
Reviewed by: Steven Field, DO, FAEMUS, FACEP (Associate Professor of EM, UT Southwestern); Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Case
A 68 year-old male presents with right flank pain that began four days prior after he tripped on his cat and fell sideways against the corner of his television stand. He reports that the pain is sharp, and worse with taking deep breaths, moving, and coughing. He is afebrile, saturating well on room air and the remainder of his vital signs are within normal limits. Physical examination is remarkable for an area of ecchymosis and point tenderness over the right inferior ribs with right thoracic paraspinal tenderness. His pain appears to worsen with changes in position. Imaging is remarkable for a right-sided nondisplaced posterior 9th rib fracture. He was treated with a multimodal pain management approach, but with minimal improvement. A plan is made to perform an erector spinae plane block and the patient consented to the procedure.
Background
Multimodal pain control is an increasingly attractive strategy for acute pain in the emergency department (ED). Now, more than ever, there is increased awareness that opioids have addictive potential and cause many adverse effects. Patients presenting to the ED in acute pain are often undertreated.1 Thanks to their proficiency in point-of-care-ultrasound (POCUS), emergency physicians possess the distinctive capability to execute nerve blocks in the ED. This strategy toward pain management in the acute setting is growing increasingly popular due to its non-addictive potential and targeted therapy.2
An erector spinae plane block (ESPB) was first described for neuropathic rib pain in 2016 by Forero et. al.3 The ESPB is a planar block that targets the area below the fascial layer and spreads within the fascial space to bathe the underlying nerves in anesthetic. Instead of injecting directly around one specific nerve (e.g. for median and ulnar nerve blocks), this procedure is targeted at anesthetizing multiple nerves within the fascial plane. ESPBs are widely used in surgical settings for management of operative pain from breast, spine, abdominal, cardiac, urologic, and thoracic surgeries.4 The anesthetic has been shown to reach the dorsal and ventral rami of the thoracic and abdominal nerves, and has been shown to spread 3-4 levels both cephalad and caudad from the injection site. This allows for both somatic and visceral anesthesia.5 An MRI study, evaluating an ESPB at T10, showed anesthetic spread from T5 to T12, with epidural and transforaminal spread, which may account for the visceral anesthetic benefits.6
Indications for ESPB 6,7
| Rib Fractures | Acute Pancreatitis | Kidney Stone |
| Shingles | Appendicitis | Compression Fracture |
Complications of ESPB 4
| Infection | Damage to Surrounding Structures | Epidural Injection |
| Bleeding | Local Anesthetic Systemic Toxicity (LAST) | Pneumothorax |
Contraindications of ESPB 8
| Contraindications | Infection over injection site | Patient refusal |
| Relative Contraindications | Platelet dysfunction | Anticoagulation status |
Thoracic Innervation
Diagram showing the anatomy of the transverse process with the overlying erector spinae.9 Needle tip is seen below the erector spinae fascial plane. (NYSORA)
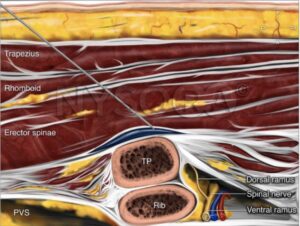
Diagram depicting transverse anatomic location of ESPB (Foreo, M) 10

How To Perform:
- Consent the Patient
- Obtain the Equipment:
- US machine with linear probe
- Antiseptic (e.g. Chlorhexidine, Betadine)
- Sterile US cover
- Sterile US gel
- Sterile gloves
- Sterile towels
- Needle apparatus
- Nerve block needle (needle with pre-connected extension tubing) or
- Spinal Needle (18-22 g) attached to IV extension tubing
- 20 cc syringe or 60 cc syringe
- 3-way stopcock (optional, but useful to toggle between saline or local anesthetic without removing and switching syringes)
- 5 cc of 1% lidocaine for skin wheal – 10 cc syringe with 25 gauge needle
- 20-30 mL of long acting anesthetic of choice (e.g. 0.5% ropivacaine or 0.25% bupivacaine) diluted with normal saline to adhere to maximum allowable dose*
*use MD Calc Local Anesthetic Dosing Calculator to calculate maximum allowable dose, may mix with saline to obtain proper volume
3. Prepare Room
Place patient on cardiac monitor and have available airway equipment and crash cart. Have intralipid readily available for treatment of local anesthetic systemic toxicity.
4. Perform Procedure
Position patient – Prone, lateral decubitus, or sitting
Set up needle apparatus- attach saline syringe to extension tubing, flush the line to eliminate air
Prepare and sterilize site
Place US sagittally and midline over spinous processes
Slide US laterally to parasagital plane and identify lateral structures
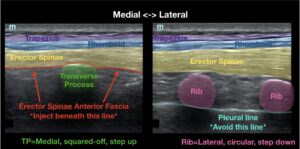
Distinguish TP from ribs.
TP will be relatively medial and superficial, with a flatter “squared-off” appearance
Ribs will be relatively lateral and deeper, with a rounder shape, and will be seen overlying the pleural line seen with lung sliding
Center US probe over TP
Identify erector spinae fascial plane- this should be the fascial plane superiorly apposed to the TP
Anesthetize skin by injecting lidocaine to form a skin wheal
Use in-plane needle guidance to position needle tip below the erectae spinae fascial plane:
- May feel slight pop when traversing fascial plane
- Aim at “corners” or superior or inferior margins of TP to ensure needle tip is just deep to fascial plane
- Needle contacting the most posterior surface of the TP may prevent it from entering sub-fascial plane
Hydrodissect with 1-2 cc of sterile saline to confirm proper injection location
Should see Erector Spinae fascial plane “lifting off” the TP
Switch from saline to prepared anesthetic
Administer 20-30 ccs of prepared anesthetic
Observe on cardiac monitor for at least 30 minutes after procedure.13
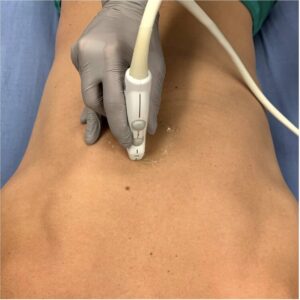
A photograph demonstrating appropriate para-sagittal positioning of the linear probe (POCUS Atlas).7

Nerve block apparatus set up. Needle connected to extension tubing, connected to syringe (AliEM- Grey, M).11

Ultrasound correlation to anatomy over the spinous process, transverse process, and ribs (Highland US).12
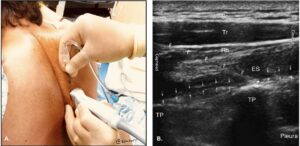
Injection technique demonstrated in picture A, needle placement visualized in picture B between the transverse process and erector spinae (Highland US).12
(UTSW)
Video 1: Needle entering the space of the ESP
Video 2: Hydrodissection to guide proper needle placement
Video 3: Post-injection, ESP space with ropivacaine
Case Resolution
20 mL of 0.5% ropivacaine is injected to the ESP at the T9 region. Patient has significant relief with the ESP block and is discharged with multimodal pain medicine and follow up.
References
- Carter D, Sendziuk P, Eliott JA, Braunack-Mayer A. Why is Pain Still Under-Treated in the Emergency Department? Two New Hypotheses. Bioethics. 2016;30(3):195-202. doi:10.1111/bioe.12170
- PubMed: Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. Erector spinae plane (ESP) block: a new paradigm in regional anesthesia and analgesia. Reg Anesth Pain Med. 2016;41(5):621-627. doi:10.1097/AAP.0000000000000451.
- PubMed: Forero M, Rajarathinam M, Adhikary S, Chin KJ. The Erector Spinae Plane Block. Reg Anesth Pain Med. 2017;42(3):377-382. doi:10.1097/AAP.0000000000000570.
- UCSF Pain Management Center: Urits I, Charipova K, Gress K, et al. Erector Spinae Plane Block. UCSF Pain Medicine. Accessed May 26, 2024. https://pain.ucsf.edu/fascial-plane-blocks/erector-spinae-plane-esp-block.
- Europe PMC: Forero M, Rajarathinam M, Adhikary SD, Chin KJ. Erector spinae plane (ESP) block: An overview. Europe PMC. Published 2017. Accessed May 26, 2024. doi:10.1016/j.bja.2017.01.012.
- Springer Link: Chin KJ, Malhas L, Perlas A. The Erector Spinae Plane Block: A Novel Analgesic Technique in Thoracic Neuropathic Pain. Curr Anesthesiol Rep. 2017;7(3):276-282. doi:10.1007/s40140-017-0231-2.
- POCUS Atlas: ESP block. POCUS Atlas. Accessed May 26, 2024. https://www.thepocusatlas.com/thoracoabdominal-blocks#ErectorSpinae.
- NCBI Bookshelf: Arshad Z, Ahmad T. Practical Anesthetic Management: An Erector Spinae Plane Block for Lumbar Spinal Surgery. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022. Accessed May 26, 2024. https://www.ncbi.nlm.nih.gov/books/NBK545305/.
- NYSORA: Chin KJ. Erector Spinae Plane Block. NYSORA. Accessed May 26, 2024. https://www.nysora.com/erector-spinae-plane-block/.
- ResearchGate: Forero M, Rajarathinam M, Adhikary S, Chin KJ. Schematic diagram of erector spinae plane block. ResearchGate. Published 2017. Accessed May 26, 2024. https://www.researchgate.net/figure/Schematic-diagram-of-erector-spinae-plane-block-A-needle-was-inserted-into-the_fig1_343767070.
- ALiEM: Grey M, Avila A, Cardwell J. Fascia Iliaca Nerve Block. ALiEM. Published 2016. Accessed May 26, 2024. https://www.aliem.com/fascia-iliaca-nerve-block/.
- Highland Ultrasound: Boswell L. Erector Spinae Plane (ESP) Block. Highland Ultrasound. Accessed May 26, 2024. https://highlandultrasound.com/erector.






