Authors: Sara Adibi, MD (EM Attending Physician, Baylor Scott & White – Centennial & Frisco) // Reviewed by: Edward Lew, MD (@elewMD); Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Clinical Case
A 69-year-old female with a history of CAD and smoking presents for palpitations along with bilateral lower extremity pain and weakness x 6 hours. She denies any back pain, recent trauma, or injury. She appears to be in atrial fibrillation with a rapid ventricular rate, which she denies any known prior history of such. You start to consider your differential diagnoses and which tests to order…but then the nurse informs you that she is beginning to develop discoloration to the lower extremities and has decreased dorsalis pedis pulses. How does this change your line of thinking?
Background
Acute aortic occlusion (AAO) is a rare and emergent vascular phenomenon, and despite advances in both diagnosis and treatment the prognosis still remains poor, ranging anywhere from 21-50%. 1 There are two major causes of occlusion: embolism and thrombosis. Previously embolism was the most common etiology, causing nearly 50-65% of cases.1,2 With improved prevention of cardioembolic events due to anticoagulation medications (thus reducing the number of embolic events)1 and/or an aging population with more advanced atherosclerotic disease, thrombosis is now the most common cause.
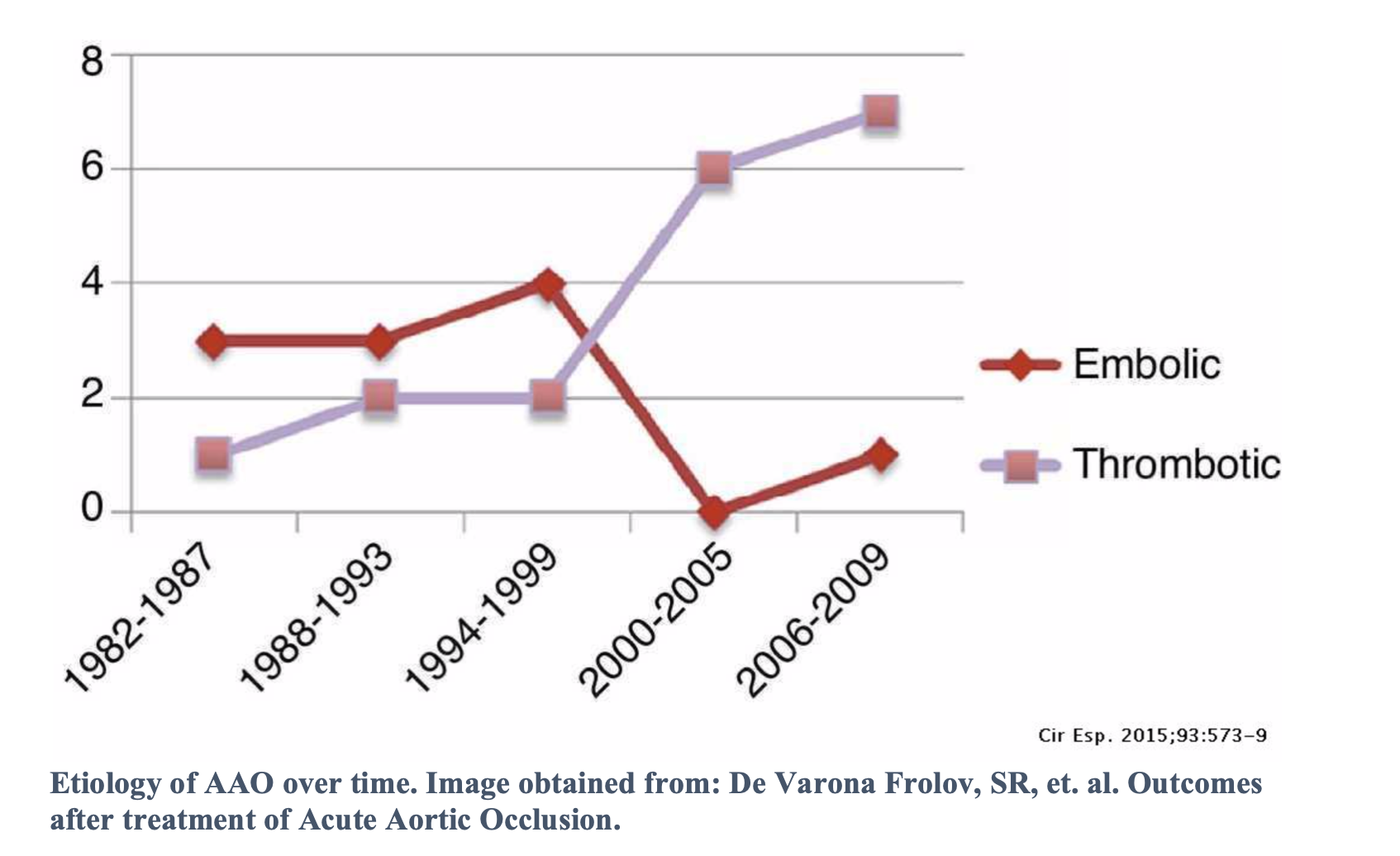
Pre-existing atherosclerosis combined with a low flow state, such as after major surgery, or with a hypercoagulable state can precipitate thrombosis and therefore acute aortic occlusion.2 Risk factors for embolism include valvular heart disease and female gender. Whereas for thrombosis, risk factors include smoking, diabetes, and infrequently blunt abdominal trauma (force on the fixed aorta causes disruption of the intima and subsequent thrombosis).3
Presentation
Clinically, these patients can vary in presentations depending on level of occlusion of the aorta. Infrarenal is the most common aortic location. Symptoms may include acute onset of pain, paralysis or weakness, and/or mottling to the lower extremities, as well as abdominal pain. If there is evidence of renal artery occlusion, acute hypertensive crisis may be the sole presenting symptom.4 With thrombotic occlusions there can also be development of collateral circulation which can delay symptomatology and therefore time to presentation. With these varied pictures it is easy to see how delay in diagnosis may occur, favoring other potential causes such as stroke, cauda equina, aortic dissection, etc, and therefore potentially worsening the prognosis.
Evaluation
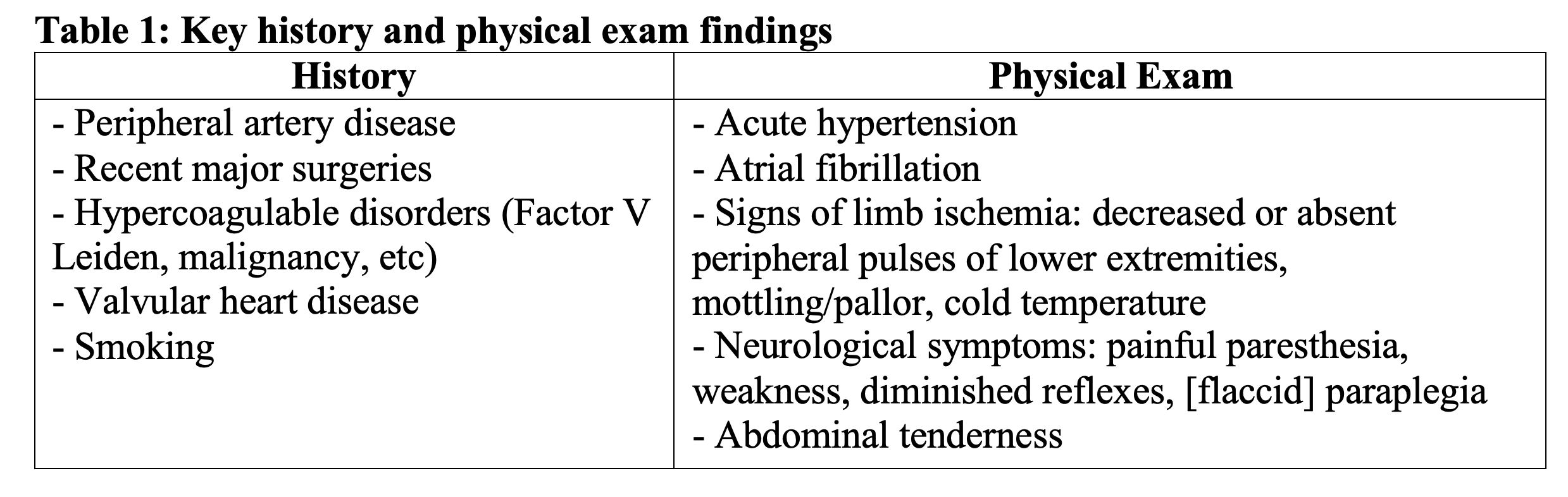
A thorough history and physical exam are key components to evaluation (Table 1). Differential diagnoses might include spinal cord compression/infarction, aortic dissection, and/or cerebrovascular accident.
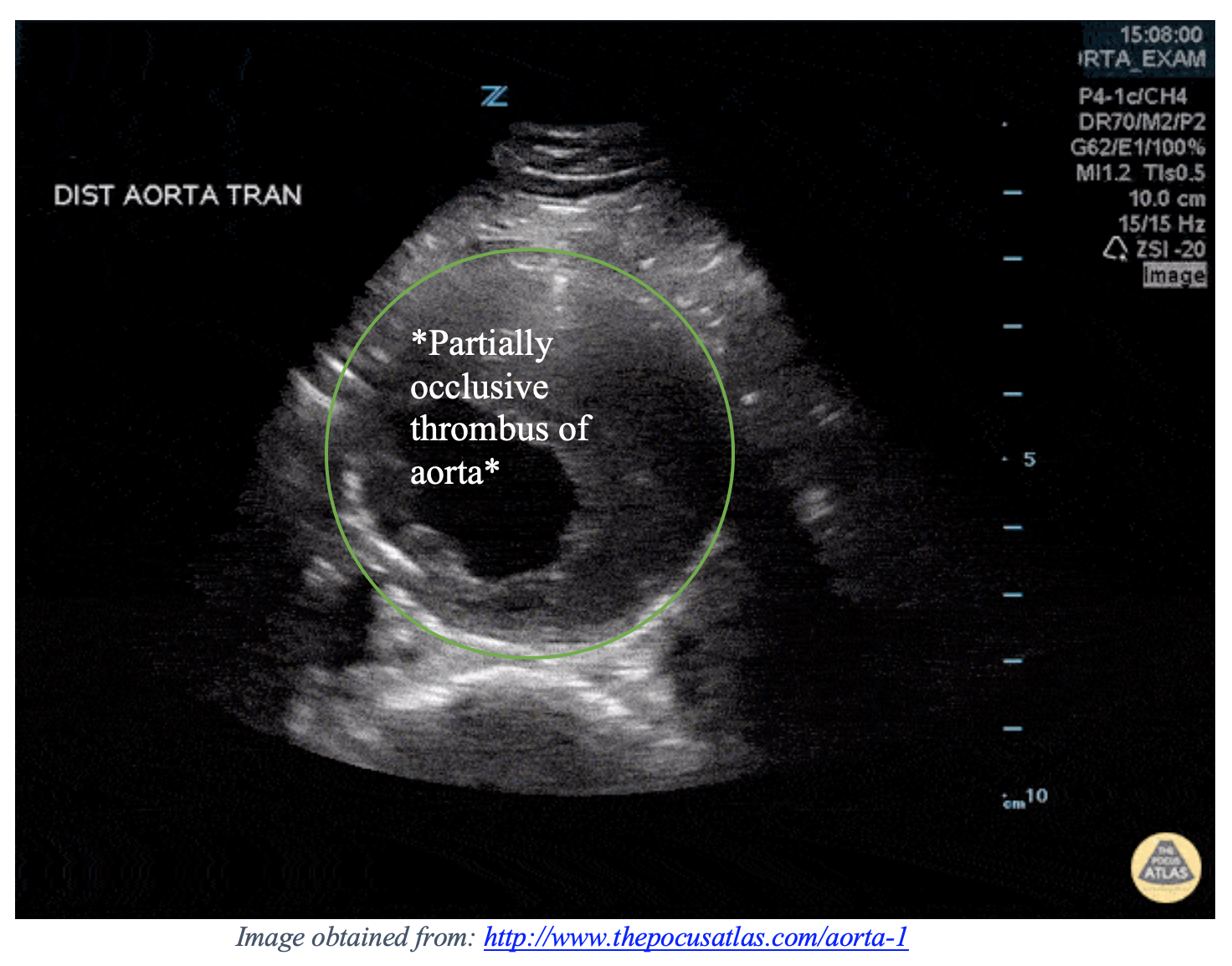
Once this diagnosis is suspected, a quick and non-invasive approach is ultrasonography of the aorta, iliac, and common femoral arteries, which can be completed at the bedside. The curvilinear probe may be used. Remember, pressure may be needed to move bowel gas, and use the spine as your landmark for locating the aorta. Search for the presence of echogenic material within the lumen of the aorta. There should be no color flow within the echogenic material. To fully assess the extent of the disease, use color flow to help determine the patency of the lumen, and be sure to scan the entire length of the aorta. It is also helpful to measure the width of the aorta, as there may be concomitant aneurysm (normal aorta < 3cm).
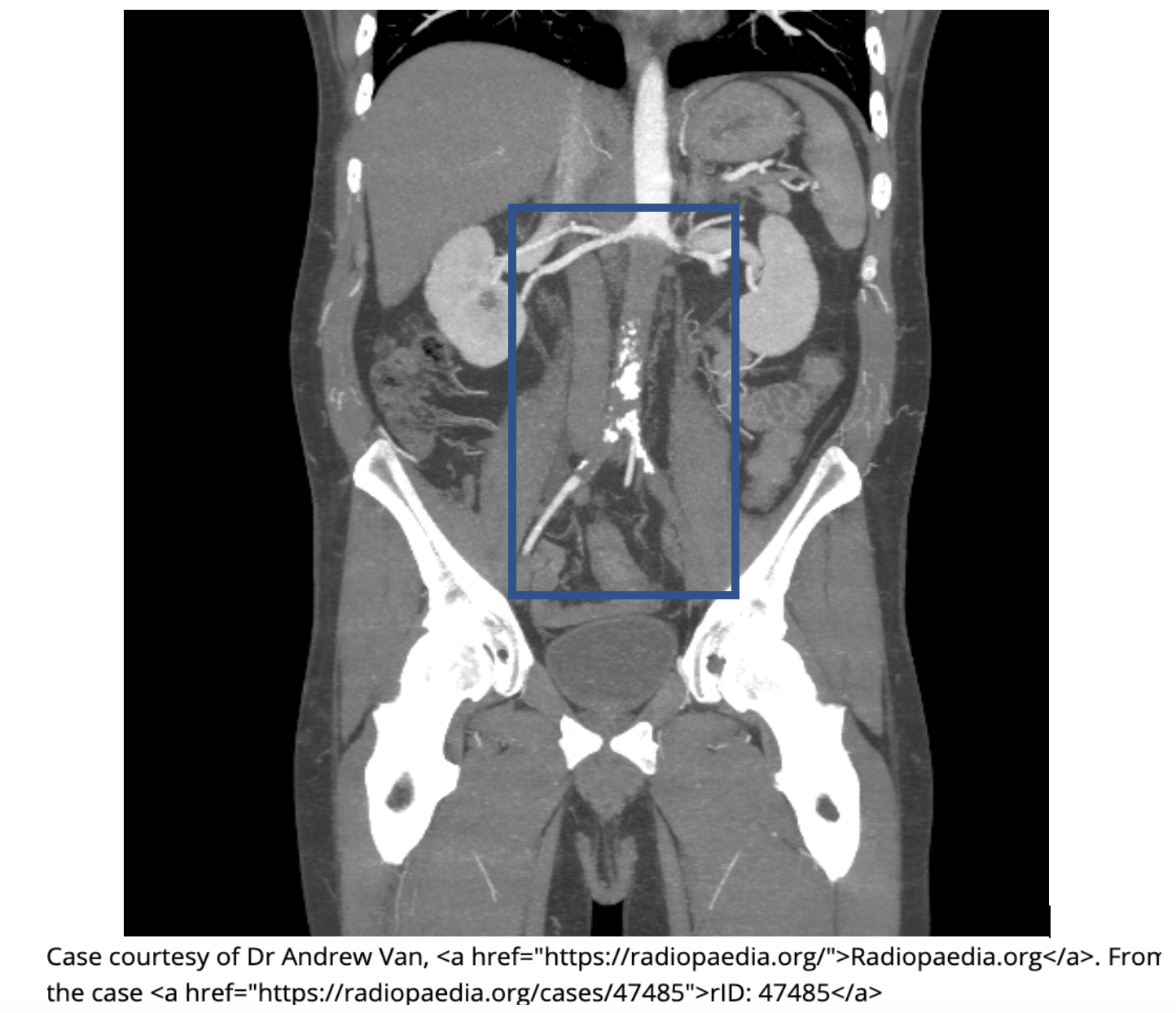
Quality and interpretation of images is operator dependent, affecting accuracy. Thus, CT Angiography (via MSCT) is the test of choice due to the ease of obtaining imaging and proximity to the ED.2,5 Once again you are looking for thrombotic masses within the lumen of the aorta that do not enhance with contrast administration. These may partially or completely occlude the lumen. Even with complete occlusions, you may still note reconstructed blood flow below the level of the thrombosis due to collateral circulation. These images are able to provide a great deal of information regarding location of thrombus/embolism, anatomical anomalies, and can help to differentiate between other possible etiologies pertaining to an acute abdomen.
Management
Management includes supportive care such as hydration with IV fluids and pain control, but it is imperative to consult vascular surgery. In very select cases, such as those without significant motor deficits and with occlusion limited to the distal abdominal aorta, treatment solely with thrombolytic therapy may be considered.1 However, most cases will require thromboembolectomy and consideration of revascularization with aortoiliac or aortofemoral reconstructions versus bypass.1-6 If vascular surgery is not available at your facility, expedient transfer is required. These patients should be heparinized (bolus 10,000 units)3 to avoid propagation of clot. If vascular surgery is present at your facility and the patient is to go directly to the OR, then heparin may be withheld on a case-by-case basis after discussion with vascular surgery.5 About half of patients will be continued on anticoagulation medications at discharge (LMWH or warfarin) or on aspirin or clopidogrel.1
Outcomes
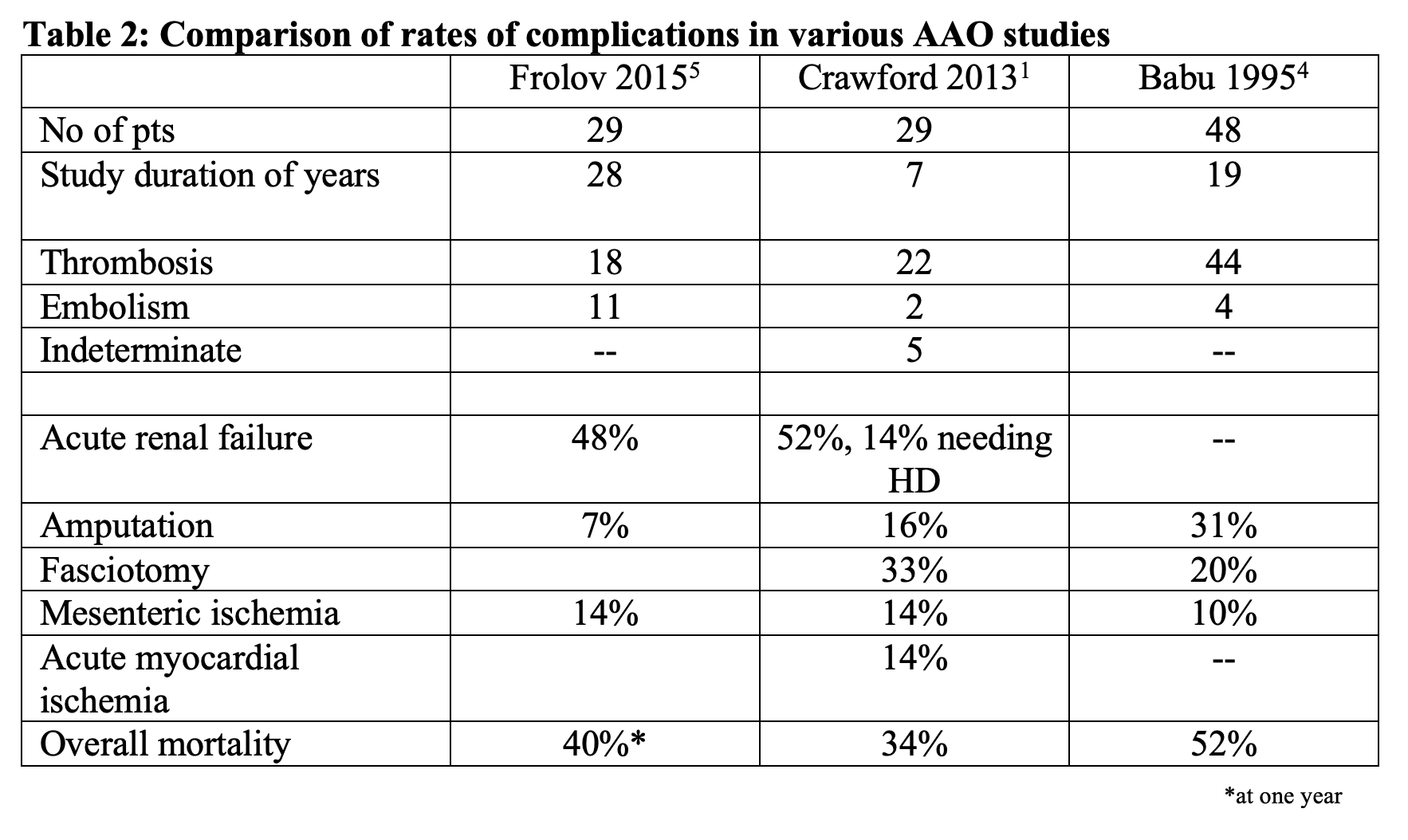
Notably, despite advances in care, overall mortality still tends to be high (between 21-52%),1,2 thus these patients will require admission to an ICU for close monitoring. Morbidity rates also tend to be high between 60-75% (see Table 2).2
Case Conclusion
You were able to recognize the signs and symptoms of an AAO promptly and obtain a CTA which confirms diagnosis of an infrarenal embolus. While awaiting for a call back from the vascular surgeon, you initiate IVF, analgesics, and control her heart rate with diltiazem. You also remember to bolus 10,000U of heparin. The vascular surgeon calls back and plans to take the patient to the OR. The patient has a complicated postoperative course that involves an ICU stay and need for dialysis, but is able to be discharged with full recovery in 30 days on anti-coagulation therapy.
Pearls
- A high index of suspicion should be maintained for sudden onset of bilateral lower extremity paresthesias/pain/weakness in combination with signs of diminished flow (mottling, decreased peripheral pulses, etc).
- CT is imaging modality of choice, but US is a rapid bedside assessment you can use.
- Definitive treatment lies with consultation in vascular surgery for OR. Consider anticoagulation to prevent propagation of clot.
References
- Crawford, JD. et al. A modern series of acute aortic occlusion. Journal of Vascular Surgery. 2014;59(4): 1044-1050.
- Dominković, M., et al. Acute Aortic Occlusion. Medicina Fluminensis. 2012:49(1):92-97.
- Littooy, Fred N., et al. Acute aortic occlusion—A multifaceted catastrophe. Journal of Vascular Surgery. 1986;4(3):211-216.
- Babu, Sateesh C., et al. Acute aortic occlusion – Factors that influence outcome. Journal of Vascular Surgery. 1995;21(4):567-575.
- De Varona Frolov, SR, et. al. Outcomes after treatment of Acute Aortic Occlusion. Cir Esp. 2015;93:573–579.
- Duvuru, R., et. al. Surgical management of acute aortic occlusion: A single-center experience. Indian Journal of Vascular and Endovascular surgery. 2018;5(1):26-28.
- TPA. (2019). Aorta — TPA. [online] Available at: http://www.thepocusatlas.com/aorta-1 [Accessed 12 Sep. 2019].
- Chaitali Shah and Pamela T Johnson. “SonoWorld.com.” Sonography & Ultrasound Resources,sonoworld.com/CaseDetails/Mural_thrombus_in_the_aorta.aspx?CaseId=70.








