Originally published on Ultrasound G.E.L. on 2/18/19 – Visit HERE to listen to accompanying PODCAST! Reposted with permission.
Follow Dr. Michael Prats, MD (@PratsEM) from Ultrasound G.E.L. team!
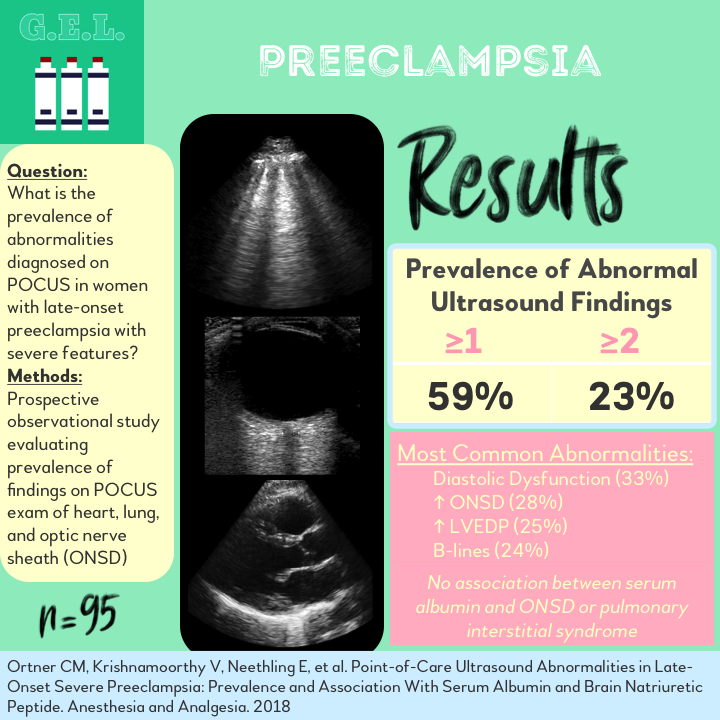
Point-of-Care Ultrasound Abnormalities in Late-Onset Severe Preeclampsia: Prevalence and Association With Serum Albumin and Brain Natriuretic Peptide
Anesthesia and Analgesia Epub Sept 2018 – Pubmed Link
Take Home Points
1. Point-of-care ultrasound can diagnose pulmonary interstitial fluid, increased optic nerve sheath diameter, and cardiac dysfunction in patients with late onset preeclampsia.
2. In this study, 59% of patients had 1 or more POCUS abnormality, with diastolic dysfunction being the most common.
3. More information is needed to know how POCUS can be helpful in this population.
Background
Pre-eclampsia is a real bummer. It’s a severe hypertensive disorder occurring in pregnancy that can result in multiple organ dysfunctions. Unbeknownst to much of the world, point-of-care ultrasound (POCUS) has actually been used to find some of these manifestations of severe preeclampsia. For example, preeclampsia can cause pulmonary edema, which we know shows up well on ultrasound of the lungs. POCUS can also diagnose increased optic nerve sheath diameter in these women, which could indicate an increased intracranial pressure from cerebral edema. Since not much is known about how ultrasound might be useful in this population, this study just aims to see how common these findings are in patients with the disease. A second goal of the study is to figure out if a low albumin correlates with these ultrasound findings, as a low oncotic pressure is one of the suggested explanations for the pathophysiology of pre-eclampsia.
Questions
What is the prevalence of abnormalities diagnosed on POCUS in women with late-onset preeclampsia with severe features?
Is there an association between pulmonary interstitial syndrome or optic nerve sheath diameter and maternal albumin level?
What is the association between cardiac dysfunction to a serum brain-natriuretic peptide (BNP), albumin, and the other POCUS findings?
Population
Single center in Cape Town, South Africa
Inclusion:
- Greater than 34 weeks gestation
- Preeclampsia with severe features
Exclusion
- In labor
- Unable to understand study
- Chronic pulmonary disease, HIV, collagen disorders, lithium intoxication, chronic renal or hepatic disease, urinary tract infection, chorioamnionitis, intrauterine fetal death, BMI > 50, acute asthma
Design
Prospective observational cohort study
Patients diagnosed with preeclampsia with severe features were enrolled
All received:
- Obstetric ultrasound
- Magnesium sulfate
- Fluid restriction
- BP management
- Cardiotocograph was analyzed for fetal well being and could lead to cesarean section.
This was all independent of the study investigation.
As part of the study, the patients received a serum BNP and albumin.
Then these patients received their POCUS – cardiac, lung, and optic nerve sheath diameter (see below for details).
These were each defined as positive or negative based on definitions below.
These findings were analyzed to look for associations between the serum tests, the ultrasound findings, clinical features and a few other things. Because of the large number of comparisons, they adjusted the statistical significance level to P < 0.025 (that is a normal thing to do).
Power analysis: Needed 80 patients to show difference of 0.6 g/dL in albumin between those with and without POCUS findings of PIS or ONSD.
Who did the ultrasounds?
Two of the study investigators, not involved in patient care
The Scan
Phased array probe for Cardiac and Pulmonary

Linear probe for ONSD

Cardiac Protocol
- Placed in left lateral decubitus
- Quinones method for left ventricular systolic function, uses linear measurements of LV cavity, may not be most accurate
- Also, used fractional shortening and “eyeball” method.
- Diastolic function evaluated with mitral valve inflow on pulsed wave doppler and tissue doppler of mitral valve annulus. Dysfunction defined by low E’.
- Calculated LVEDP, defined as E/E’ ≤8 or between 9 and 13 + BNP > 200.
Thoracic Protocol
- 8 regions (2 anterior, 2 lateral on each side)
- Pulmonary interstitial syndrome diagnosed as ≥3 Blines in two regions on both sides. Also given a score equalling total number of B-lines in all windows
Optic Nerve Sheath
- Patients supine, head elevated 30º
- Measure nerve in both transverse and sagittal plane in both eyes, took mean of all four measurements. Increased ICP defined as ONSD >5.8 mm.
The Evidence Atlas – Pulmonary
Results
N = 95
- Mean age 27
- Mean gestation 39 weeks
- Mean BMI 31.3 kg/m2
- Mean SBP 165
- Severe features were most commonly hypertension (76%), headache/visual disturbance (76%), or severe proteinuria (37%)
- Similar between those who had + POCUS findings versus those who did not
- More headaches and visual disturbances in POCUS positive (84%) compared to POCUS negative (64%)
Primary Outcomes
Prevalence of Ultrasound Findings
- 59% had ≥1 ultrasound abnormality
- 36% had 1 ultrasound abnormality, 23% had ≥2
- Increased ONSD 28% (CI 20-39%)
- Pulmonary interstitial syndrome 24% (CI 16-34%)
- Systolic dysfunction 10% (CI 4-17%)
- Diastolic dysfunction 33% (CI 23-43%)
- Raised LVEDP 25% (CI 16-36%)
Association with Serum Markers
No association between PIS or ONSD and serum albumin
POCUS + mean albumin 31.6 g/L
POCUS – mean albumin 33.4 g/L (p = 0.03)
Secondary Outcomes
No association between serum albumin and any type of cardiac dysfunction
BNP was associated with systolic dysfunction, diastolic dysfunction, and increased LVEDP
POCUS + mean BNP 304.0 pg/mL
POCUS – mean BNP 124.3 pg/mL (p = 0.03)
Other Findings
PIS was associated with lower LV systolic function, higher LV diameter at end systole, diastolic dysfunction
BNP was not accurate for diagnosing any type of cardiac dysfunction
- Sensitivity ranged from 50-57%
- Specificity ranged from 72-84%
Good intra- and inter-observer agreement
Limitations
Patients were from South Africa. This limits the external validity to other populations, especially when discussion the incidence of disease which can certainly vary geographical.
Lots of exclusion criteria. Understandably, they didn’t want other factors that could affect either their POCUS or their serum markers, but excluding patients with urinary infection? Excluding obese women? That can limit the applicability of the examination.
Was POCUS being used to show that albumin would change or was albumin being used to show POCUS findings would change? The introduction to the paper makes it seem that there is only minimal evidence to support either relationship, yet they seem to use them to confirm each other as accurate. They did their power calculation based on finding a difference in albumin, that makes me think that the albumin was being used as the dependent variable here. The bottom line is that it would have been nice to have a control group so that you could compare BOTH the POCUS findings and the serum markers to controls without severe pre-eclampsia. Even if the point was just so show the prevalence of the POCUS findings in this population, we really don’t know if that matches the prevalence of disease because there was no standard to check it against.
Discussion
Seems that the pulmonary edema in preeclampsia is associated with cardiac dysfunction. This may provide some theories as to how all of this dysfunction in orchestrated. Since the albumin did not seem associated, it might be the case that the colloid osmotic pressure does not contribute as much, at least in late-onset preeclampsia.
What to do with this information? Well – based on this information, we know that point-of-care ultrasound can find things in preeclampsia. Unfortunately, we don’t know what findings those things means for those patients. Even though this information is merely descriptive, I think it is quite thought provoking. It makes sense that POCUS would be able to find evidence of pulmonary edema, elevated intracranial pressure, and cardiac function that might occur in these patients. This is a good start to say that POCUS might be helpful – either diagnostically or prognostically. More research is needed and it will be interesting to see if there is a role for POCUS with these patients.
Take Home Points
1. Point-of-care ultrasound can diagnose pulmonary interstitial fluid, increased optic nerve sheath diameter, and cardiac dysfunction in patients with late onset preeclampsia.
2. In this study, 59% of patients had 1 or more POCUS abnormality, with diastolic dysfunction being the most common.
3. More information is needed to know how POCUS can be helpful in this population.
Our score

Expert Reviewer for this Post

Joseph Pare, MD MHS @jrpare29
Director of Ultrasound Research in the Department of Emergency Medicine at Boston University School of Medicine
Reviewer’s Comments
A few additional comments: the mean BMI was >30. I am not sure if the authors made BNP adjustments for BMI as this can be falsely low in an obese population, however I presume the increased BMI is a result of the pregnancy in many cases and I am unsure if a correction is necessary based on this “obesity” from pregnancy. I would also state that with only 80 patients and only a handful of people with positive findings, and then also doing a correction for multiple hypothesis testing, this study is hard to get excited about. If they had just done one test the PIS on POCUS would have been significant right? but they also needed to check OSND, etc….. Perhaps with only 80 patients they shouldn’t have tried to perform multiple hypothesis testing.
Cite this post as
Michael Prats, MD. POCUS in Preeclampsia. Ultrasound G.E.L. Podcast Blog. Published on February 18, 2019. Accessed on October 02, 2020. Available at https://www.ultrasoundgel.org/63.