Today on the emDOCs cast with Brit Long, MD (@long_brit), we cover sympathetic crashing acute pulmonary edema (SCAPE).
Episode 123: Sympathetic Crashing Acute Pulmonary Edema
What is this?
- SCAPE is a subset of acute heart failure syndrome (AHFS) associated with rapid onset of respiratory distress, pulmonary edema, and hypertension.
What is different with SCAPE compared to other types of AHFS?
- AHFS is common and associated with significant morbidity and mortality.
- Several different subtypes of AHFS.
- Subacute pulmonary edema to AHF: worsening symptoms over days, hypervolemic with systemic congestion (peripheral edema, ascites, anasarca).
- SCAPE differs in several significant ways: rapid onset (hours), respiratory distress, severe HTN, may or may not be systemically volume overload.
- SCAPE defining features: 1) rapid onset of respiratory distress (<4-6 hours); 2) pulmonary edema with severe dyspnea; 3) abdominal vital signs with SBP > 160 and/or > 120, hypoxic, tachypneic, tachycardic; 4) critically ill, evidence of pulmonary edema.
- In SCAPE, uncontrolled sympathetic function and increased afterload leads to HTN and fluid redistribution from the periphery into the pulmonary system.
- Causes: ACS, arrhythmia, valvular dysfunction, infection, nonadherence to meds, myocarditis, volume overload.
What are the key tests?
- Tests: ECG, labs, chest imaging. Goal is to assess for end organ injury and the underlying trigger while resuscitating.
- Labs: CBC, electrolytes, renal/liver function, troponin. Elevations in Cr, LFTs, troponin associated with worse outcomes.
- Troponin elevations common in SCAPE, but typically associated with demand ischemia, not OMI.
- BNP may be used if uncertain of AHFS diagnosis, but typically not helpful.
What about imaging?
- Chest x-ray: cardiomegaly, bilateral interstitial markings, perihilar pulmonary edema, pleural effusions.
- Sensitivity 56-75%, specificity 86-96%; up to 20-25% have normal x-ray (Martindale, Sartini, Collins, Maw).
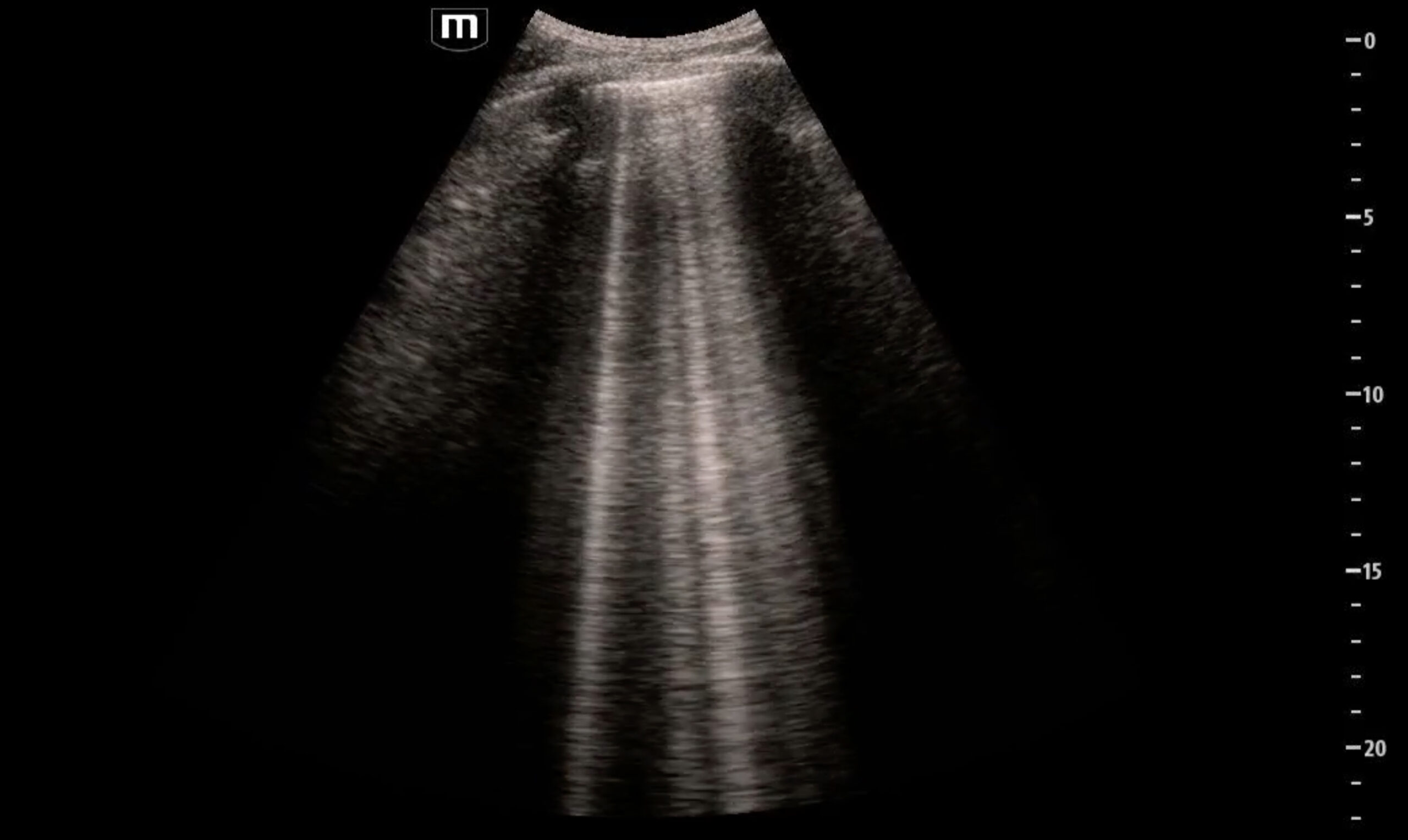
- POCUS: Rapid, reliable for evaluation of suspected heart failure with pulmonary edema.
- Endorsed by the American College of Emergency Physicians, Society for Academic Emergency Medicine/Heart Failure Society of America’s Acute Heart Failure Working Group, and the European Society of Cardiology (ACEP, Collins 2015, Ponikowski).
- Multiple meta-analyses suggest sensitivity 75-90% and specificity 80-93%; more reliable than chest x-ray and can differentiate between other conditions with dyspnea (COPD) (Martindale, Maw, McGivery, Staub, Lian).
- Evaluate for ≥ 3 B lines in two bilateral lung zones. If present => diagnostic for pulmonary edema.
- Echocardiography can assist, but not mandatory for diagnosis of SCAPE.
- E-point septal separation (EPSS) measures distance between anterior mitral valve leaflet and ventricular septum; > 7 mm suggests EF < 50% (Silverstein, Anderson).
- IVC diameter and respiratory change in diameter can assess fluid tolerance.
Treatment:
- Goals: address patient’s respiratory status and HTN/high afterload.
- Primary treatments: NIPPV and high-dose nitroglycerin.
NIPPV:
- Start immediately if no contraindications present (respiratory failure and need for emergent intubation, recent facial surgery/trauma, recurrent emesis).
- Provides respiratory support: increases the intrathoracic pressure, decreases preload, prevents alveolar collapse at end-expiration, reduces LV afterload.
- Meta-analyses demonstrate reduced need for intubation, improved survival, improved respiratory indices (e.g., respiratory rate, oxygenation, hypercapnia), and decreased work of breathing (Masip, Collins 2006, Weng, Berbenetz).
- 2019 Cochrane review: 24 studies, 2664 patients with acute cardiogenic pulmonary edema; NNT 17 to prevent death and NNT 13 to prevent intubation (Berbenetz).
- May use BPAP or CPAP; neither superior to the other.
- BPAP: start at 10-12 cm H20/5-6 cm H20 and then increase.
- CPAP: start at 5-8 cm H20 and rapidly titrate.
- Increasing BPAP/CPAP pressures will rapidly decrease preload and afterload.
- Caution with pressures > 20 cm H20 (may result in gastric insufflation).
- If having issues with the mask, hold the mask gently to the patient’s face and start at lower pressures. May use haloperidol, droperidol, ketamine, or fentanyl for comfort.
- Must closely monitor; if not improving or decompensating, intubate.
Nitroglycerin:
- Nitroglycerin is the first line medication to reduce blood pressure.
- Standard doses of nitroglycerin (0.4 mg SL, 50-80 mcg per minute over 5 minutes) reduce preload.
- SCAPE is associated with vasoconstriction and high afterload. At higher doses nitroglycerin vasodilates and reduces afterload.
- Literature suggests high doses in SCAPE are safe and efficacious. May include 500-2000 micrograms over 2 minutes or an infusion of 400-800 micrograms per minute for 2-2.5 minutes (Wang, Mathew, Siddiqua, Houseman, Stemple, Paone, Levy, Wilson).
- Feasibility study evaluated 2 mg boluses every 3 minutes compared to 30 mcg per minute. Lower intubation, need for BPAP and ICU admission in bolus group (Levy 2007).
- RCT evaluating high-dose (600-1000 microgram bolus followed by infusion at 100 micrograms/minute) versus low-dose nitroglycerin (infusion of 20-40 micrograms per minute with no bolus) found greater symptom resolution at 6 hours (65.4% versus 11.5%) and 12 hours (88.5% versus 19.5%) with high-dose bolus. Shorter hospital LOS, lower intubation, lower MACE in high-dose group (Siddiqua).
- Feared risks of high-dose bolus primarily include hypotension. Rare based on current data. 2021 observational study with 25 patients utilized a mean bolus dose of 872 micrograms, with a mean cumulative dose of 35 mg (Mathew).
- ACEP clinical policy on AHFS: level C recommendation – high-dose nitroglycerin is safe and effective in patients with HF and elevated blood pressure (ACEP).
- Personally, I administer a bolus of 500-600 mcg for those with a SBP 160-200 and 1000 mcg for those with SBP > 200, and then start infusion at 100 mcg/minute with close monitoring.
- Most patients will improve with 1 or 2 boluses; once BP and respiratory improves (target BP < 140-160), infusion rate can be reduced or discontinued.
- If no improvement in 5 minutes, repeat bolus and maximize NIPPV support; may repeat the bolus again.
- If no IV access, administer 3-5 400 mcg tablets at one time (provide a squirt of saline or water to assist with dissolution).
- Contraindication: recent phosphodiesterase type-5 inhibitor use.
- Aortic stenosis is not an absolute contraindication to nitroglycerin with SCAPE, but use lower doses with more gradual titration (Claveau).
What are other medications if patients don’t improve with nitroglycerin?
- Uncommon with maximal NIPPV and high-dose nitroglycerin, but may use another vasodilator (clevidipine or nicardipine) or ACE inhibitor if SBP remains > 160 mm Hg (Raggi, Peacock 2010/2014, Ayaz, Annane).
- Clevidipine or nicardipine are also recommended if there’s a contraindication to nitroglycerin.
- PRONTO RCT compared clevidipine with standard IV antiHTN therapy in HTN AHFS and found clevidipine had greater likelihood of reaching BP target and faster time to BP target with reduction in dyspnea (Peacock 2014).
- ACE inhibitors reduce arterial resistance and increase venous capacitance by blocking the renin-angiotensin system (RAS) and angiotensin II synthesis (Ayaz, Annane).
- Most common: enalaprilat 0.625-1.25 mg IV repeated every 15 minutes up to a maximum dose of 5 mg or oral captopril 12.5-25 mg.
- BP reduction typically within 30 minutes with IV enalaprilat.
- Avoid in renal dysfunction.
What about diuretics?
- Diuretics are key in AHFS with volume overload.
- Class 1 recommendation from American College of Cardiology /American Heart Association guidelines (Yancy).
- ACEP level C recommendation that while there is no specific timing for diuretic therapy, physicians can consider earlier administration of diuretics in ED patients with HF (ACEP).
- Should be confident in diagnosis of AHFS with volume overload, as diuretics may cause harm.
- In ED population, diuretics have not demonstrated clear benefit in mortality.
- Literature suggests IV furosemide may decrease preload and pulmonary capillary wedge pressures while increasing venous capacitance (Dikshit, Fanciosa, Pickkers). Randomized data suggests no difference in reported dyspnea with furosemide versus placebo in pulmonary edema with severe HTN (Holzer).
- Key: SCAPE is associated with excessive sympathetic function leading to increased afterload rather than volume overload.
- Most patients with SCAPE are hypovolemic or euvolemic due to fluid maldistribution from the splanchnic circulation to the pulmonary system (thus NIPPV and nitro).
- If systemic volume overload present (weight gain, peripheral edema, anasarca), administer furosemide 20-40 mg IV, torsemide 10-20 mg IV, or bumetanide 1 mg IV.
What medications should we avoid?
- Beta blockers may reduce EF and worsen pulmonary edema in acute decompensated HF (Heidenreich).
- Current literature suggests morphine may worsen outcomes in AHFS.
- 2022 prospective randomized trial comparing morphine (up to 8 mg) and midazolam (up to 3 mg) stopped early for harm, with significantly fewer serious adverse events in the midazolam group (18.2% vs. 42.9%; RR 0.42, 95% CI 0.22-0.80) (Dominguez).
- 2022 meta-analysis (6 observational studies) found higher in-hospital mortality with morphine (OR 2.39, 95% CI 1.13-5.08), increased need for invasive ventilation (OR 6.14, 95% CI 5.84-6.46), increased need for non-invasive ventilation (OR 1.85, 95% CI 1.45-2.36) and increased need for vasopressors/inotropes (OR 2.93, 95% CI 2.20-3.89) (Witharana).
- Avoid nephrotoxic agents.
Summary:
- SCAPE is sudden, severe pulmonary edema, hypertension, and respiratory distress with hypoxemia due to excess afterload and fluid maldistribution into the pulmonary system.
- Get labs, ECG, and use US to look for ≥ 3 B lines in bilateral lung fields (diagnostic of pulmonary edema in the appropriate setting).
- Address respiratory status and HTN/afterload. Start with NIPPV and high-dose nitroglycerin. Both are effective in improving respiratory and hemodynamic status, but closely monitor. Intubate if respiratory status not improving.
- High-dose nitroglycerin is safe and effective; reduces afterload and preload. May use boluses 500-1000 mcg plus infusion.
- For refractory HTN, consider nicardipine or clevidipine, or an ACE inhibitor.
- Diuretics can be used for volume overload; otherwise avoid.
References/Further Reading:
- Long B, Brady WJ, Gottlieb M. Emergency medicine updates: Sympathetic crashing acute pulmonary edema. Am J Emerg Med. 2025 Jan 5;90:35-40.
- Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 May 3;145(18):e895-e1032. doi: 10.1161/CIR.0000000000001063. Epub 2022 Apr 1. Erratum in: Circulation. 2022 May 3;145(18):e1033. doi: 10.1161/CIR.0000000000001073. Erratum in: Circulation. 2022 Sep 27;146(13):e185. doi: 10.1161/CIR.0000000000001097. Erratum in: Circulation. 2023 Apr 4;147(14):e674. doi: 10.1161/CIR.0000000000001142. PMID: 35363499.
- American College of Emergency Physicians Clinical Policies Subcommittee (Writing Committee) on Acute Heart Failure Syndromes. Clinical Policy: Critical Issues in the Evaluation and Management of Adult Patients Presenting to the Emergency Department With Acute Heart Failure Syndromes: Approved by ACEP Board of Directors, June 23, 2022. Ann Emerg Med. 2022 Oct;80(4):e31-e59. doi: 10.1016/j.annemergmed.2022.05.027. Erratum in: Ann Emerg Med. 2023 Mar;81(3):383. doi: 10.1016/j.annemergmed.2023.01.040. PMID: 36153055.
- Collins S, Storrow AB, Albert NM, et al. Early management of patients with acute heart failure: state of the art and future directions. A consensus document from the society for academic emergency medicine/heart failure society of America acute heart failure working group. J Card Fail. 2015;21:27-43.
- Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013; 62(16):e147–239.
- Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18:891-975.
- Long B, Koyfman A, Gottlieb M. Diagnosis of Acute Heart Failure in the Emergency Department: An Evidence-Based Review. West J Emerg Med. 2019 Oct 24;20(6):875-884.
- Long B, Koyfman A, Gottlieb M. Management of Heart Failure in the Emergency Department Setting: An Evidence-Based Review of the Literature. J Emerg Med. 2018 Nov;55(5):635-646.
- Long B, Koyfman A, Chin EJ. Misconceptions in acute heart failure diagnosis and Management in the Emergency Department. Am J Emerg Med. 2018 Sep;36(9):1666-1673.
- Martindale JL, Wakai A, Collins SP, et al. Diagnosing Acute Heart Failure in the Emergency Department: A Systematic Review and Meta-analysis. Acad Emerg Med. 2016;23:223-242.
- Sartini S, Frizzi J, Borselli M, et al. Which method is best for an early accurate diagnosis of acute heart failure? Comparison between lung ultrasound, chest X-ray and NT pro-BNP performance: a prospective study. Intern Emerg Med. 2017;12:861–869.
- Collins SP, Lindsell CJ, Storrow AB, Abraham WT; ADHERE Scientific Advisory Committee, Investigators and Study Group. Prevalence of negative chest radiography results in the emergency department patient with decompensated heart failure. Ann Emerg Med. 2006;47:13-8.
- Maw AM, Hassanin A, Ho PM, et al. Diagnostic Accuracy of Point-of-Care Lung Ultrasonography and Chest Radiography in Adults With Symptoms Suggestive of Acute Decompensated Heart Failure: A Systematic Review and Meta-analysis. JAMA Netw Open. 2019 Mar 1;2(3):e190703.
- Maw AM, Hassanin A, Ho PM, et al. Diagnostic Accuracy of Point-of-Care Lung Ultrasonography and Chest Radiography in Adults With Symptoms Suggestive of Acute Decompensated Heart Failure: A Systematic Review and Meta-analysis. JAMA Netw Open. 2019 Mar 1;2(3):e190703.
- McGivery K, Atkinson P, Lewis D, et al. Emergency department ultrasound for the detection of B-lines in the early diagnosis of acute decompensated heart failure: a systematic review and meta-analysis. CJEM. 2018;20:343-352.
- Staub LJ, Mazzali Biscaro RR, Kaszubowski E, et al. Lung ultrasound for the emergency diagnosis of pneumonia, acute heart failure, and exacerbations of chronic obstructive pulmonary disease/asthma in adults: a systematic review and meta-analysis. J Emerg Med. 2019;56:53-69.
- Lian R, Zhang GC, Yan ST, et al. Role of ultrasound lung comets in the diagnosis of acute heart failure in emergency department: a systematic review and meta-analysis. Biomed Environ Sci. 2018;31:596-607.
- Silverstein JR, Laffely NH, Rifkin RD. Quantitative estimation of left ventricular ejection fraction from mitral valve E-point to septal separation and comparison to magnetic resonance imaging. Am J Cardiol. 2006;97(1):137-40.
- Anderson KL, Jenq KY, Fields JM, et al. Diagnosing heart failure among acutely dyspneic patients with cardiac, inferior vena cava, and lung ultrasonography. Am J Emerg Med. 2013;31(8):1208-1214.
- Masip J, Betbesé AJ, Páez J, et al. Non-invasive pressure support ventilation versus conventional oxygen therapy in acute cardiogenic pulmonary oedema: a randomised trial. Lancet. 2000 Dec 23-30;356(9248):2126-32.
- Collins SP, Mielniczuk LM, Whittingham HA, et al. The use of noninvasive ventilation in emergency department patients with acute cardiogenic pulmonary edema: a systematic review. Ann Emerg Med. 2006 Sep;48(3):260-9, 269.e1-4.
- Weng CL, Zhao YT, Liu QH, et al. Meta-analysis: Noninvasive ventilation in acute cardiogenic pulmonary edema. Ann Intern Med. 2010 May 4;152(9):590-600. doi: 10.7326/0003-4819-152-9-201005040-00009. Erratum in: Ann Intern Med. 2010 Aug 17;153(4):280.
- Berbenetz N, Wang Y, Brown J, et al. Non-invasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary oedema. Cochrane Database Syst Rev. 2019 Apr 5;4(4):CD005351.
- Wang K, Samai K. Role of high-dose intravenous nitrates in hypertensive acute heart failure. Am J Emerg Med. 2020 Jan;38(1):132-137.
- Mathew R, Kumar A, Sahu A, et al. High-Dose Nitroglycerin Bolus for Sympathetic Crashing Acute Pulmonary Edema: A Prospective Observational Pilot Study. J Emerg Med. 2021 Sep;61(3):271-277.
- Siddiqua N, Mathew R, Sahu AK, et al. High-dose versus low-dose intravenous nitroglycerine for sympathetic crashing acute pulmonary edema: a randomised controlled trial. Emerg Med J. 2024 Jan 22;41(2):96-102.
- Houseman BS, Martinelli AN, Oliver WD, et al. High-dose nitroglycerin infusion description of safety and efficacy in sympathetic crashing acute pulmonary edema: The HI-DOSE SCAPE study. Am J Emerg Med. 2023 Jan;63:74-78.
- Stemple K, DeWitt KM, Porter BA, et al. High-dose nitroglycerin infusion for the management of sympathetic crashing acute pulmonary edema (SCAPE): A case series. Am J Emerg Med. 2021 Jun;44:262-266.
- Paone S, Clarkson L, Sin B, Punnapuzha S. Recognition of Sympathetic Crashing Acute Pulmonary Edema (SCAPE) and use of high-dose nitroglycerin infusion. Am J Emerg Med. 2018 Aug;36(8):1526.e5-1526.e7.
- Levy P, Compton S, Welch R, et al. Treatment of severe decompensated heart failure with high-dose intravenous nitroglycerin: a feasibility and outcome analysis. Ann Emerg Med 2007;50:144–52.
- Wilson SS, Kwiatkowski GM, Millis SR, et al. Use of nitroglycerin by bolus prevents intensive care unit admission in patients with acute hypertensive heart failure. Am J Emerg Med. 2017;35(1):126-131.
- Claveau D, Piha-Gossack A, Friedland SN, et al. Complications Associated With Nitrate Use in Patients Presenting With Acute Pulmonary Edema and Concomitant Moderate or Severe Aortic Stenosis. Ann Emerg Med. 2015 Oct;66(4):355-362.e1.
- Raggi JR, O’Connell TW, Singer DJ. Nicardipine: When high dose nitrates fail in treating heart failure. Am J Emerg Med. 2021 Jul;45:681.e3-681.e5.
- Peacock F 4th, Varon J, Ebrahimi R, et al. Clevidipine for severe hypertension in acute heart failure: a VELOCITY trial analysis. Congest Heart Fail. 2010 Mar-Apr;16(2):55-9.
- Peacock WF, Chandra A, Char D, et al. Clevidipine in acute heart failure: Results of the A Study of Blood Pressure Control in Acute Heart Failure-A Pilot Study (PRONTO). Am Heart J. 2014 Apr;167(4):529-36.
- Ayaz SI, Sharkey CM, Kwiatkowski GM, et al. Intravenous enalaprilat for treatment of acute hypertensive heart failure in the emergency department. Int J Emerg Med 2016;9(1):28.
- Annane D, Bellissant E, Pussard E, et al. Placebo controlled, randomized, double-blind study of intravenous enalaprilat efficacy and safety in acute cardiogenic pulmonary edema. Circulation 1996; 94(6):1316–24.
- Dikshit K, Vyden JK, Forrester JS, et al. Renal and extrarenal hemodynamic effects of furosemide in congestive heart failure after acute myocardial infarction. N Engl J Med 1973; 288(21):1087–90.
- Franciosa JA, Silverstein SR. Hemodynamic effects of nitroprusside and furosemide in left ventricular failure. Clin Pharmacol Ther 1982;32(1):62–9.
- Pickkers P, Dormans TP, Russel FG, et al. Direct vascular effects of furosemide in humans. Circulation 1997;96(6):1847–52.
- Holzer-Richling N, Holzer M, Herkner H, et al. Randomized placebo controlled trial of furosemide on subjective perception of dyspnoea in patients with pulmonary oedema because of hypertensive crisis. Eur J Clin Invest 2011;41(6):627–34.
- Domínguez-Rodríguez A, Suero-Mendez C, Burillo-Putze G, et al; MIMO (MIdazolam versus MOrphine) Trial Investigators. Midazolam versus morphine in acute cardiogenic pulmonary oedema: results of a multicentre, open-label, randomized controlled trial. Eur J Heart Fail. 2022 Oct;24(10):1953-1962.
- Witharana TN, Baral R, Vassiliou VS. Impact of morphine use in acute cardiogenic pulmonary oedema on mortality outcomes: a systematic review and meta-analysis. Ther Adv Cardiovasc Dis. 2022 Jan-Dec;16:17539447221087587.






