Authors: William Bost, MD (Emergency Medicine Resident, Carolinas Medical Center, Charlotte, NC), Ann-Jeannette Geib, MD (Emergency Medicine Attending, Medical Toxicologist, Carolinas Medical Center, Charlotte, NC) // Reviewed by: Cynthia Santos, MD (@Cynthia Santos, MD); Alex Koyfman, MD (@EMHighAK); and Brit Long, MD (@long_brit)
Case:
A 16-year-old female presents with vomiting and mild agitation after ingestion of an entire bottle of diet pills, Zantrex-3(™), a supplement containing yerba mate, guarana, green tea, and caffeine. In the ED, she was in sinus tachycardia with a rate of 140 with BP 95/40. Her blood sugar was mildly elevated at 170, and she was tremulous and mildly agitated. She had active vomiting and frequent diuresis. Approximately 30 minutes after arrival, she had a generalized tonic-clonic seizure lasting 10 minutes.
She received midazolam 5 mg IV x 2, two 20 cc/kg IV fluid boluses, and was intubated. Labs showed potassium 2.9, bicarb 25, lactate 2.9, CPK 2000, creatinine 1.5. In the ED she develops frequent runs of narrow complex tachycardia at a rate of 180. What are your next steps in the management of this patient?
Questions:
1. What are the systemic effects of a methylxanthine overdose?
2. How can you treat the cardiovascular effects of a methylxanthine overdose?
Background:
- Caffeine is a ubiquitous substance that is available in increasing formulations, including caffeine tablets, drinks, and as an additive in many foods.
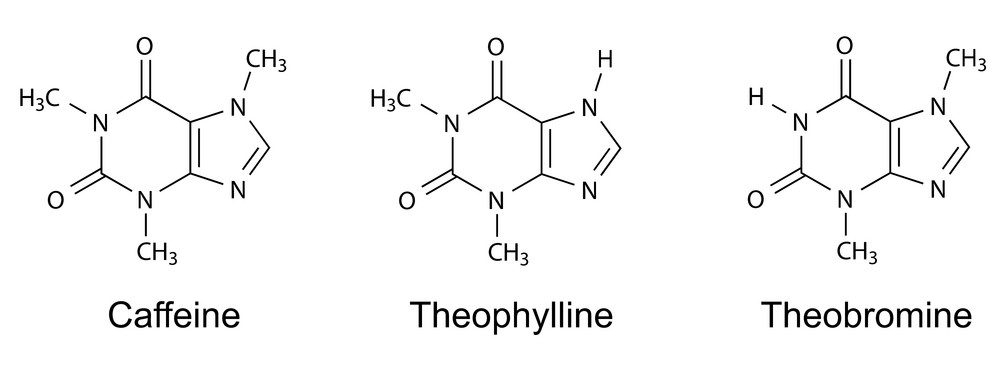
- Therapeutically it is used to treat headaches and neonatal apnea and bradycardia. It is part of a class of drugs called methylxanthines, which includes theophylline and theobromine.
- Theophylline is a bronchodilator once commonly used for asthma, though still uncommonly prescribed.
- Theobromine is commonly found in chocolate, but we have limited information on human toxicity (1).
- Metabolism is hepatic via CYP 2A1 for caffeine and 1A2 for theophylline.
- Inducing agents include tobacco, meaning tobacco cessation in a COPD patient taking theophylline will abruptly increase levels.
- The therapeutic window for caffeine is wide relative to theophylline, meaning toxicity is rarely accidental with most reported cases being from intentional self-harm.
- Methylxanthines affect nearly every organ system therapeutically and in toxicity.
- The mechanism of action is both as an adenosine antagonist and cAMP phosphodiesterase inhibitor.
- Adenosine antagonism causes endogenous release of catecholamines. It also acts as an anticonvulsant. Phosphodiesterase inhibition increases intracellular cAMP and calcium, as well as beta agonism and enhancement of its second messenger system.
Pearls:
- Gastrointestinal effects include protracted nausea and vomiting via acid secretion and smooth muscle relaxation. Pulmonary effects include bronchodilation as well as CNS driven tachypnea.
- CNS effects include mood stimulation, improved performance, anxiety, and agitation at therapeutic levels; in toxicity can cause refractory seizures via adenosine antagonism. Seizures are refractory to phenytoin and fosphenytoin and can be refractory to benzodiazepines.(2).
- Musculoskeletal effects include increased contractility, decreased fatigue, and increased oxygen consumption, which makes caffeine a common pre-workout supplement. In toxicity it can cause rhabdomyolysis, possibly via sequestered intracellular calcium, best treated with fluids and benzodiazepines.
- Metabolic effects are due to the overall hyperadrenergic state, including a lactic acidosis. Hypokalemia due to an intracellular shift from beta stimulation is common, though it should be cautiously treated due to possible concurrent rhabdomyolysis that would lead to intracellular release of potassium.
- Cardiovascular effects vary and are due to catecholamine excess. They include arrhythmias, refractory hypotension, and myocardial infarction.
- Atrial and ventricular tachydysrhythmias are the most common cause of death in methylxanthine overdose and include supraventricular tachycardia (SVT), multifocal atrial tachycardia, ventricular tachycardia, and premature ventricular contractions; these are more often seen in acute on chronic toxicities (3).
- SVT may be refractory to adenosine and cardioversion, though SVT can be responsive to beta-blockers, calcium channel blockers, and benzodiazepines. Calcium channel blockers may improve outcomes in SVT (4).
- Electrolyte abnormalities should be cautiously corrected in the setting of dysrhythmias.
- Hypotension can be due to volume depletion from emesis and primary beta receptor-induced vasodilation.
- Fluid resuscitation should be followed by vasopressors, likely phenylephrine and norepinephrine, though beta-agonists should be avoided, due to theoretical worsening of beta mediated dysrhythmias and vasodilatory shock.
- Vasodilatory shock can be treated with short-acting beta-blockers such as esmolol (5-7).
- Subendocardial myocardial infarction has been reported in caffeine overdose (8).
- Enhanced elimination should be considered in all cases including multidose activated charcoal (MDAC), which is known to remove theophylline via “gut dialysis”.
- MDAC may assist in theophylline overdose and it can be considered for caffeine, which is metabolized to theophylline (9).
- Hemodialysis (HD) should be considered based on the clinical presentation of the patient, as drug levels are infrequently available in a timely manner. Consider HD in all cases of refractory shock, dysrhythmias, or refractory seizures.
Take Home Points:
- Methylxanthine toxicity affects nearly every organ system. Chronic theophylline toxicity should be considered in patients with altered mental status, vomiting, and means of exposure.
- Management of dysrhythmias involves calcium channel and beta-blockers.
- Seizures should be treated with benzodiazepines.
- Management of hypotension involves fluid resuscitation, alpha agonists, and beta-blockers.
- Consider MDAC if able to tolerate enteral intake, and hemodialysis for severe cases.
Case Conclusion:
The patient was given IV diltiazem boluses, with return to sinus tachycardia, with no repeat episodes of SVT in the ED. A caffeine level was sent, though it was decided to pursue HD before a level returned. The patient had a full recovery following resuscitation and HD. Caffeine level, resulted 3 days later, was 52 ug/mL.
References:
- Hoffman, R.S., Howland, M.A., Lewin, N.A., Nelson, L.S., Goldfrank, L. R. (2015). Methylxanthines and Selective beta 2-Adrenergic Agonists In 10e, Goldfrank’s Toxicologic Emergencies. London: Prentice-Hall.
- Jacobs M.H., Senior R.M. Theophylline toxicity due to impaired theophylline degradation. Am Rev Respir Dis. (1974);110:342–345.
- Shannon M: Life-threatening events after theophylline overdose: a 10-year prospective analysis. Arch Intern Med
- . (1999);159:989–994.Whitehurst V.E., Joseph X, Vick J.A. et al. Reversal of acute theophylline toxicity by calcium channel blockers in dogs and rats. Toxicology. (1996);110:113–121
- Dettlo R.W., Touchette M.A., Zarowitz B.J. Vasopressor-resistant hypotension following a massive ingestion of theophylline. Ann Pharmacother
- (1993);27:781–784Biberstein M.P., Ziegler M.G., Ward D.M. Use of beta-blockade and hemoperfusion for acute theophylline poisoning. West J Med. (1984);141:485–490.
- Price K.R., Fligner D.J. Treatment of caffeine toxicity with esmolol. Ann Emerg Medicine. (1996);19: 44-46.
- Forman J, Aizer A, Young CR: Myocardial infarction resulting from caffeine overdose in an anorectic woman. Ann Emerg Med. (1997);29(1):178-80
- Aldridge A, Aranda JV, Neims AH: Caffeine metabolism in the newborn. Clin Pharmacol Ther. (1979); 25:447-453.