Authors: Zachary Boivin MD (Ultrasound Faculty Yale Department of Emergency Medicine), Jia Jian Li MD (Ultrasound Faculty St John’s Riverside Hospital Department of Emergency Medicine) // Reviewed by: Stephen Alerhand MD (Ultrasound Faculty Rutgers University Department of Emergency Medicine)
Case
A 27 year-old G2P1 female with no prior medical history presents to the Emergency Department with four days of vaginal bleeding and lower abdominal cramping. She reports taking misoprostol four days ago for a medical abortion at approximately 8 weeks gestational age. She passed a large blood clot shortly after taking misoprostol, but she continues to have persistent vaginal bleeding and abdominal pain, soaking one pad every two hours. She denies fever or foul-smelling discharge. Her vital signs are within normal limits except for mild tachycardia. Abdominal examination reveals a soft abdomen with mild suprapubic tenderness. On pelvic examination, the cervical os is closed with mild oozing of dark red blood, without cervical motion tenderness or visible fetal tissue.
Given her symptoms and examination findings, a point-of-care ultrasound (POCUS) scan was performed to evaluate for retained products of conception (RPOC).
Making the diagnosis
RPOC can manifest in patients after fetal delivery, medical or surgical abortion, or miscarriage. Early identification of RPOC using POCUS is important to identify the source and location of the bleeding. Failure to identify RPOC can lead to worsening bleeding and increases the risk of infections such as endometritis. Obtaining a history prior to performing POCUS is paramount to help focus the POCUS examination.
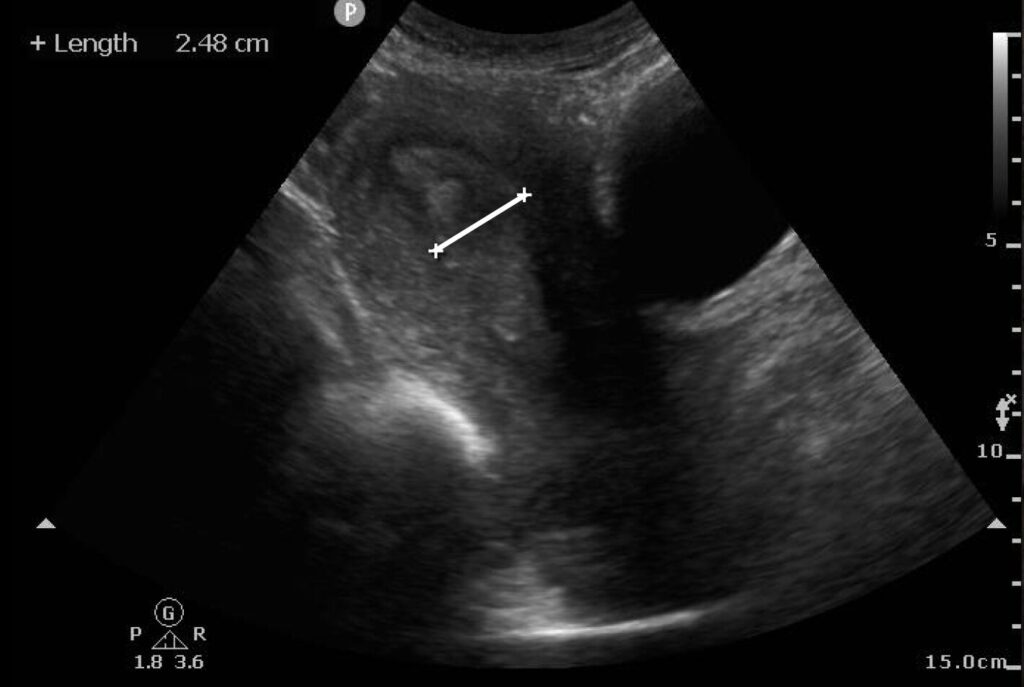
POCUS for identification of RPOC starts with visualization of the uterus and endometrial stripe, using the bladder and vaginal stripe as landmarks (Image 1) (Video 1). To perform the scan, place the probe in the sagittal plane superior to the pubic brim. The normal uterus appears homogeneous and isoechoic or hyperechoic. The endometrium is located centrally within the uterus and appears more hyperechoic. Fanning the probe can help identify the endometrium, which then can be measured within the uterus in the sagittal plane, at the thickest area of echogenicity, without the inclusion of fluid or myometrium (Image 2) if there is concern for RPOC.
Image 1: Sagittal view of the uterus in early pregnancy

Video 1: Sagittal view of the uterus
Image 2: Measured endometrium that appears thickened and heterogeneous
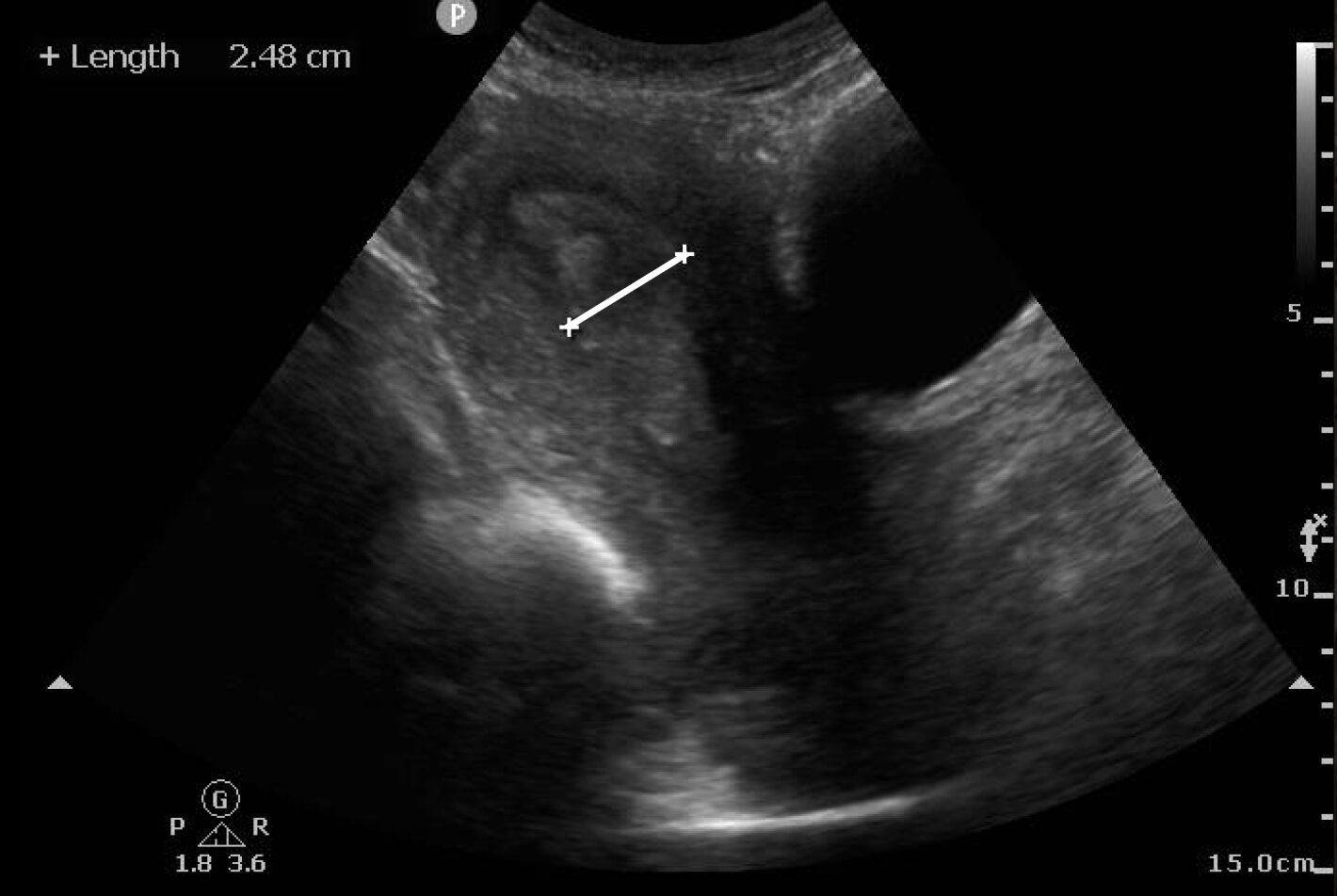
Endometrial thickness measurements using ultrasound have been shown to be more reliable for diagnosis RPOC than history alone.1-4 RPOC often appears with a heterogeneously thickened endometrium > 10 mm, but other studies cite > 15 mm for the diagnosis.5 Ideal visualization of RPOC occurs through transvaginal POCUS (Image 3) (Video 2), but transabdominal POCUS can also be accurate in diagnosing RPOC (Image 4) (Video 3). To date, only one study has evaluated for RPOC using POCUS, which demonstrated 93.8% specificity and 79.0% sensitivity for identifying RPOC.6
Image 3: Transvaginal ultrasound showing a thickened endometrial stripe (white star) suggestive of retained products of conception
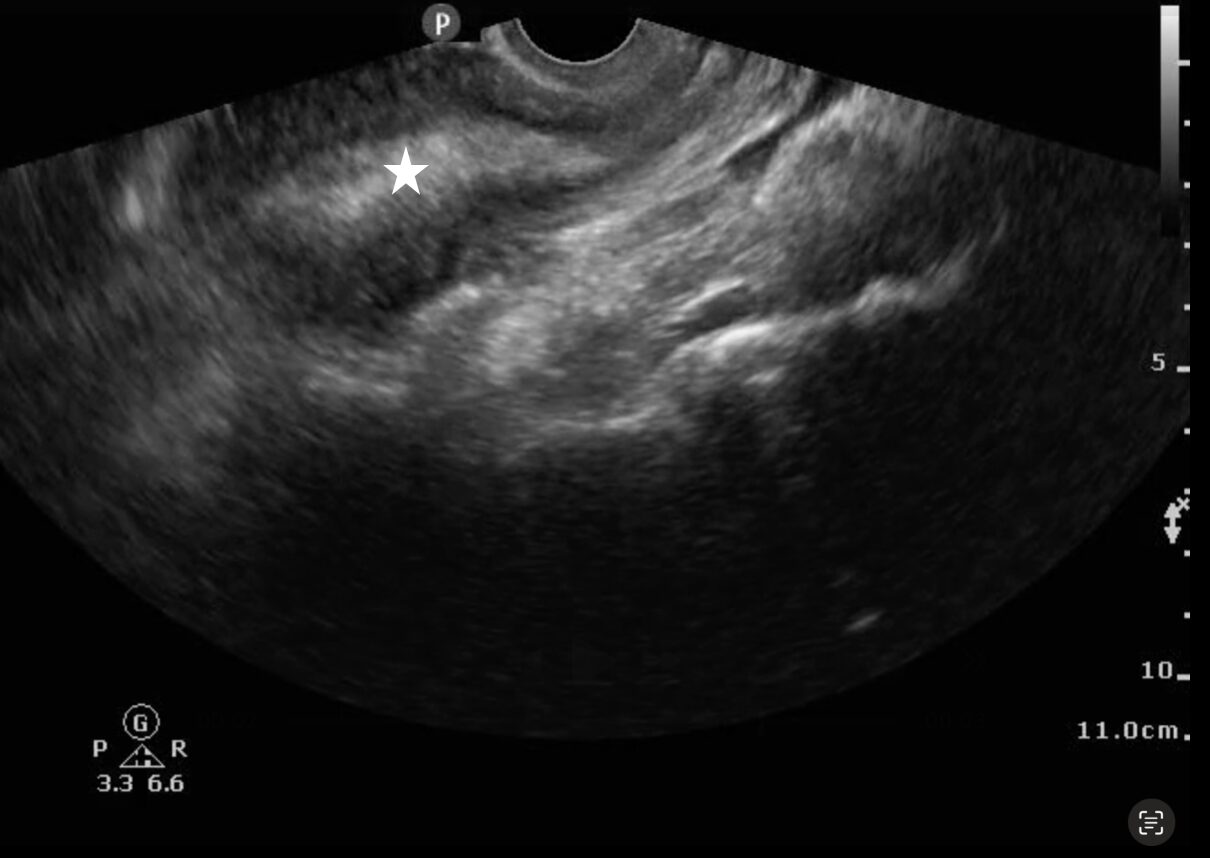
Video 2: Transvaginal ultrasound showing a thickened endometrial stripe suggestive of retained products of conception
Image 4: Transabdominal ultrasound showing a thickened endometrial stripe (white star)
suggestive of retained products of conception 
Video 3: Transabdominal ultrasound showing a thickened endometrial stripe suggestive of retained products of conception
Computed tomography (CT) plays a limited role in diagnosing RPOC but may be more useful in complex cases or when a significant amount of time has passed since pregnancy termination.7 In most cases, ultrasound is sufficient for diagnosis and should be the first-line imaging modality.
The role of color Doppler
Color Doppler can be applied to the endometrium to increase the specificity for RPOC, as placental tissue within the endometrium will demonstrate vascularity (Video 4). Doppler can also help differentiate between RPOC and a hematometra, i.e. a blood clot within the uterus. However, these conditions are managed similarly, and thus the differentiation is not as critical.
Video 4: Transabdominal ultrasound showing retained products of conception with color Doppler flow
Nevertheless, a recent study by Ashkar Majadla et al. showed up to 25% of patients with confirmed RPOC had no vascularity on ultrasound.8 The study by Boivin et al. was retrospective and only a small number of studies included the use of Doppler, suggesting that the diagnosis can be made without use of color Doppler.6 If color Doppler is applied, look for a signal over the endometrium. If there is no clear evidence of miscarriage (as the endometrium may appear thickened in early pregnancy), avoid the use of color Doppler in early pregnancy given the principle of ALARA (as low as reasonably achievable) for fetal radiation exposure,
Case Resolution
The patient was found to have RPOC on the POCUS scan, the OB/GYN service was consulted, and they administered a repeat dose of misoprostol after shared decision-making. The patient was discharged home to follow-up with OB/GYN in the outpatient setting.
Pearls
- A full bladder allows for better visualization of the uterus using transabdominal ultrasound, whereas an empty bladder improves transvaginal visualization of the uterus.
- The endometrium is measured within the uterus in the sagittal plane, at the thickest area of echogenicity, without the inclusion of fluid or myometrium. In RPOC, the endometrium appears heterogenous
- For transabdominal ultrasound, increasing pressure to displace bowel gas can improve visualization of the uterus.
- Endometrial thickness can vary with the menstrual cycle (i.e. it is thicker during the secretory phase and thinner during menstruation), so this history factor is important for the diagnosis of RPOC.
- Placing color Doppler over the endometrium to visualize placental vascularity can improve the accuracy of identifying RPOC.
Pitfalls
- In early pregnancy, there can be thickening of the endometrium > 1.0 cm, which can mimic RPOC.
- Mimics of RPOC include cervical stenosis, endometritis, molar pregnancy, and ectopic pregnancy.
- A fibroid uterus can appear heterogenous with hypoechoic masses and makes the diagnosis of RPOC more difficult.
- A transvaginal ultrasound may better visualize the endometrium as compared to transabdominal ultrasound.
Conclusion
POCUS can help identify RPOC in patients with recent spontaneous abortion, elective abortions, or post-delivery. Both transvaginal and transabdominal POCUS can adequately visualize the endometrium allowing for identification of RPOC.
References
- Malvern J, Campbell S, May P. Ultrasonic scanning of the puerperal uterus following secondary postpartum haemorrhage. J Obstet Gynaecol Br Commonw. Apr 1973;80(4):320-4. doi:10.1111/j.1471-0528.1973.tb11199.x
- Achiron R, Goldenberg M, Lipitz S, Mashiach S. Transvaginal duplex Doppler ultrasonography in bleeding patients suspected of having residual trophoblastic tissue. Obstet Gynecol. Apr 1993;81(4):507-11.
- Alcázar JL, Baldonado C, Laparte C. The reliability of transvaginal ultrasonography to detect retained tissue after spontaneous first-trimester abortion, clinically thought to be complete. Ultrasound Obstet Gynecol. Aug 1995;6(2):126-9. doi:10.1046/j.1469-0705.1995.06020126.x
- Rulin MC, Bornstein SG, Campbell JD. The reliability of ultrasonography in the management of spontaneous abortion, clinically thought to be complete: a prospective study. Am J Obstet Gynecol. Jan 1993;168(1 Pt 1):12-5. doi:10.1016/s0002-9378(12)90877-7
- Hamel CC, van Wessel S, Carnegy A, et al. Diagnostic criteria for retained products of conception-A scoping review. Acta Obstet Gynecol Scand. Dec 2021;100(12):2135-2143. doi:10.1111/aogs.14229
- Boivin Z, Barber D, Chimileski B, et al. Accuracy of point-of-care ultrasound in diagnosing retained products of conception. The American journal of emergency medicine. 2025/01/13/ 2025;doi:https://doi.org/10.1016/j.ajem.2025.01.032
- Lee NK, Kim S, Lee JW, et al. Postpartum hemorrhage: Clinical and radiologic aspects. Eur J Radiol. Apr 2010;74(1):50-9. doi:10.1016/j.ejrad.2009.04.062
- Ashkar Majadla N, Abu Shqara R, Haj S, et al. Sonographic evaluation of retained products of conception within 48 h following delivery: a retrospective cohort study. Arch Gynecol Obstet. Published online August 12, 2024. doi:10.1007/s00404-024-07688-8