Author: Lloyd Tannenbaum, MD (Emergency Medicine Resident, San Antonio, TX) // Edited by: Jamie Santistevan, MD (@jamie_rae_EMdoc – EM Physician, Presbyterian Hospital, Albuquerque, NM); Manpreet Singh, MD (@MPrizzleER – Assistant Professor of Emergency Medicine / Department of Emergency Medicine – Harbor-UCLA Medical Center); and Brit Long, MD (@long_brit – EM Attending Physician, San Antonio, TX)
Welcome to this edition of ECG Pointers, an emDOCs series designed to give you high yield tips about ECGs to keep your interpretation skills sharp. For a deeper dive on ECGs, we will include links to other great ECG FOAMed!
Ventricular tachycardia (VT) is a crucial diagnosis to not miss. Especially for an ER physician. If the patient is crashing, a wide complex tachycardia gets treated like VT and the patient gets a healthy dose of electricity. Those cases are easy. What about cases where there is more time to consider other possibilities? What if you have a stable patient with a wide complex tachycardia? This week’s edition of EKG pointers will explore how to manage wide complex tachycardias and how to differentiate VT from other mimics.
The Case:
You are called over to the bedside of a 54 year old male with a history significant for hypertension, diabetes, hyperlipidemia, smoking and obesity. The nurse is concerned because he just performed an EKG on this patient and it looks like this:
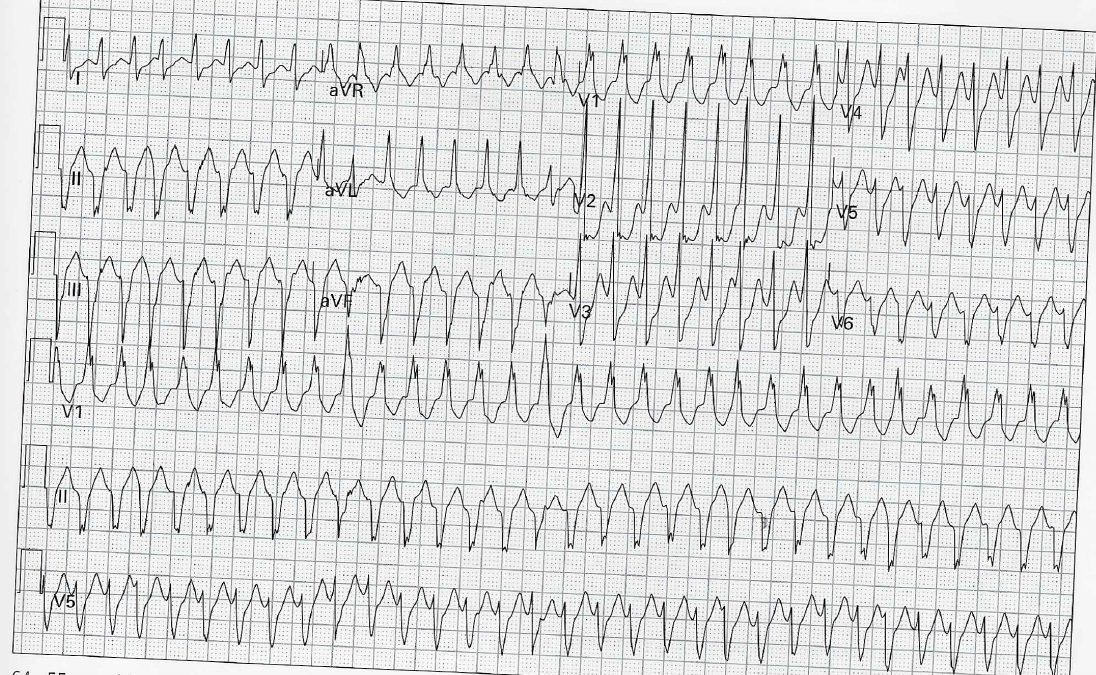
EKG from Amal Mattu and William Brady’s EKGs For The Emergency Physician 2[1].
The patient has a stable blood pressure and is complaining of ankle pain. Besides wondering why an EKG was performed on this patient, what do you want to do?
Let’s start with the basics. The American College of Cardiologists, the American Heart Association, and the European Society of Cardiologists have developed the following algorithm as a way to approach wide complex tachycardias[2]:
Why are we in such a hurry to diagnose VT? Well, the heart can only sustain VT for so long, eventually it will degrade into ventricular fibrillation. There are two major types of VT, monomorphic and polymorphic. As the name suggests, in monomorphic VT, the complexes all look approximately the same where as in polymorphic VT, the complex are constantly changing. A good example of polymorphic VT is Torsades De Pointes, which you can review here: http://www.emdocs.net/ecg-pointers-is-it-torsade-de-pointes/. The remainder of this post will focus on monomorphic VT.
There are several diagnostic clues that we can see in the EKG that point us to towards VT. The first two are universal; they are seen in every case of VT:
- The first is in the name: tachycardia. These patients must have a heart rate over 100 beats per minutes
- The second is that the EKG must have a WIDE QRS, i.e. the QRS is >120 msec.
(BONUS FOAM: Dr. Amal Mattu does an excellent lecture on, really wide complex tachycardias: https://www.youtube.com/watch?v=UXh8PS9dtmo)
What else will we see on an EKG that points us to VT [3]?
-Capture beats – Capture beats occur when the SA node “captures” the ventricles and a “normal sinus beat” appears to be in the middle of a run of VT.
-Fusion beats – Fusion beats occur when a ventricular beat and a sinus beat fire at the same time and on the EKG you see a combination of the two.
-AV dissociation – The P waves will be randomly dispersed throughout the rhythm. Some will be before the QRS, some will be after and some will be contained within the QRS complex. It is also not uncommon to be unable to identify p waves at all.
-Josephson’s sign – This occurs when there is notching during the nadir of the S-wave.
-Brugada’s sign – This sign occurs when the distance of the onset of the QRS complex to the nadir of the S wave is >100 msec.
-If there is an RSR’, the LEFT “bunny” ear is typically taller than the right in cases of VT, which is the opposite of what is expected in a Right Bundle Branch Block where the RIGHT ear is typically taller.
Let’s look at our EKG and see if any of these signs are present:
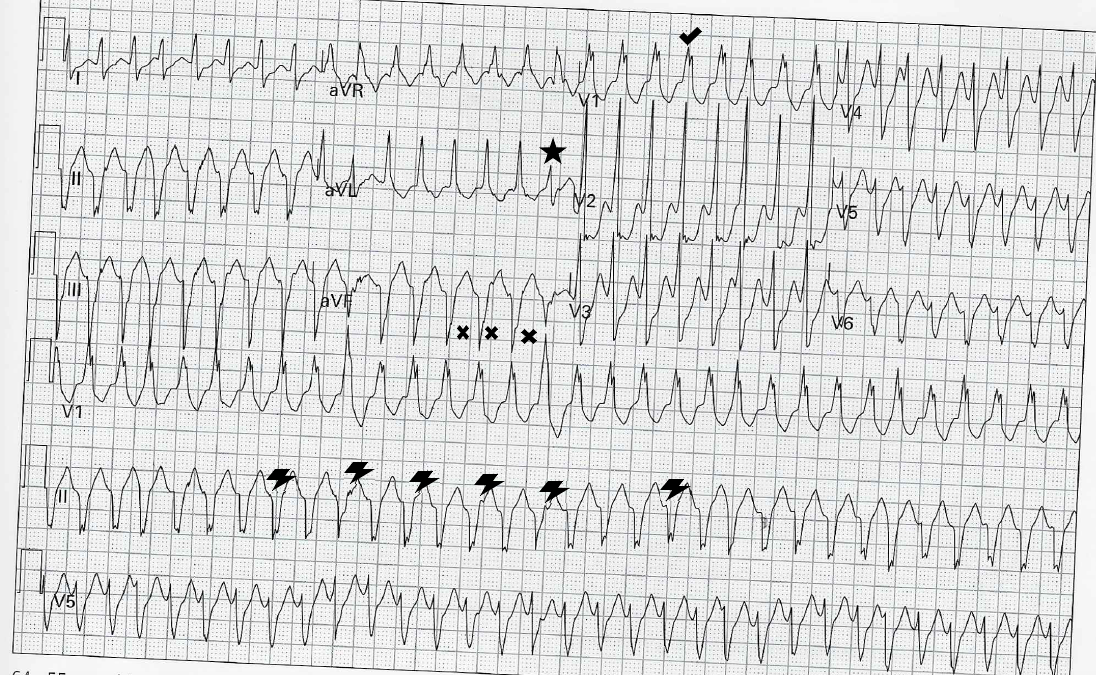
This EKG has been marked to show some of the above signs that lean towards VT. The star marks a fusion beat (a supraventricular beat coincides with a ventricular beat to produce a narrower complex). The check mark shows the taller left “bunny” ear is taller than the right. The “X” shows S-wave notching. The lightning bolts mark the location of interspersed P-waves, representing AV dissociation.
Why are we stressing so much about properly diagnosing VT? Well, if the patient presents with a rhythm that is thought to be SVT with aberrancy but is actually VT, that patient may get treated with AV nodal blocking agents. If you treat VT with AV nodal blocking agents, the patient’s rhythm will quickly degrade into ventricular fibrillation. The Brugada algorithm is often used to differentiate VT from SVT with aberrancy, based on 4 sequential questions [4][5]. If any answer along the algorithm is yes, then VT is the diagnosis. However, keep in mind that validations of the Brugada algorithm have demonstrated sensitivities approximating 80% [6].
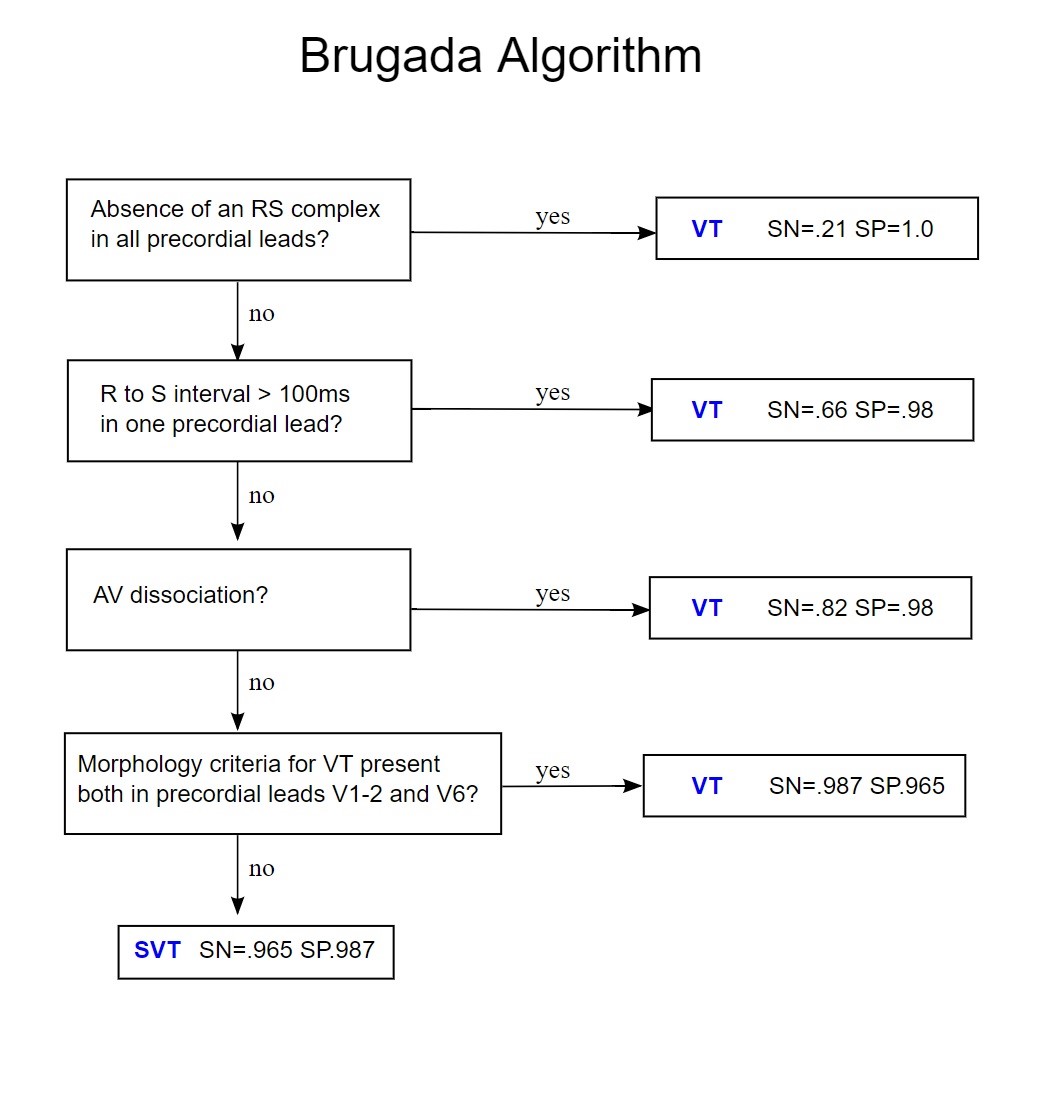
Compliments of CardioNetwork’s ECGPedia [4].
Life in the Fast Lane and Healio have both done fantastic write ups of the Brugada algorithm and walk you through each step with EKG examples to help better explain the algorithm. See them below:
MDCalc also has the criteria set up as “Yes” or “No” questions that you can go through: https://www.mdcalc.com/brugada-criteria-ventricular-tachycardia
That was pretty complex, right? Well in 2010, Brugada et al published a paper [4,5] in the Journal Heart Rhythm that found high sensitivity in diagnosing VT based on the R-Wave Peak Time (RWPT) in lead II being greater than 50 msec. To calculate the RWPT, measure the start of the QRS complex to the peak of the R-wave. If that distance is longer than 50 msec, it is very likely that the rhythm is VT. That’s much simpler.
Case Conclusion:
After further discussion with the patient, it turned out that he passed out and when he woke up, his ankle hurt. He was found to be in ventricular tachycardia, stabilized with amiodarone, and admitted by cardiology for further work up.
Resources/Further Reading:
- Mattu, Amal and Brady William. ECGs for the Emergency Physician 2. Malden: Blackwell Publishing. 2008. Print.
- Blomström-Lundqvist C, Scheinman MM, Aliot EM, Alpert JS, Calkins H, Camm AJ, Campbell WB, Haines DE, Kuck KH, Lerman BB, Miller DD, Shaeffer CW, Stevenson WG, Tomaselli GF, Antman EM, Smith SC Jr, Alpert JS, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Hiratzka LF, Hunt SA, Jacobs AK, Russell RO Jr, Priori SG, Blanc JJ, Budaj A, Burgos EF, Cowie M, Deckers JW, Garcia MA, Klein WW, Lekakis J, Lindahl B, Mazzotta G, Morais JC, Oto A, Smiseth O, Trappe HJ, and European Society of Cardiology Committee, NASPE-Heart Rhythm Society. ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias–executive summary. a report of the American college of cardiology/American heart association task force on practice guidelines and the European society of cardiology committee for practice guidelines (writing committee to develop guidelines for the management of patients with supraventricular arrhythmias) developed in collaboration with NASPE-Heart Rhythm Society. J Am Coll Cardiol. 2003 Oct 15;42(8):1493-531. PubMed ID:14563598
- Burns, Edward. 19 March 2017. Ventricular Tachycardia -Monomorphic. https://lifeinthefastlane.com/ecg-library/ventricular-tachycardia/.
- de Jong, Jonas. 24 February 2013. Approach to the Wide Complex Tachycardia. https://en.ecgpedia.org/wiki/Approach_to_the_Wide_Complex_Tachycardia#bibkey_Brugada2.
- Pava LF, Perafán P, Badiel M, Arango JJ, Mont L, Morillo CA, and Brugada J. R-wave peak time at DII: a new criterion for differentiating between wide complex QRS tachycardias. Heart Rhythm. 2010 Jul;7(7):922-6. DOI:10.1016/j.hrthm.2010.03.001 | PubMed ID:20215043
- Isenhour JL, Craig S, Gibbs M, et al. Wide complex tachycardia: Continued evaluation of diagnostic criteria. Academic EM. 2000;7(7):769-773.








