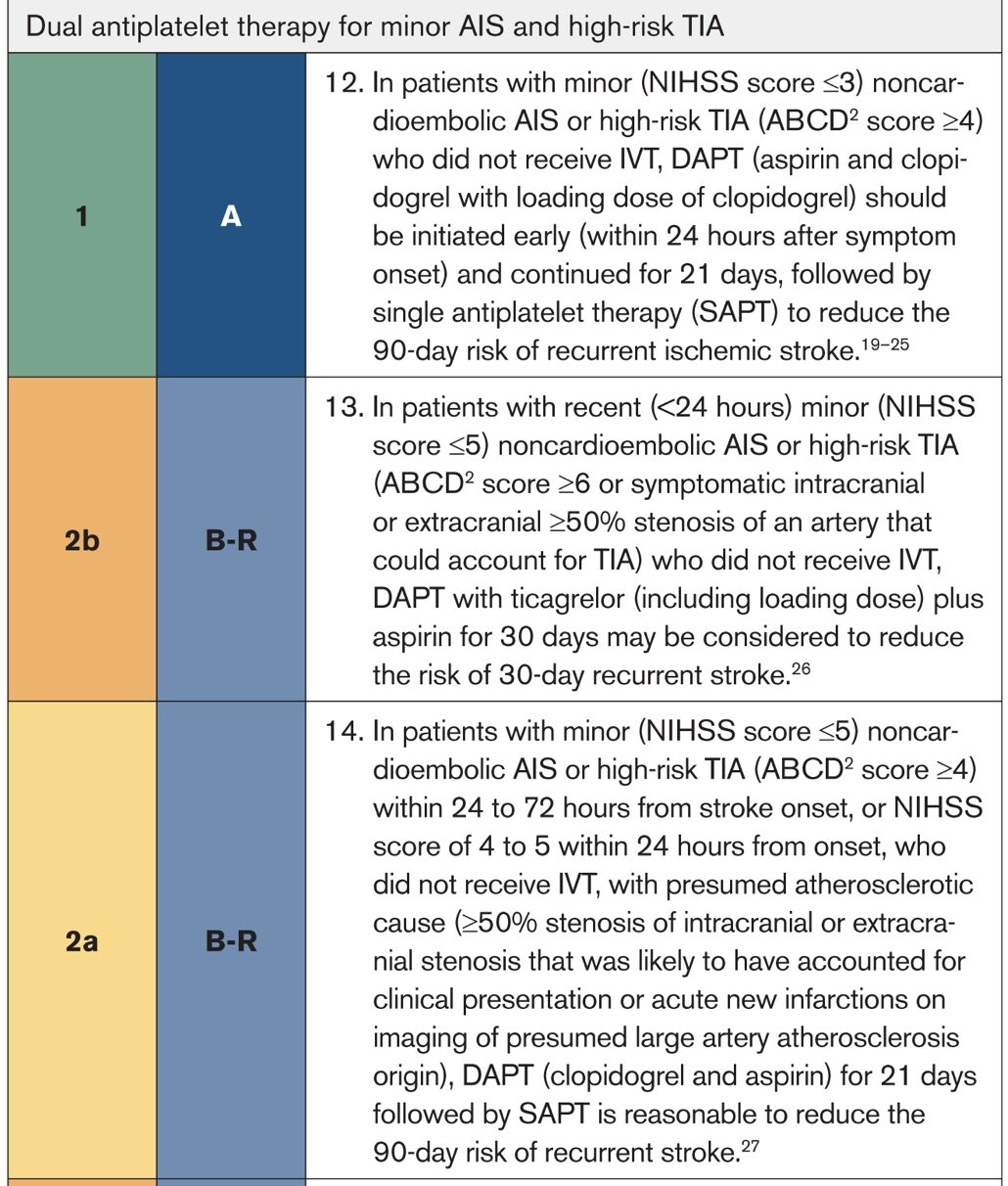
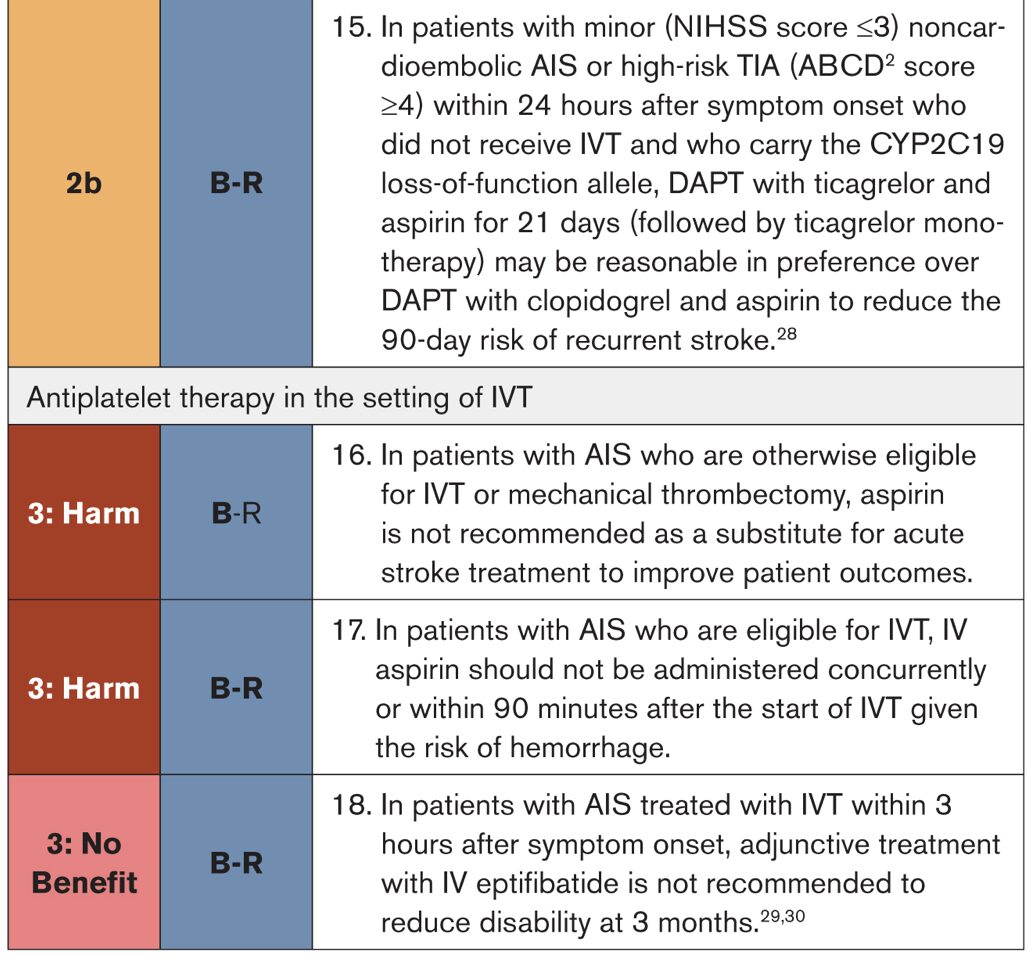
- 4.8. Antiplatelet Treatment: COR 2a. In patients with minor (NIHSS score ≤5) noncardioembolic AIS or high-risk TIA (ABCD2 score ≥4) within 24 to 72 hours from stroke onset, or NIHSS score of 4 to 5 within 24 hours from onset, who did not receive IVT, with presumed atherosclerotic cause (≥50% stenosis of intracranial or extracranial stenosis that was likely to have accounted for clinical presentation or acute new infarctions on imaging of presumed large artery atherosclerosis origin), DAPT (clopidogrel and aspirin) for 21 days followed by SAPT is reasonable to reduce the 90-day risk of recurrent stroke.
- 4.9. Anticoagulants: COR 2a. In carefully selected (eg, milder severity) patients with AIS with atrial fibrillation, a strategy of early oral anticoagulation poststroke is low risk and is reasonable compared with a strategy of delayed anticoagulation, although the efficacy of early anticoagulation for prevention of early recurrent stroke is not established.
Abbreviations/Notes:
- AIS indicates acute ischemic stroke; CT, computed tomography; CTA, computed tomography angiography; CSC, comprehensive stroke center; DAPT, dual antiplatelet therapy; DIDO, door-in-door-out (time metric for stroke transfers); EMS, emergency medical services; EVT, endovascular thrombectomy; ICA, internal carotid artery; IV, intravenous; IVT, intravenous thrombolysis; LVO, large vessel occlusion; MRA, magnetic resonance angiography; MRI, magnetic resonance imaging; mTICI, modified thrombolysis in cerebral infarction (scale for reperfusion success); NIHSS, National Institutes of Health Stroke Scale; SAPT, single antiplatelet therapy; SBP, systolic blood pressure; SSOC, stroke system of care; TIA, transient ischemic attack; and TSC, thrombectomy-capable stroke center
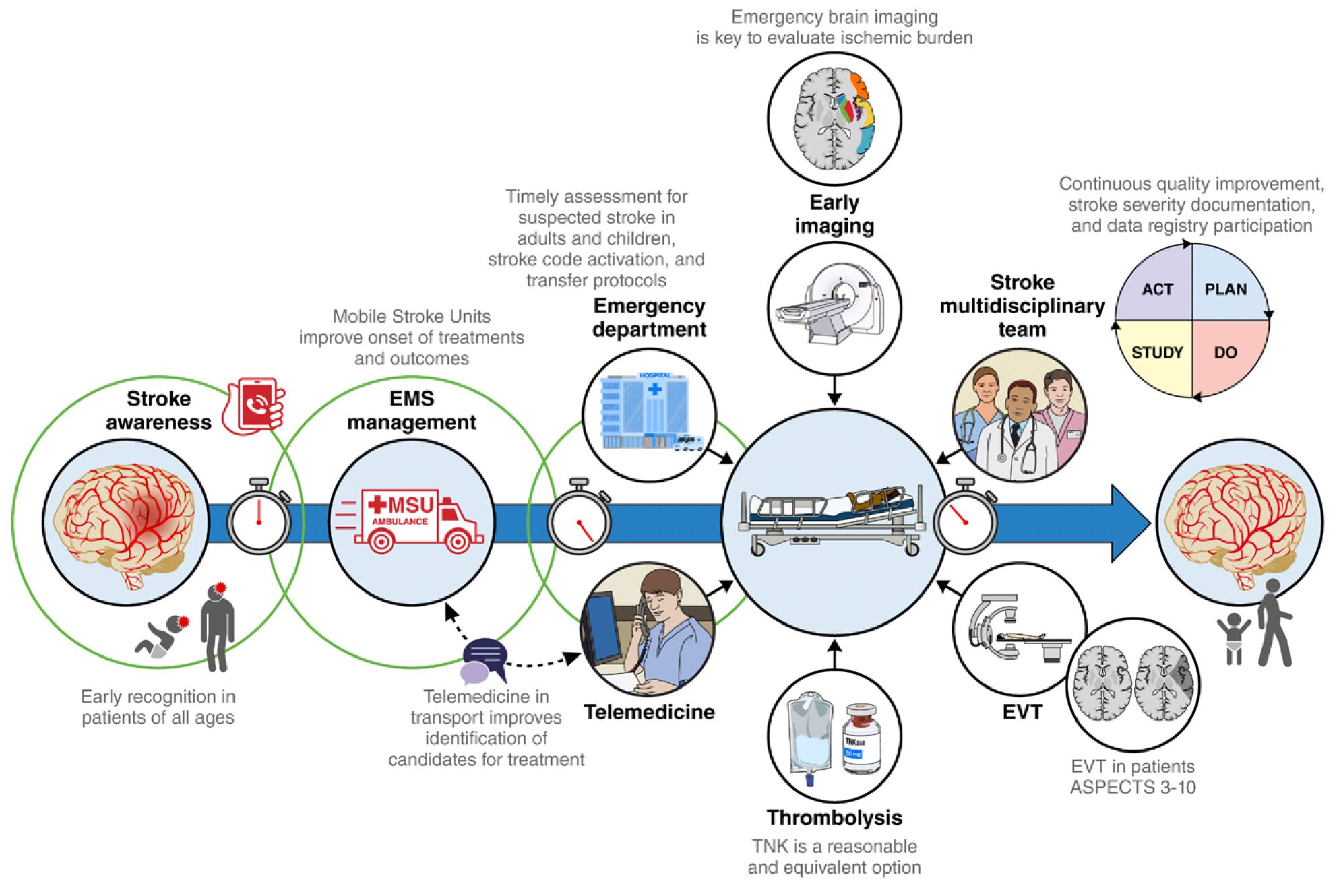
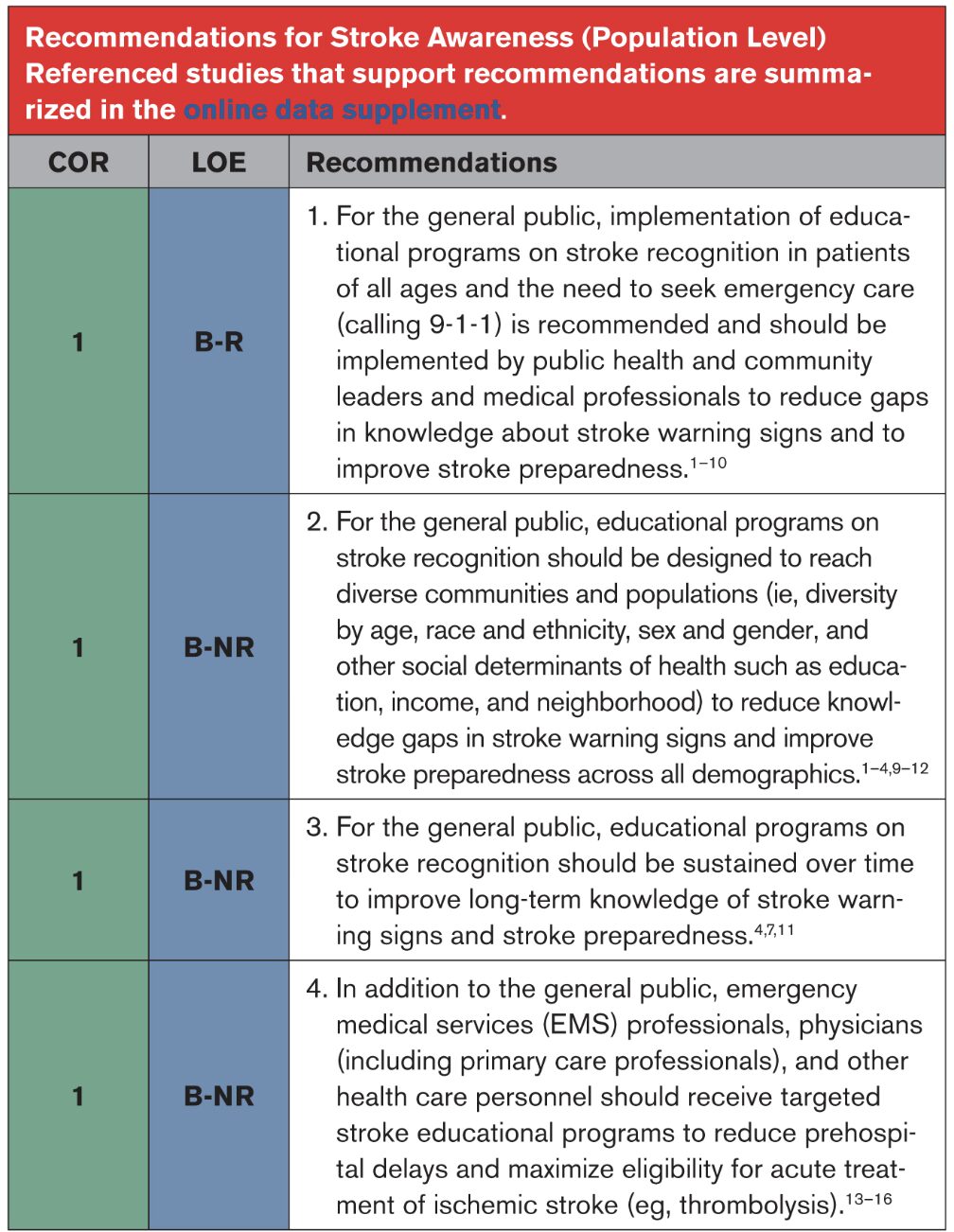
2.1 Stroke Awareness (General Population)
2.2 EMS Systems
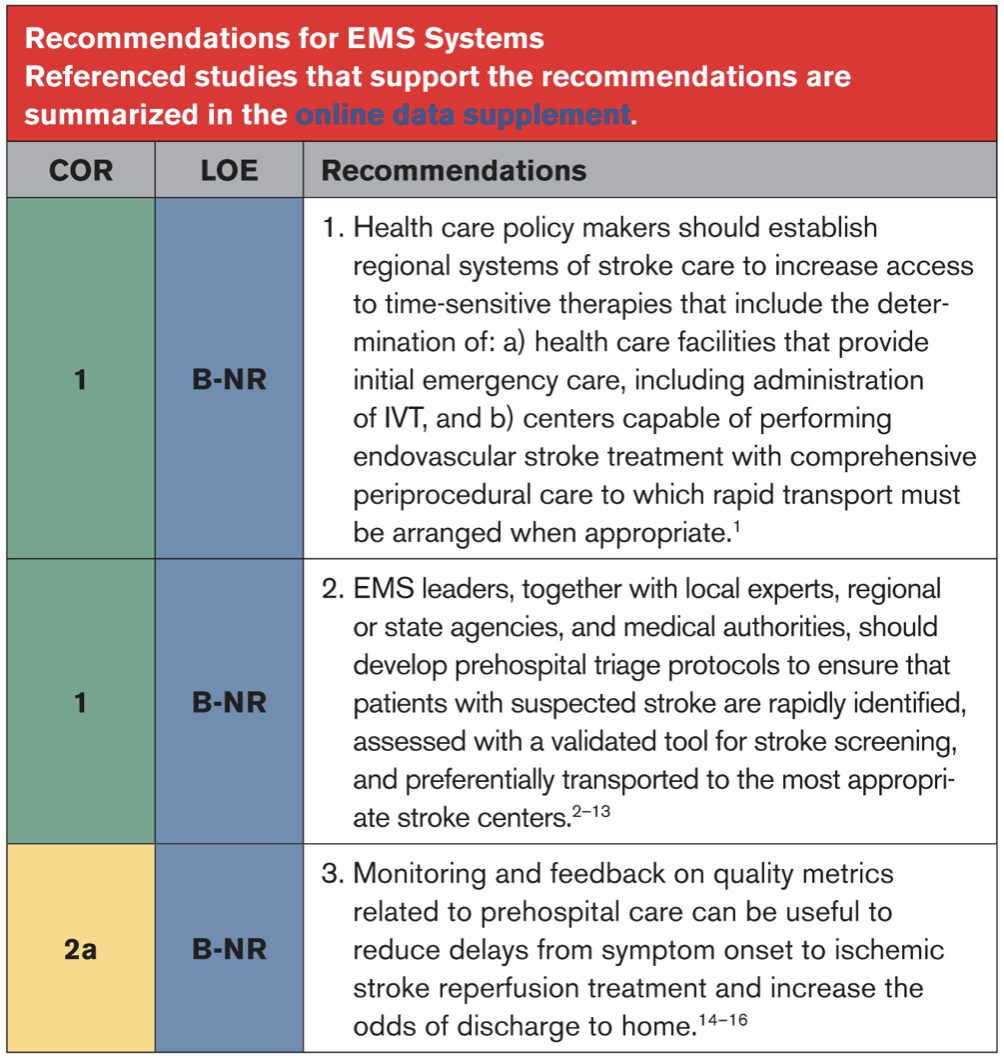
2.3 Prehospital Assessment and Management

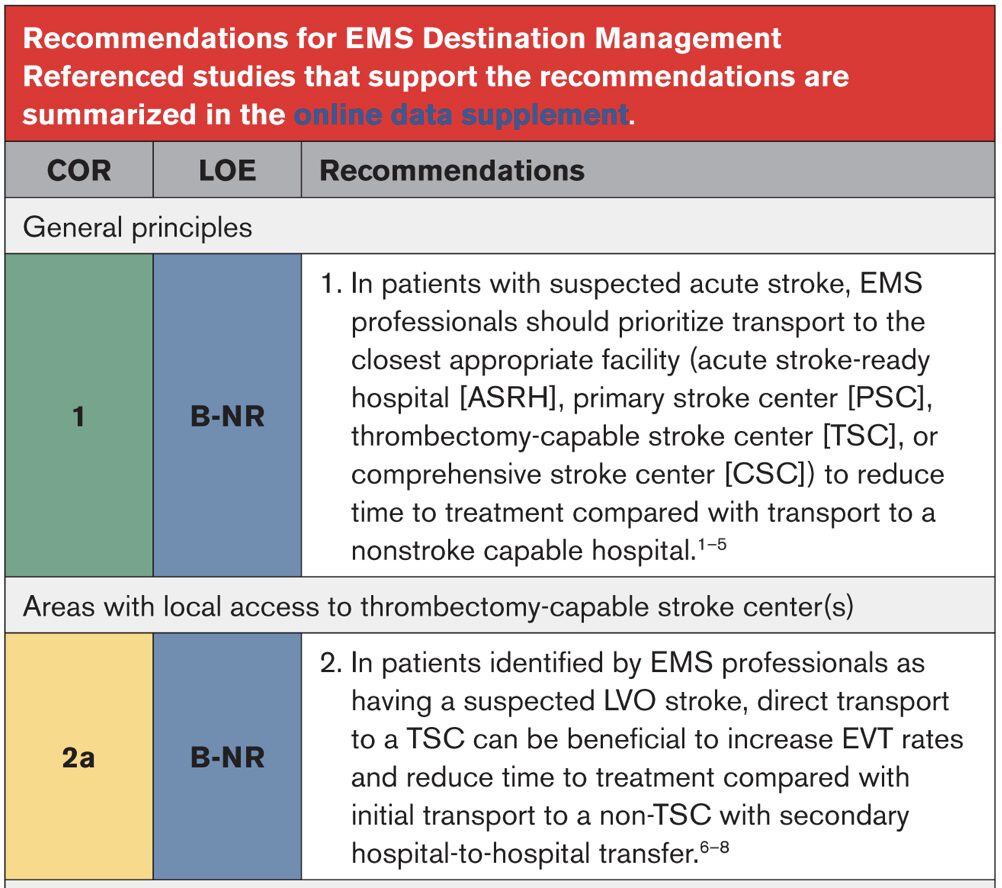
2.4 EMS Destination Management
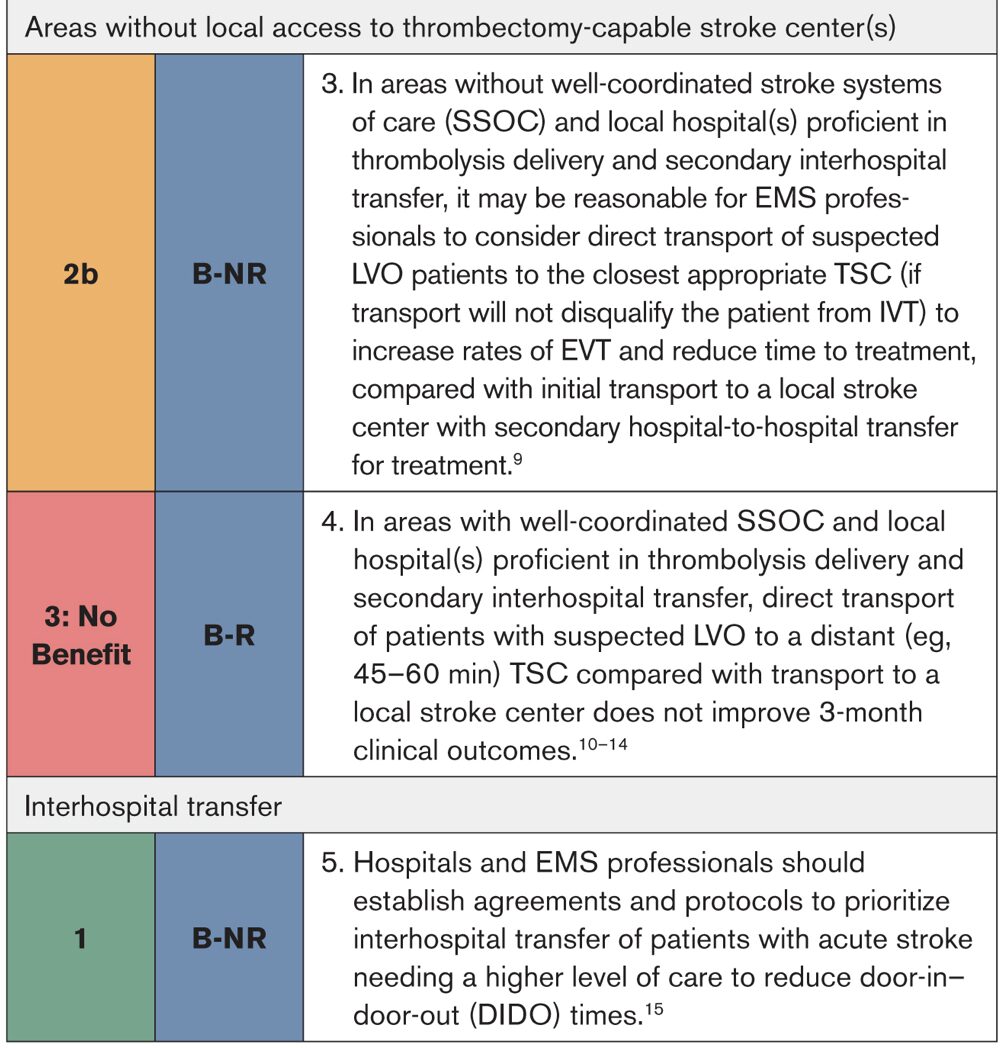
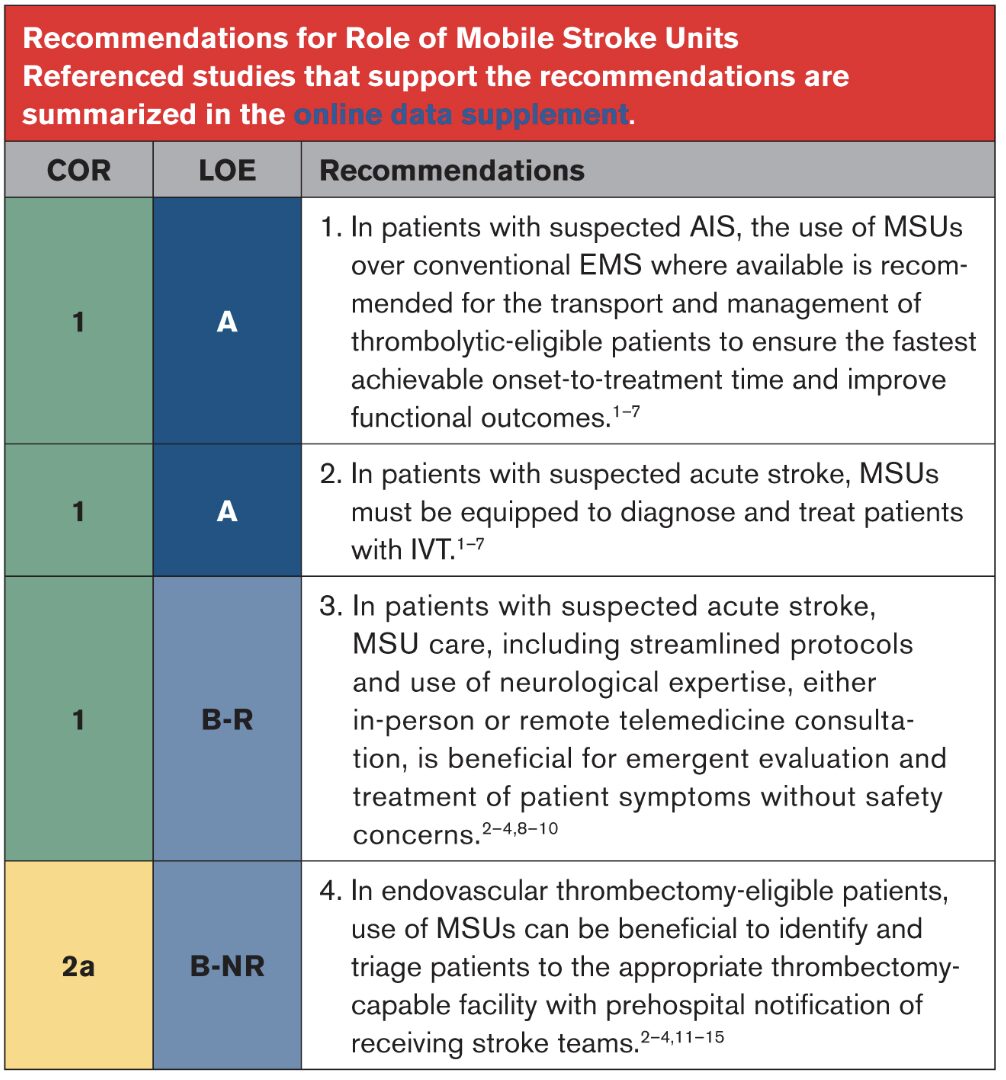
2.5 Role of Mobile Stroke Units
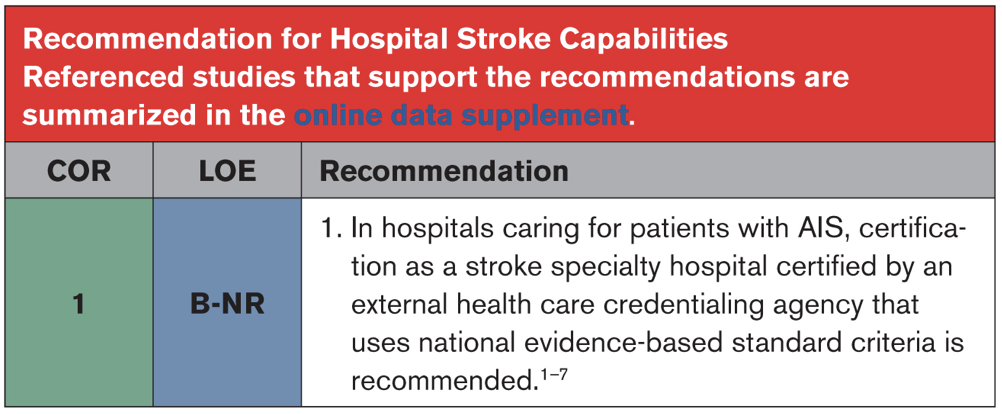
2.6 Hospital Stroke Capabilities
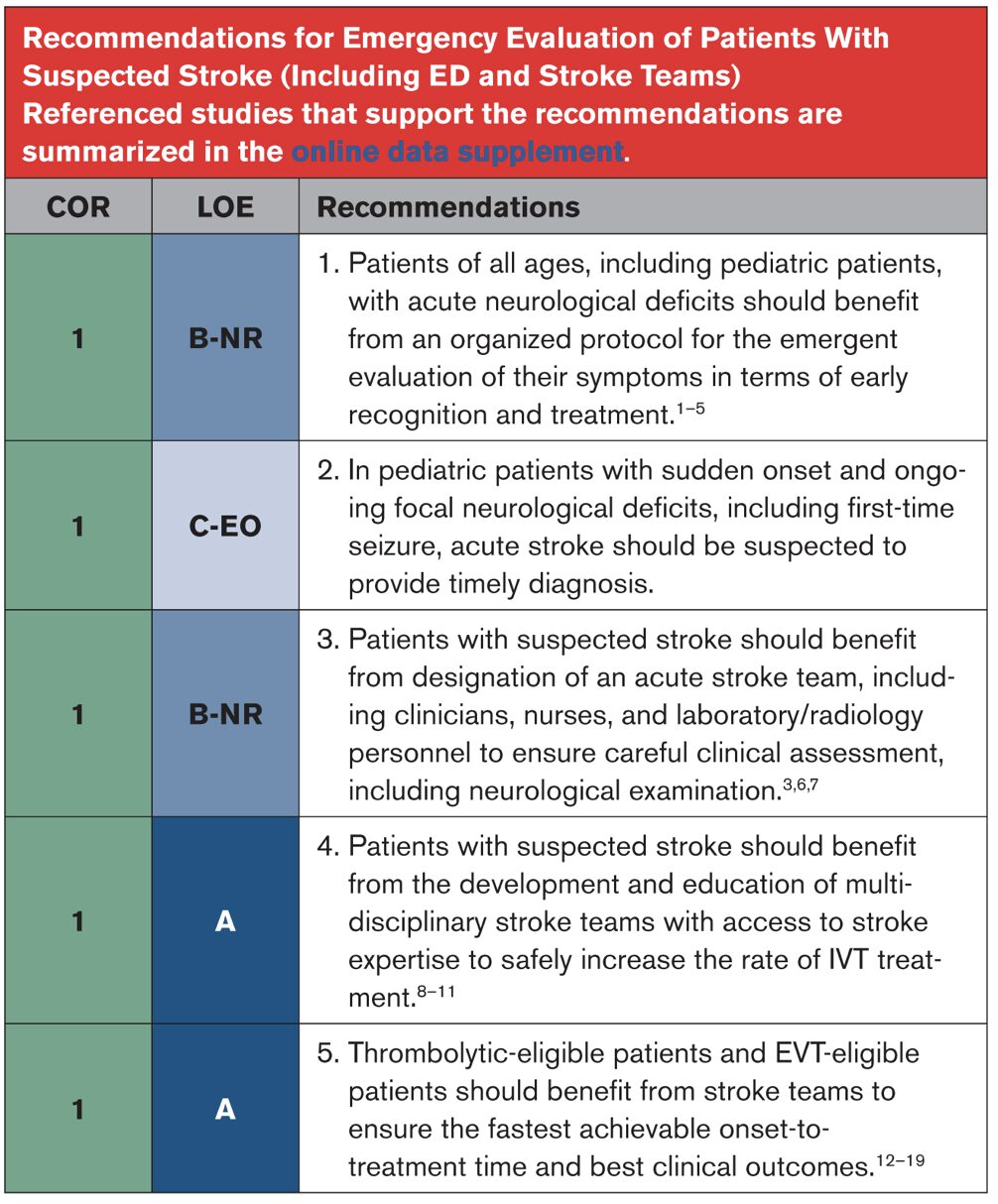
2.7 Emergency Evaluation of Patients With Suspected Stroke (Including ED and Stroke Teams)
2.8 Telemedicine

2.9 Organization and Integration of Components
2.10 Stroke Registries, Quality Improvement, and Risk Adjustment

3.1 Stroke Scales

3.2 Initial, Vascular, and Multimodal Imaging Approaches
3.3 Other Diagnostic Tests
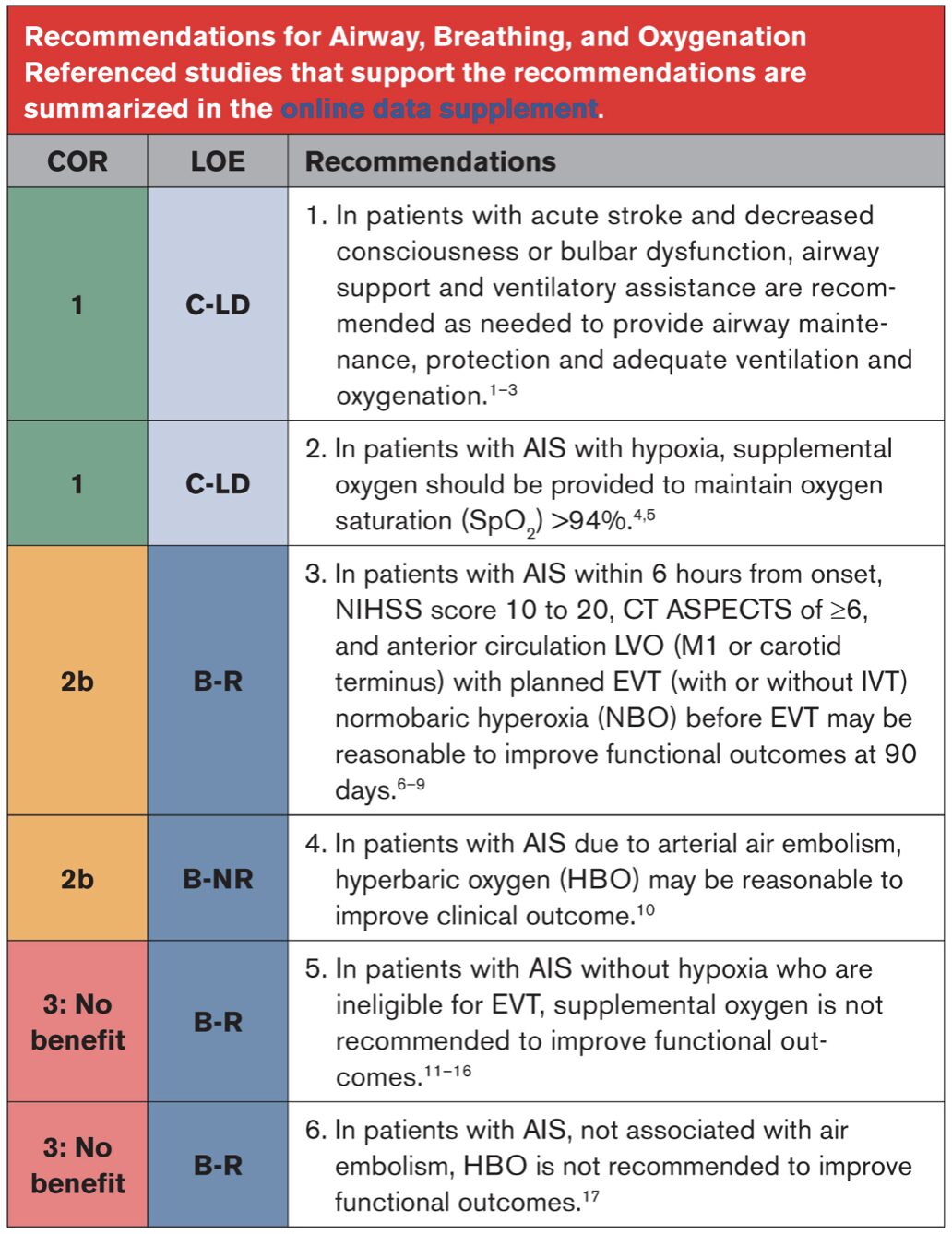
4.1 Airway, Breathing, and Oxygenation
4.2 Head Positioning
4.3 Blood Pressure Management

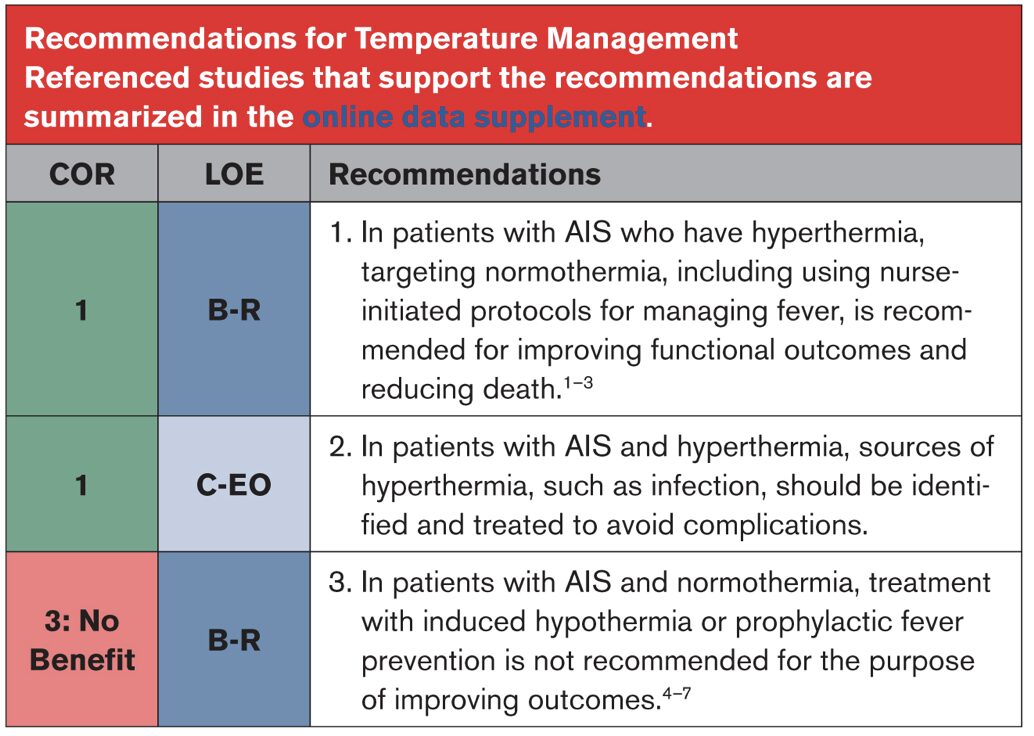
4.4 Temperature Management
4.5 Blood Glucose Management

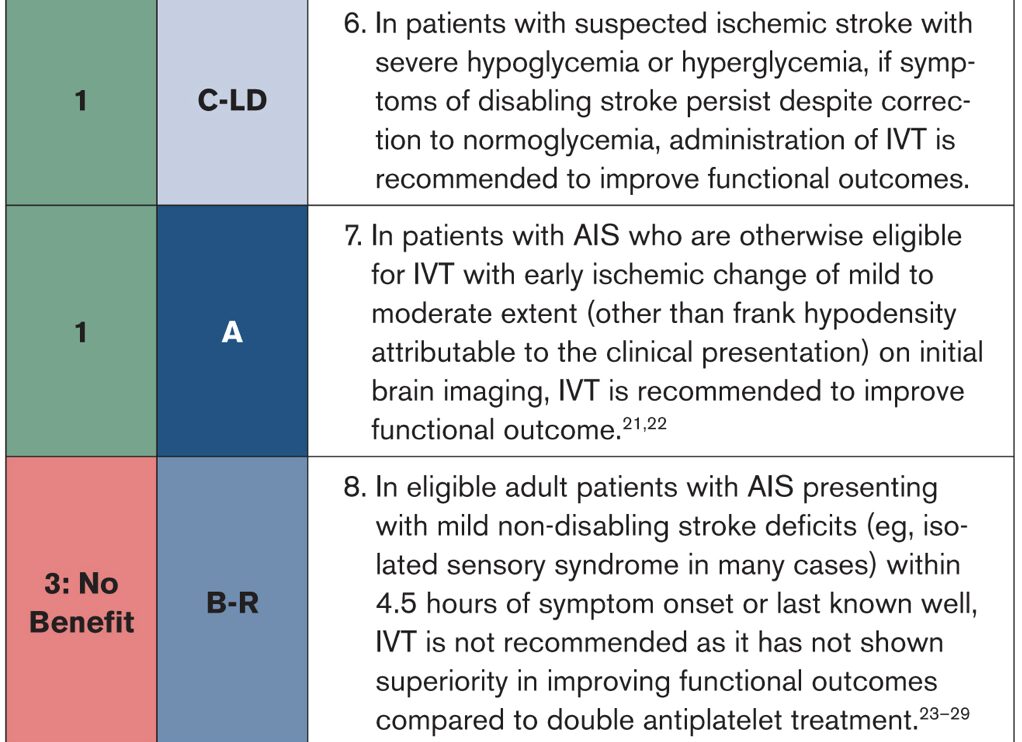
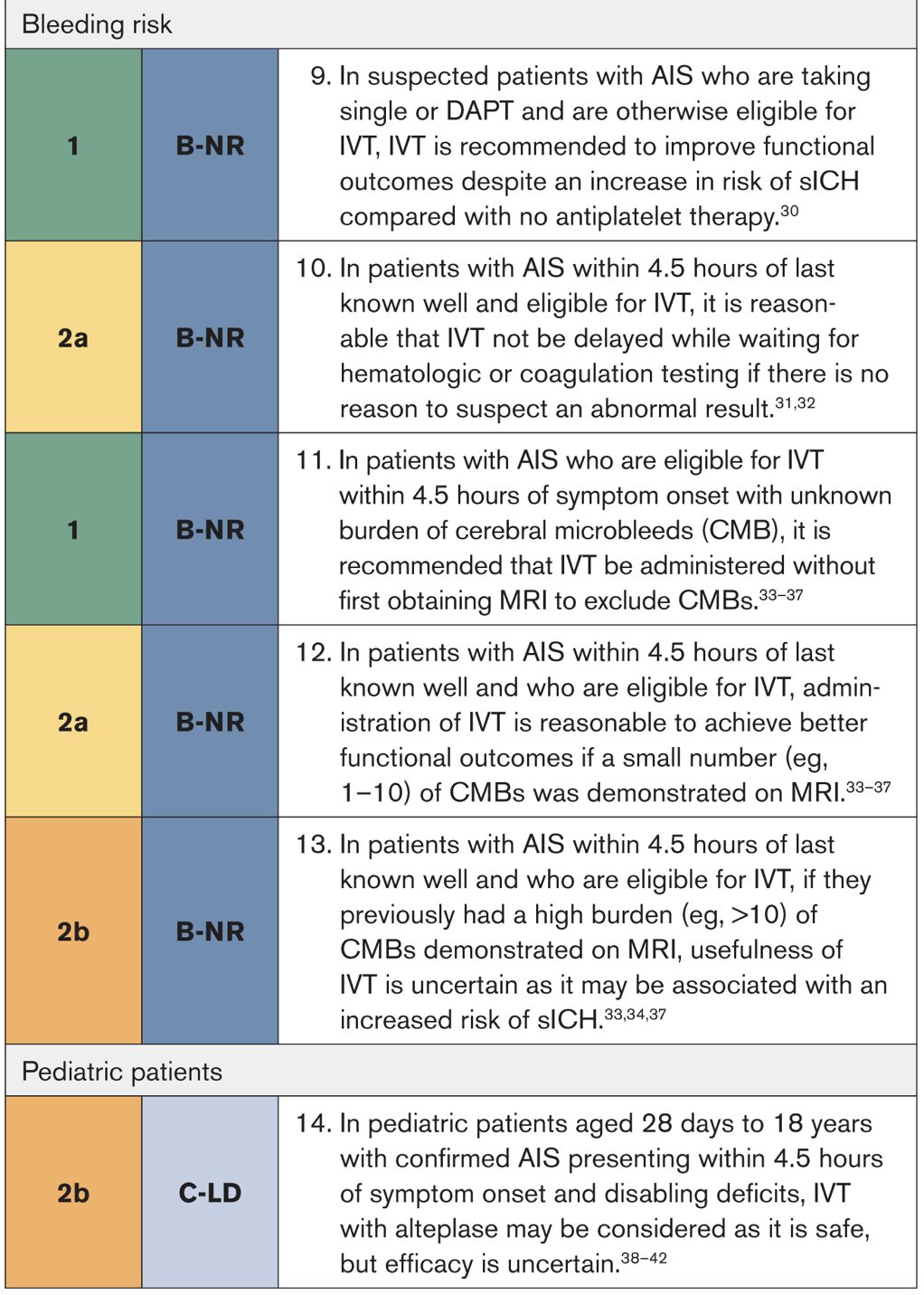
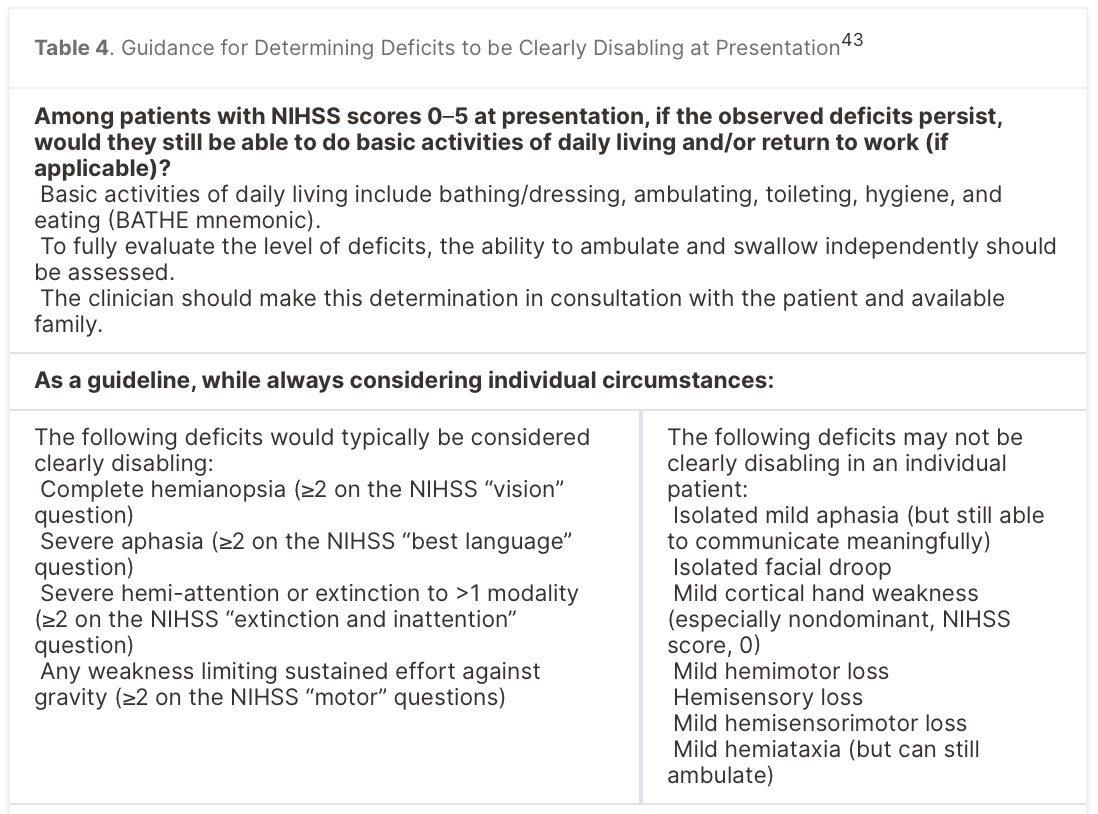
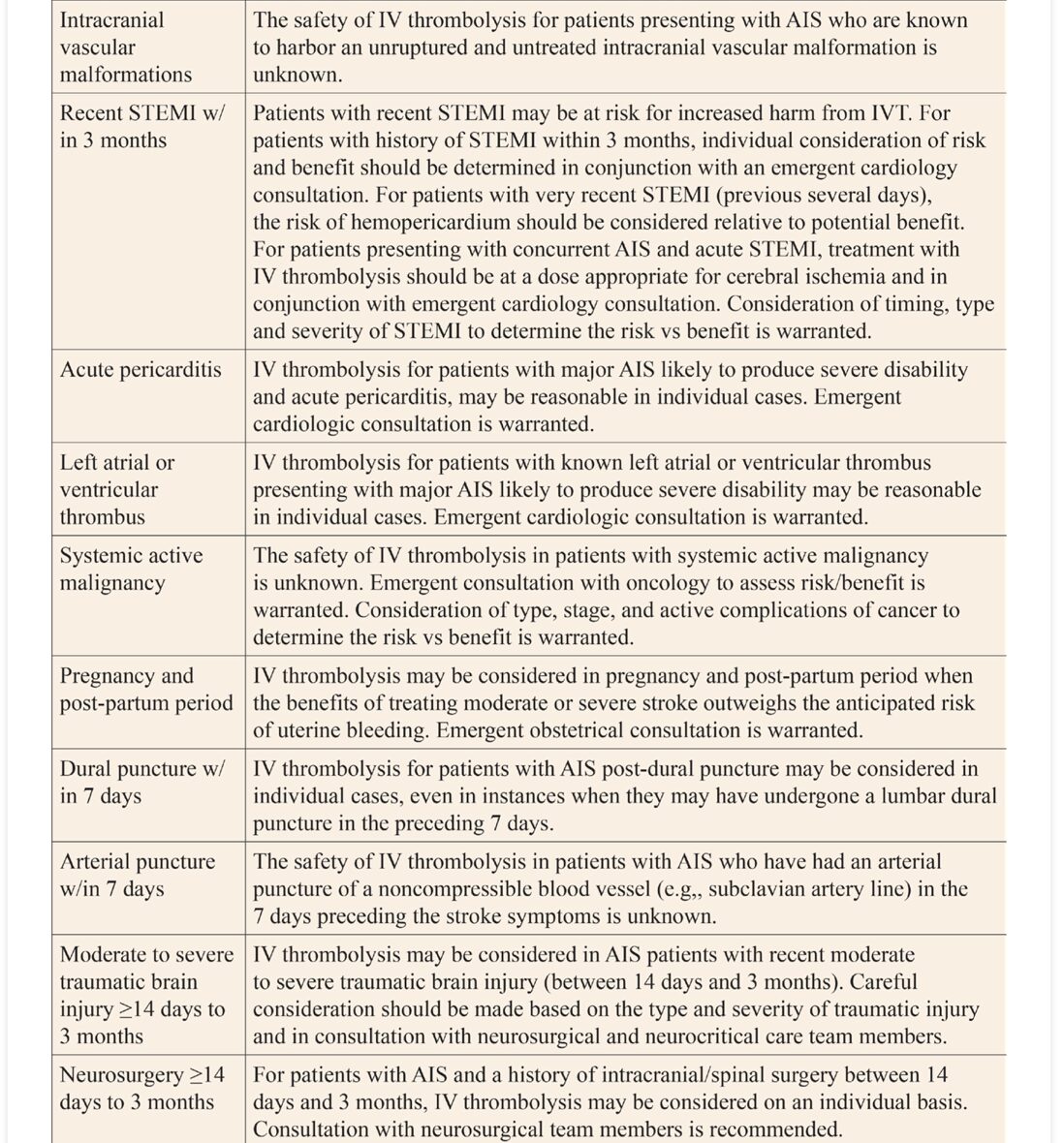
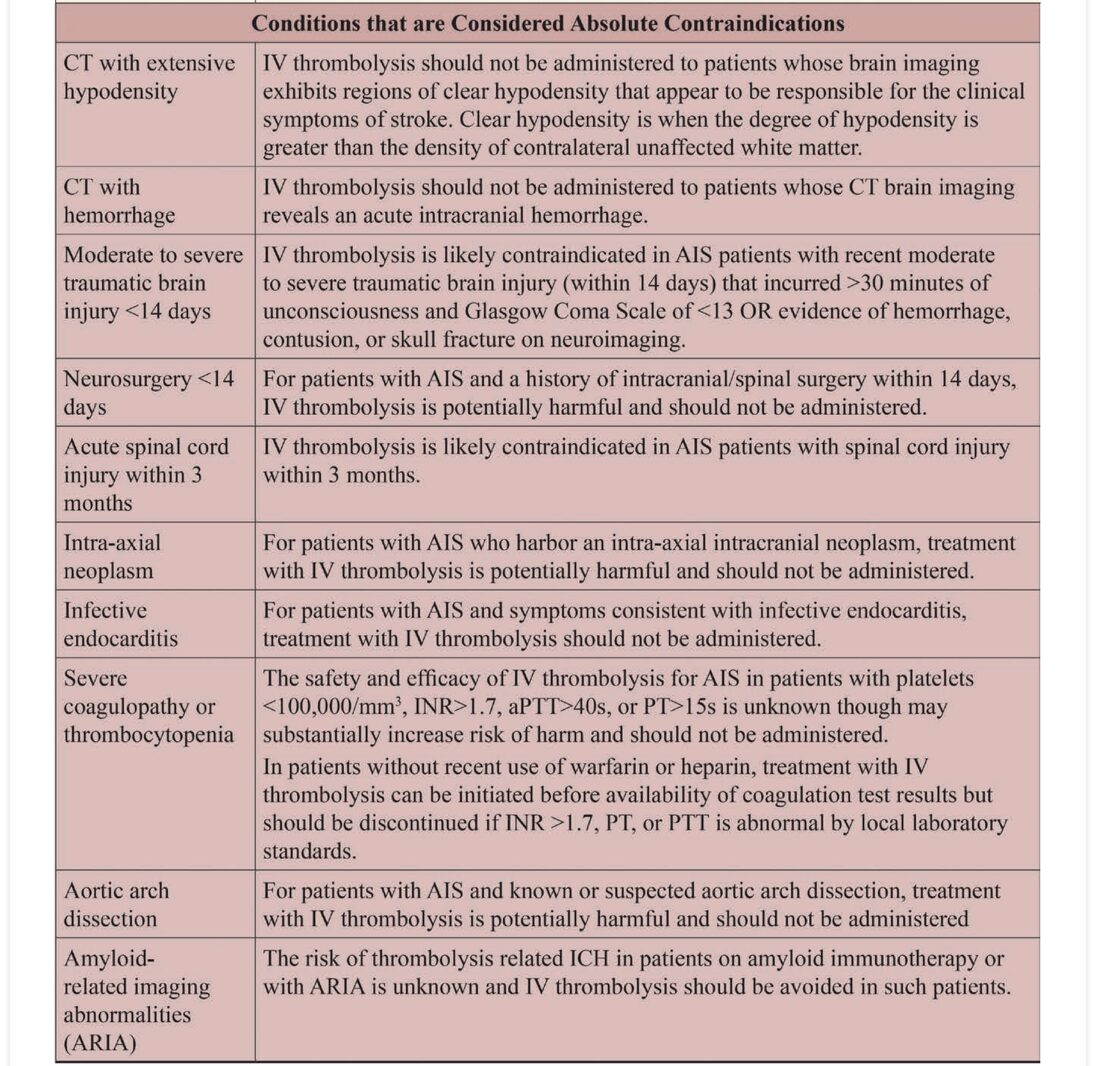
4.6.1 Thrombolysis Decision-Making



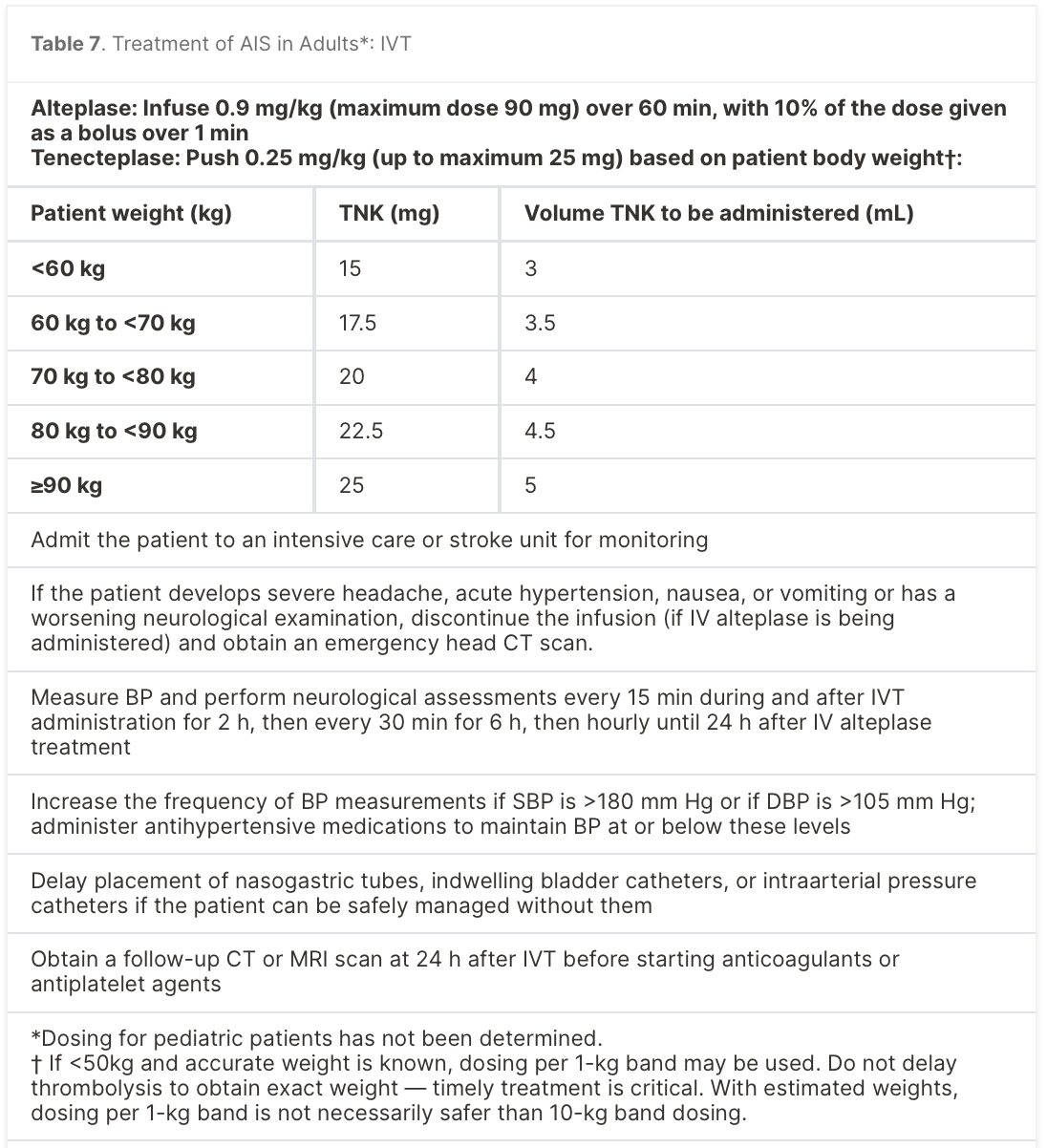
4.6.2 Choice of Thrombolytic Agent
4.6.3 Extended Time Windows for Intravenous Thrombolysis

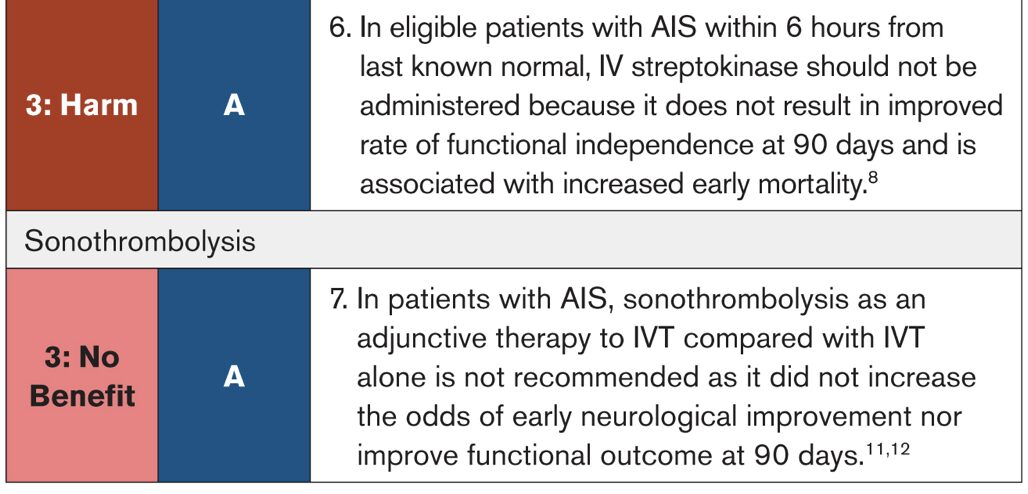
4.6.4 Other IV Fibrinolytics and Sonothrombolysis

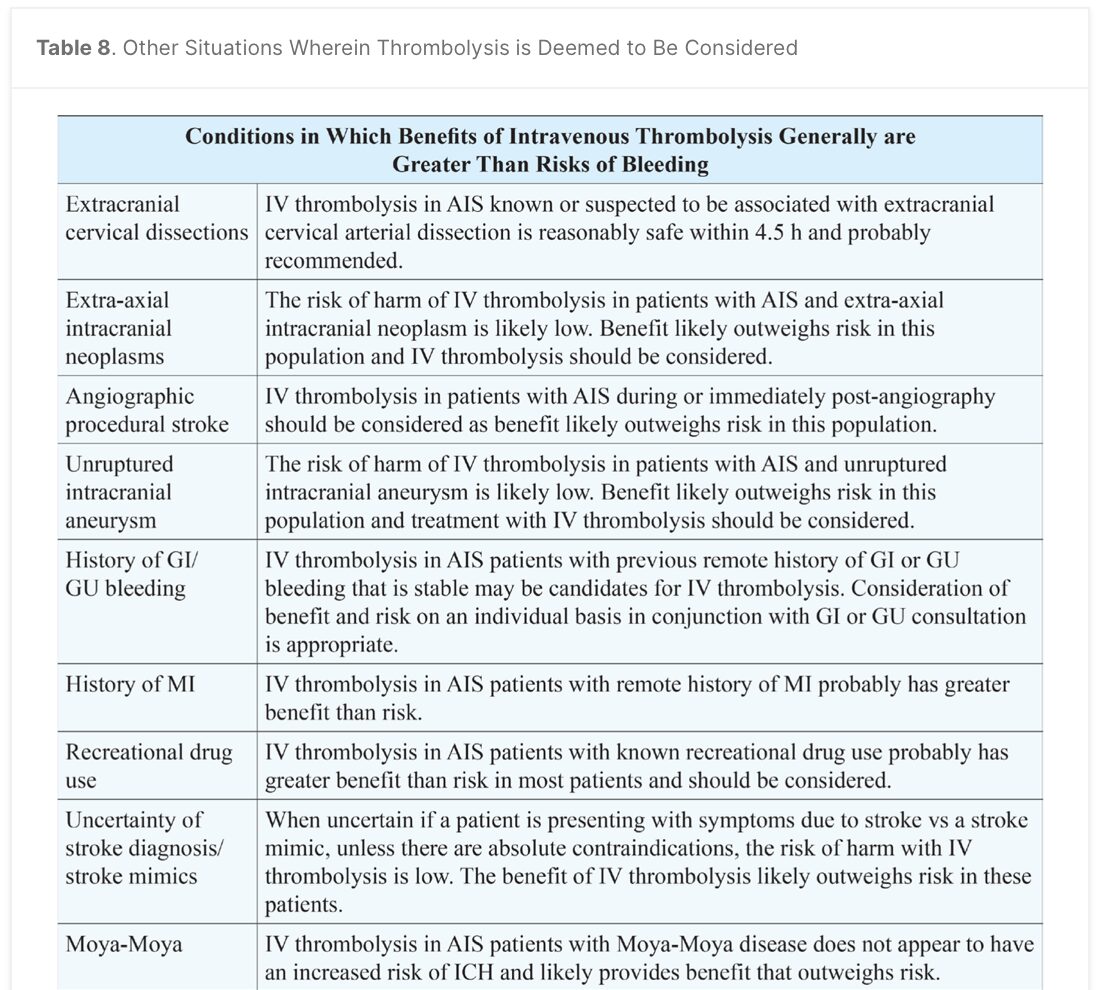
4.6.5 Other Specific Circumstances


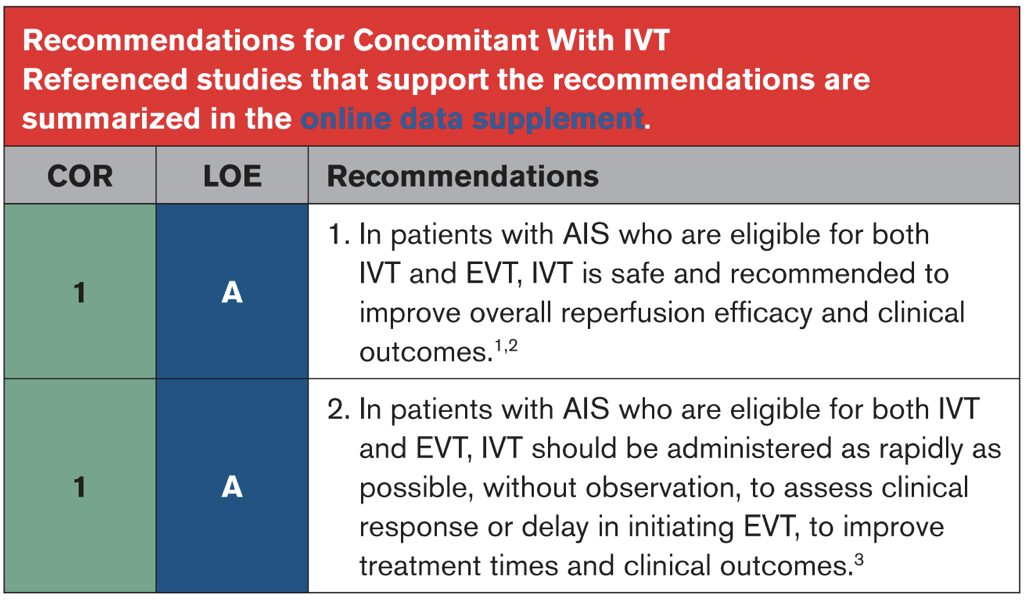
4.7.1 Endovascular thrombectomy concomitant with IVT
4.7.2 EVT for Adult Patients

4.7.3 Posterior Circulation Stroke

4.7.4 Endovascular Techniques


4.7.5 EVT in Pediatric Patients
4.8 Antiplatelet Treatment

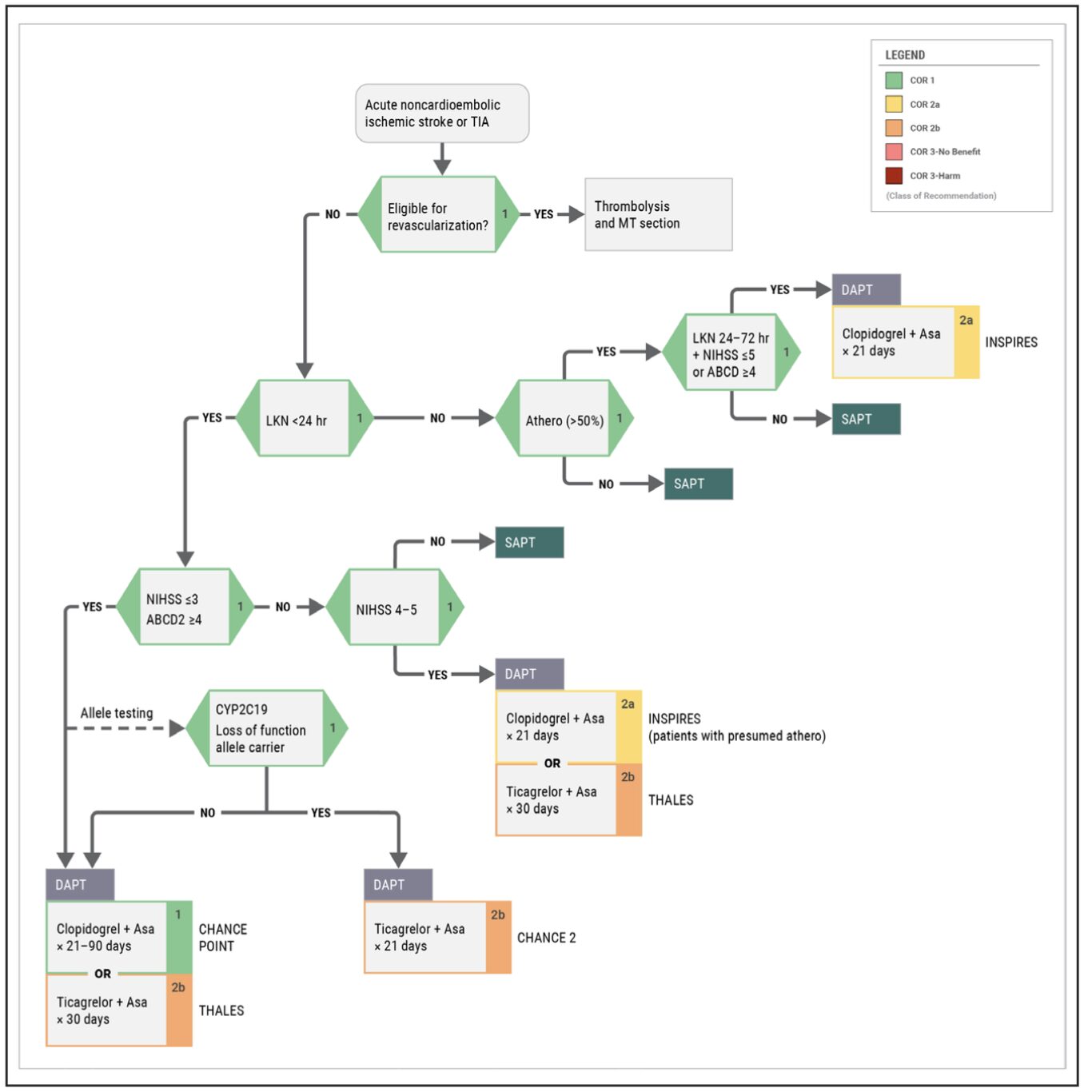
4.9 Anticoagulants
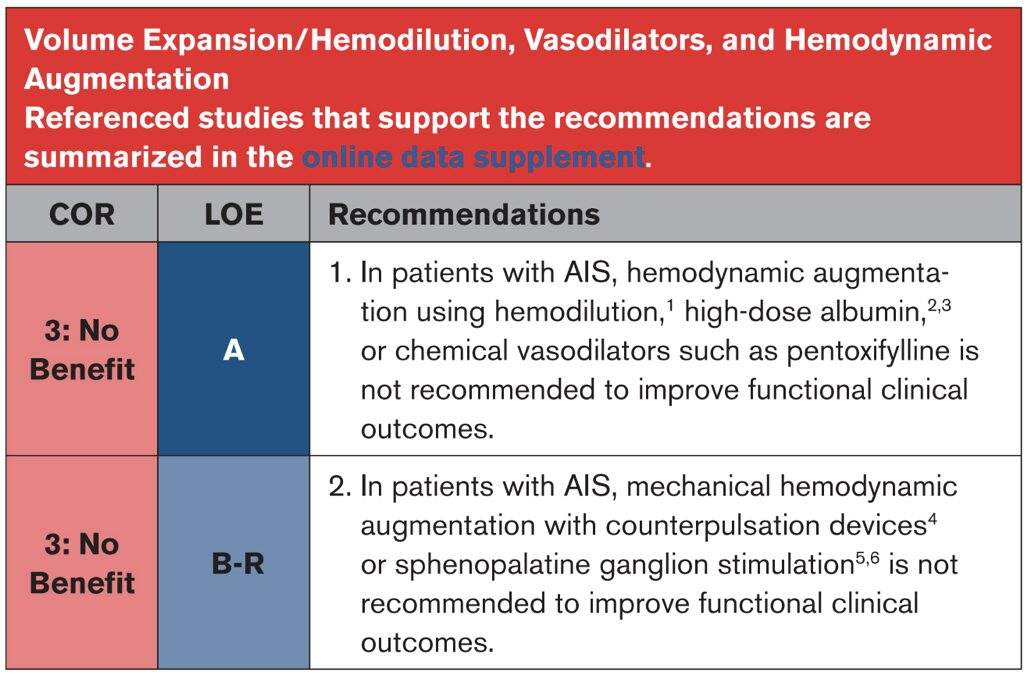
4.10 Volume Expansion/Hemodilution, Vasodilators, and Hemodynamic Augmentation
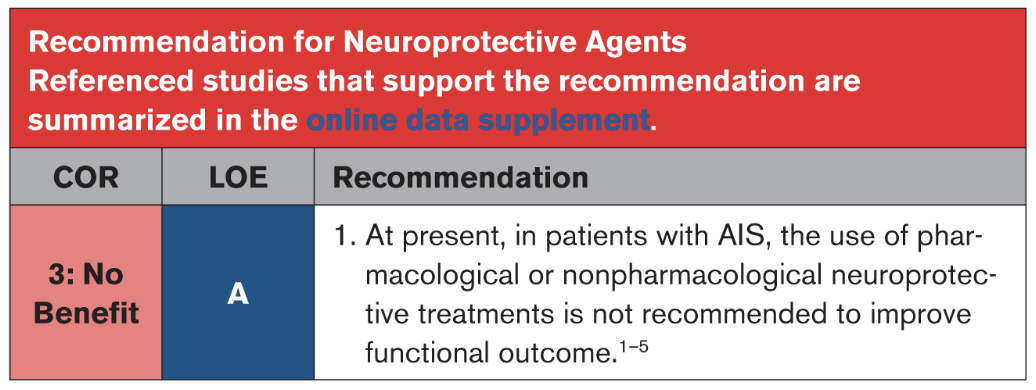
4.11 Neuroprotective Agents
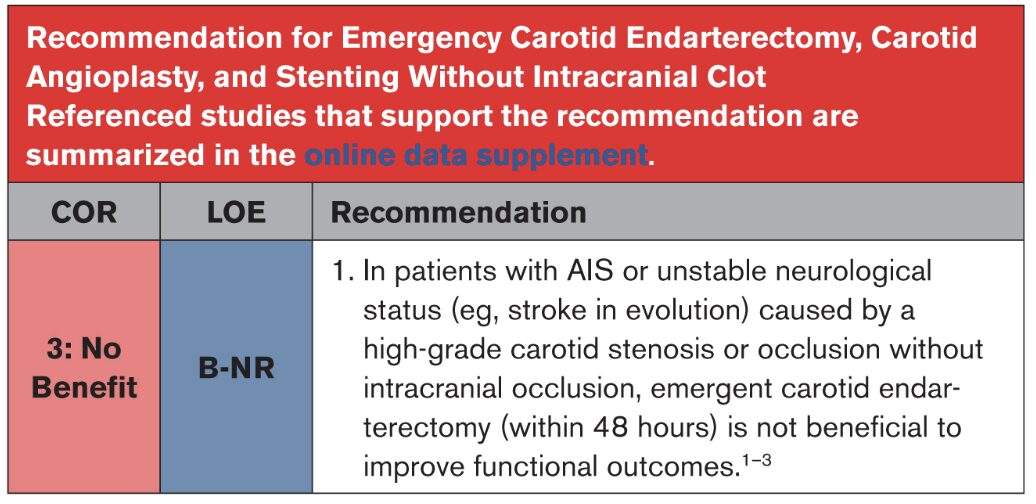
4.12 Emergency Carotid Endarterectomy, Carotid Angioplasty, and Stenting Without Intracranial Clot
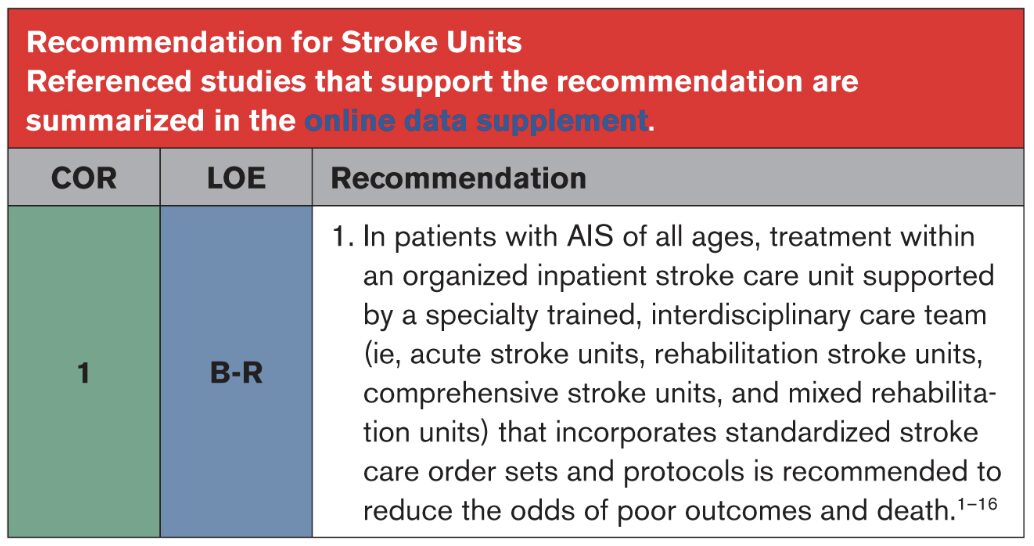
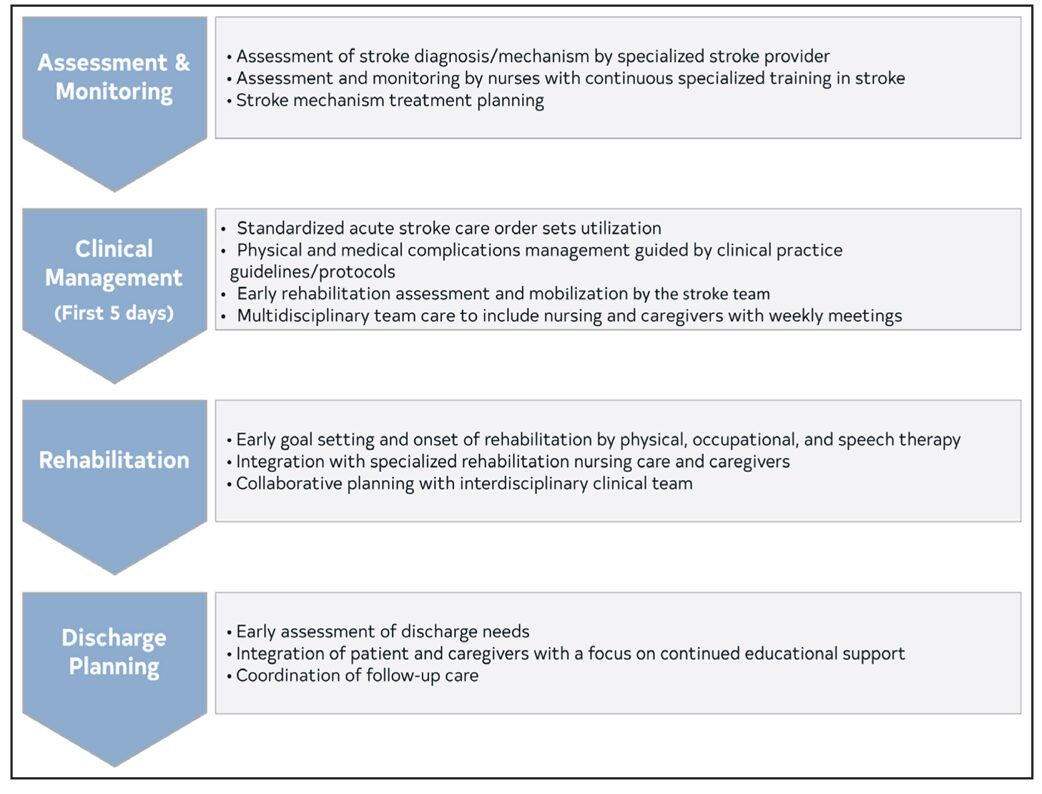
5.1 Stroke Units
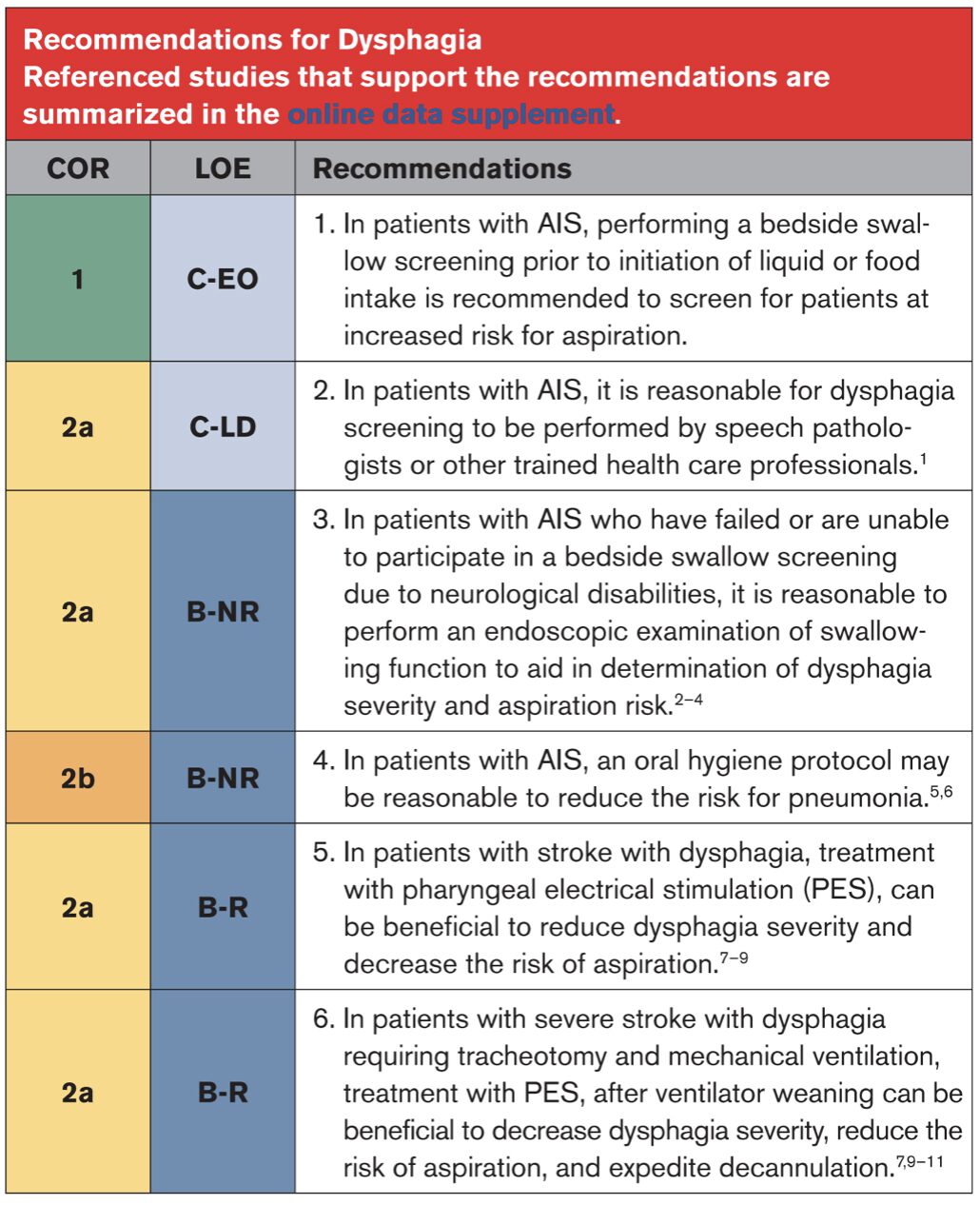
5.2 Dysphagia
5.3 Nutrition

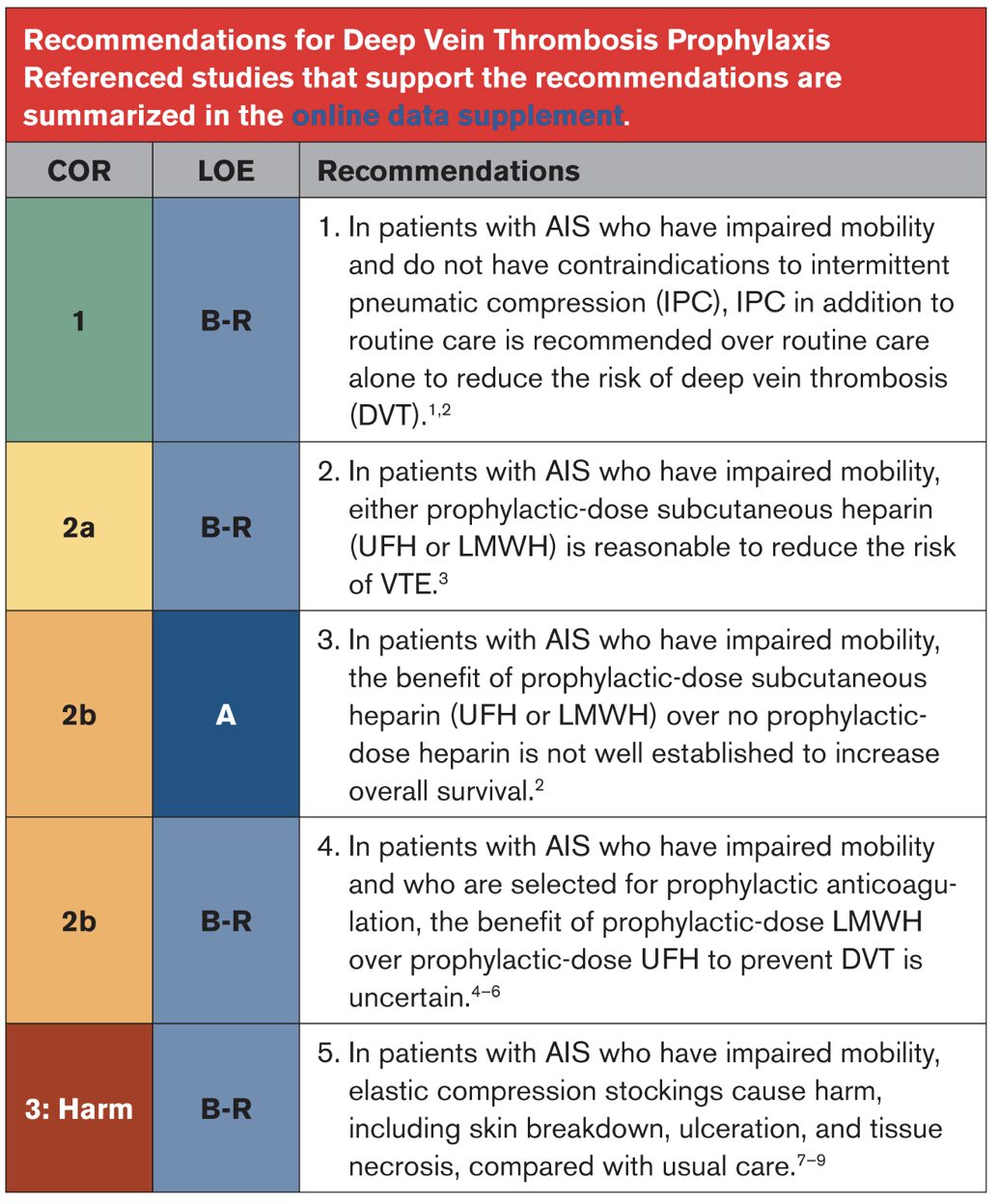
5.4 DVT Prophylaxis
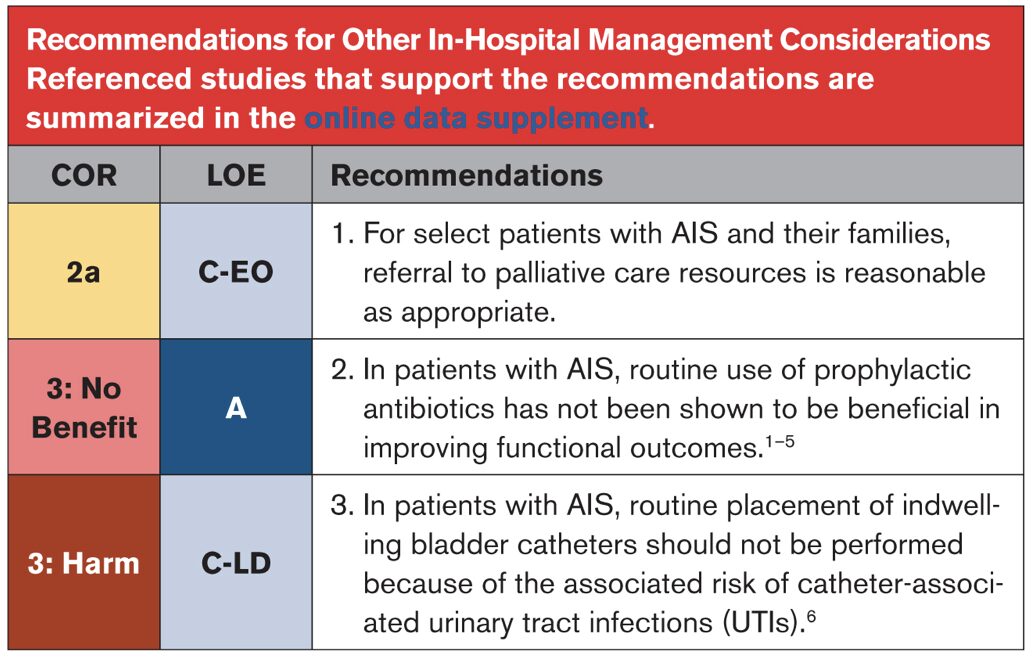
5.5 Depression
5.6 Other In-Hospital Management Considerations
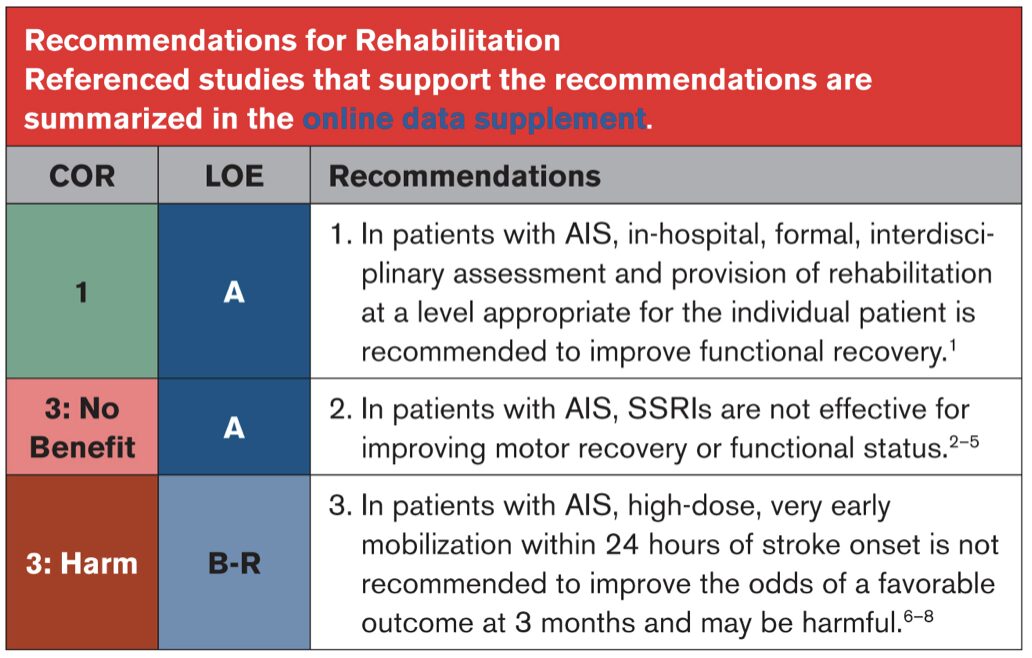
5.7 Rehabilitation
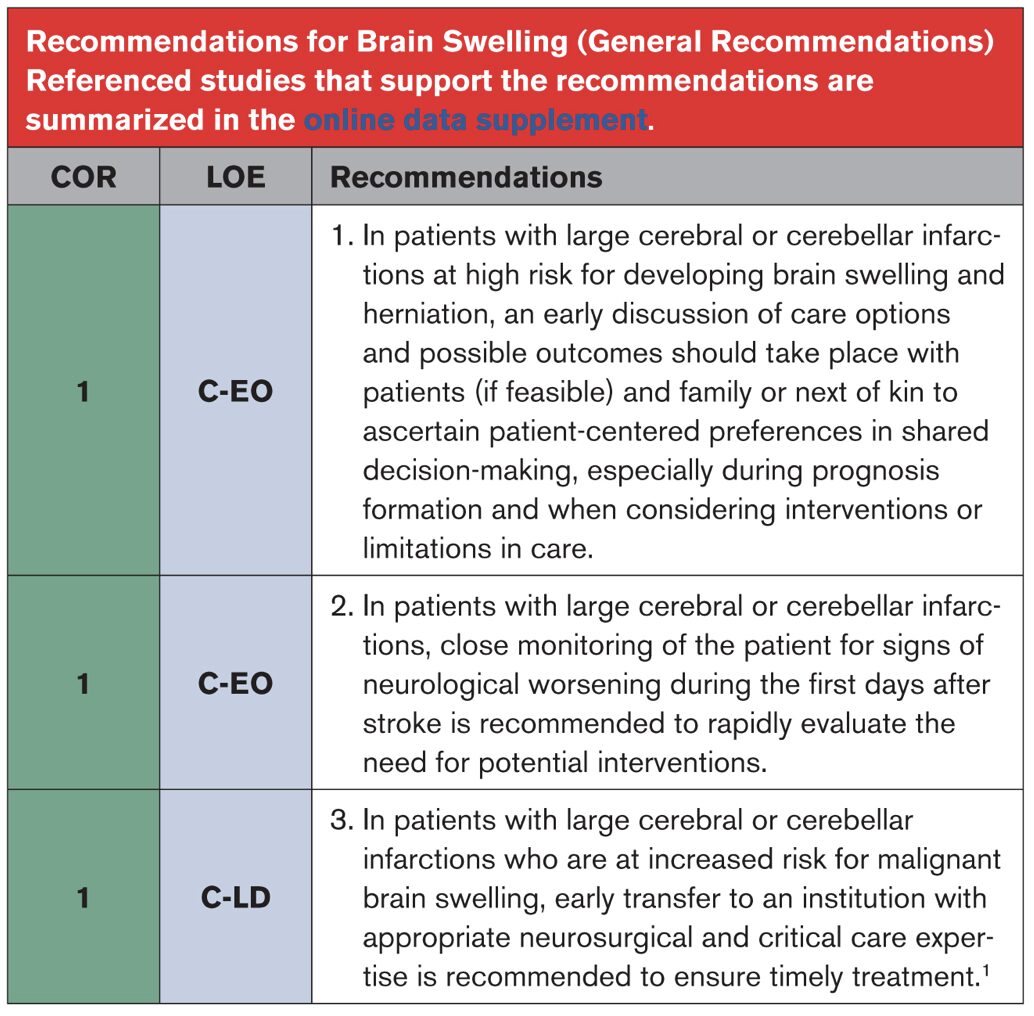
6.1 Brain Swelling (General Recommendations)
6.2 Brain Swelling (Medical Management)

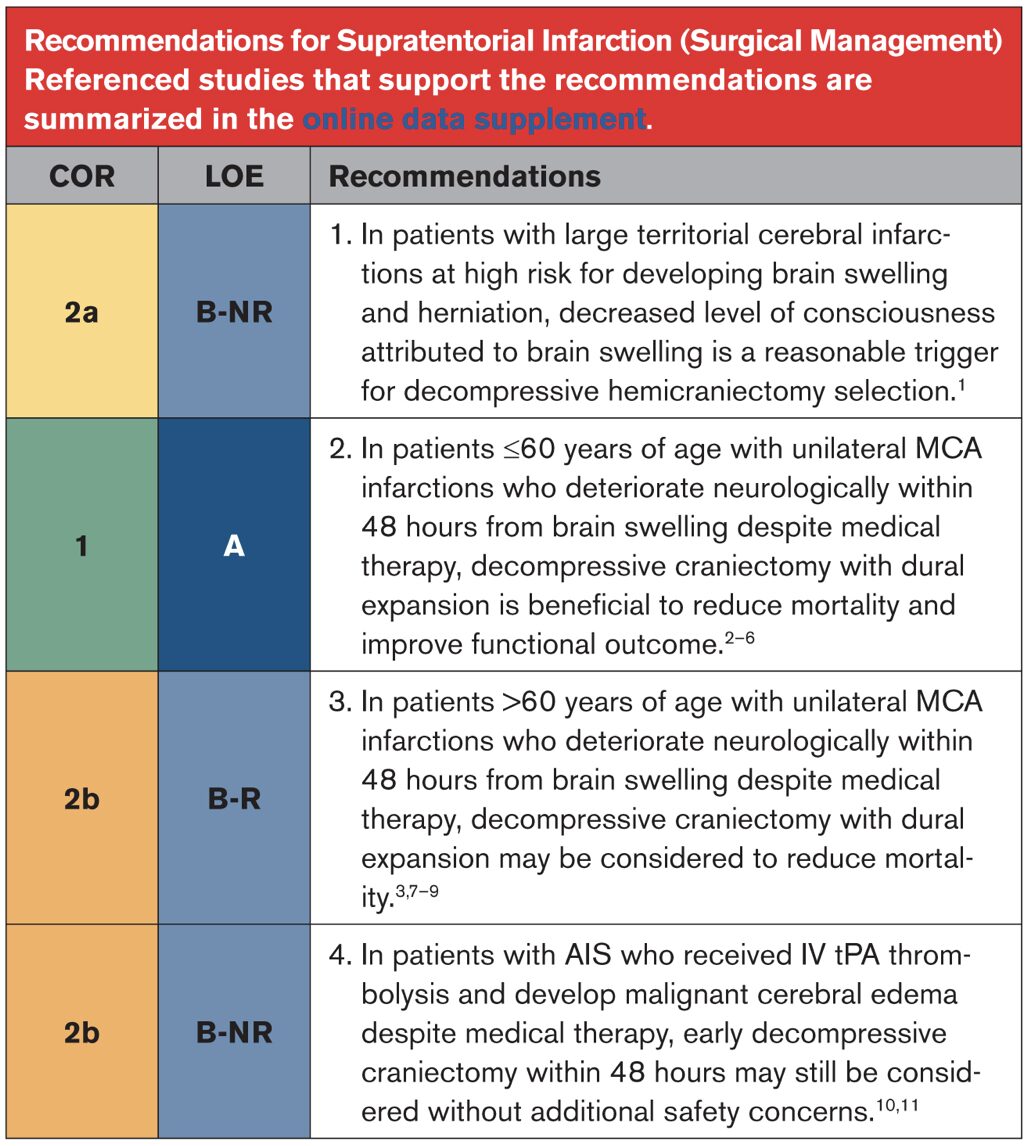
6.3 Supratentorial Infarction (Surgical Management)
6.4 Cerebellar Infarction (Surgical Management)

6.5 Seizures