Author: Erica Simon, DO, MHA (@E_M_Simon, EMS Fellow, SAUSHEC, USAF) // Edited by: Alex Koyfman, MD (@EMHighAK, EM Attending Physician, UTSW / Parkland Memorial Hospital) and Brit Long, MD (@long_brit, EM Attending Physician, SAUSHEC, USAF)
Welcome to EM@3AM, an emdocs series designed to foster your working knowledge by providing an expedited review of clinical basics. We’ll keep it short, while you keep that EM brain sharp.
A 29-year-old gravid female presents to the emergency department by ambulance following a motor vehicle collision. Per bystander reports, the young woman was struck on the passenger side of her compact vehicle at highway speeds. Following a prolonged extrication, the patient was intubated in the field secondary to altered mental status (GCS 6).
Initial ED vital signs: BP 95/79, HR 132, RR (Ventilator: 12), SpO2 98% on FiO2 100%, ETCO2 36 mmHg
Upon arrival, primary survey reveals an airway has been secured with an endotracheal tube. The patient is intubated and sedated. Bilateral breath sounds are present. Pulses are intact distally.
During the secondary survey you note blood oozing from the patient’s peripheral IV. Based upon fundal height, you estimate the patient as being in her third trimester of pregnancy.
What’s the next step in your evaluation and treatment?
Answer: Disseminated Intravascular Coagulation (DIC)1-5
- Definition: A systemic process in which the activation of the coagulation and fibrinolysis systems results in the simultaneous formation of thrombin and plasmin, with consumption of coagulation factors.1
- Etiologies: DIC may occur in the setting of sepsis (Gram negative infection most common1), burns, malignancy, obstetric complications, and trauma.
- Clinical Presentation: The balance between thrombin and plasmin formation in the individual patient clinically translates into a prothrombotic vs. hemorrhagic state.
- Evaluation:
- Assess ABCs and obtain vital signs.
- Perform a thorough history and physical examination.
- The diagnosis of DIC is clinical (appropriate clinical state/circumstance + laboratory findings suggestive of DIC):
- Characteristic laboratory studies in a hyperfibrinolytic state:
- Prolonged PT and aPTT
- Reduced Fibrinogen
- Elevated D-dimer
- Thombocytopenia
- Peripheral smear: microangiopathic hemolytic anemia (schistocytes and helmet cells)
- Note: An elevated level of fibrinogen degradation products is non-specific in the evalution of DIC: may variably represent plasmin-cleaved fibrinogen, soluble fibrin, or insoluble fibrin.1
- Characteristic laboratory studies in a pro-thrombotic state:
- Normal PT and aPTT
- Normal or Elevated Fibrinogen
- Elevated D-dimer
- Mild Thrombocytopenia
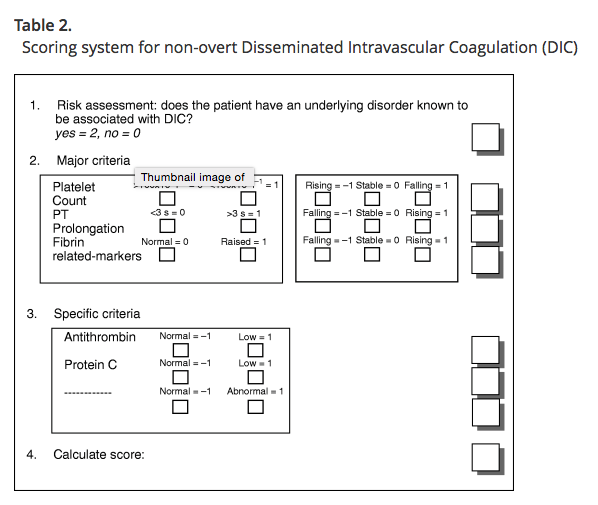
- In 2001, the International Society on Thrombosis and Haemostasis Subcommittee published scoring systems for the identification of overt (decompensated) and non-overt (subtle hemostatic dysfunction) DIC.2
- A validation study of the scoring systems, performed by Toh and Downey in 2005 (12 month study, one critical care unit, n = 450 patients; outcomes: overt DIC and 28-day mortality) demonstrated:3
- A 78% mortality for patients scoring ≥ 5 with the over DIC scoring system.
- Prognostic relevance of the non-overt DIC scoring system for individuals with a score ≥ 5 (i.e. – scoring system capable of identifying patients at risk of morbidity/mortality secondary to progression to overt DIC).
- A validation study of the scoring systems, performed by Toh and Downey in 2005 (12 month study, one critical care unit, n = 450 patients; outcomes: overt DIC and 28-day mortality) demonstrated:3
- Characteristic laboratory studies in a hyperfibrinolytic state:

http://onlinelibrary.wiley.com/doi/10.1111/j.1538-7836.2007.02313.x/full
http://onlinelibrary.wiley.com/doi/10.1111/j.1538-7836.2007.02313.x/full
- Treatment:4,5
- Identify and treat the underlying etiology.
- Mild and asymptomatic => monitor to resolution. Often self-limited.
- Severe => hemodynamic support as indicated, in addition to:
- Blood component therapy if active bleeding or high-risk for bleeding:
- Fresh-frozen plasma (10-15 ml/kg IV) => Goal is to normalize the INR.5
- Platelet transfusion (1-2 U/10 kg) if platelet count < 20,000/ mm3 or < 50,000/ mm3 in the presence of active bleeding.5
- Administer cryoprecipitate (1 U/5 kg) if fibrinogen <100 mg/dL => goal fibrinogen level: 100-150 mg/dL.5
- Consider recombinant factor VIIa, or antithrombin III for refractory bleeding.5
- Drug therapy:4,5
- Administer parenteral vitamin K (10 mg) if active bleeding.
- Consider heparin (300-500 U/hr) for DIC manifested by thrombosis or acrocyanosis in the absence of active bleeding.5
- Anti-fibrinolytics (tranexamic acid and ε-amioncaproic acid) are generally contraindicated, except in the setting of life-threatening bleeding and failure of blood component therapy. (Administration results in unopposed fibrin deposition which may result in thrombosis.)
- Blood component therapy if active bleeding or high-risk for bleeding:
- Pearls:5
- Consider the following in the differential diagnosis of DIC:
- Vitamin K deficiency (normal platelet count), hemolytic uremic syndrome (coagulation assays within normal limits), thrombotic thrombocytopenic purpura (low ADAMTS13 activity), HELLP syndrome (hemolysis, elevated liver function tests, and low platelets).
- Mortality rate in severe DIC exceeds 75%. Death commonly results from progression of the underlying disease, and associated complications (acute renal failure, intracerebral hematoma, shock, or cardiac tamponade).1
- Consider the following in the differential diagnosis of DIC:
References:
- Napolitano M, Schmaier A, Kessler C. Coagulation and Fibrinolysis. In Henry’s Clinical Diagnosis and Management by Laboratory Methods. 23rd ed. Philadelphia, Elsevier. 2017; 39:794-811.e3.
- International Society on Thrombosis and Haemostasis. ISTH SSC Reference Tools: Scoring System for Disseminated Intravascular Coagulation. Accessed 24 Aug 2017. Available from: http://onlinelibrary.wiley.com/doi/10.1111/j.1538-7836.2007.02313.x/full
- Toh C, and Downey C. Performance and prognostic importance of a new clinical and laboratory scoring system for identifying non-overt disseminated intravascular coagulation. Blood Coagul Fibrinolysis. 2005; 16(1):69-74.
- Schafer, A. Hemorrhagic Disorders: Disseminated Intravascular Coagulation, Liver Failure, and Vitamin K Deficiency. In Goldman-Cecil Medicine. 25th ed. Philadelphia, Elsevier. 2016; 175:1181-1184.e2.
- Gultawatvichai P, and Rathore B. Disseminated Intravascular Coagulation. In Ferri’s Clinical Advisor. Philadelphia, Elsevier. 2018; 398-399.e2.
For Additional Reading:







2 thoughts on “EM@3AM – Disseminated Intravascular Coagulation”
Pingback: Post-Partum Hemorrhage - R.E.B.E.L. EM - Emergency Medicine Blog
Pingback: REBEL Core Cast 44.0 - Postpartum Hemorrhage - REBEL EM - Emergency Medicine Blog