Authors: Brannon Inman (EM Resident, San Antonio, TX) and Lloyd Tannenbaum (EM Attending Physician, San Antonio, TX) // Reviewed by: Jamie Santistevan, MD (@jamie_rae_EMdoc, EM Physician, Presbyterian Hospital, Albuquerque, NM); Manpreet Singh, MD (@MPrizzleER); and Brit Long, MD (@long_brit)
Welcome to this edition of ECG Pointers, an emDOCs series designed to give you high yield tips about ECGs to keep your interpretation skills sharp. For a deeper dive on ECGs, we will include links to other great ECG FOAMed!
The Case:
A 54-year-old woman is brought to the emergency department for palpitations. In triage she has a heart rate of 120 bpm, BP 143/89, SpO2 99%. Shortly after being roomed, she begins to complain of worsening symptoms and looks pale. Repeat vitals are obtained, and she is placed on the monitor. Repeat blood pressure is 100/88, the monitor reads a heart rate of 236. An ECG is obtained and shows rapid atrial flutter with 1:1 conduction (Figure 1).

While establishing the safety net (IV x2, placing the defibrillation pads on her, and bringing the crash cart to the bedside) her heart rate spontaneously slows. She looks less pale, and repeat blood pressure is 137/95. You look at the monitor and now see Atrial Fibrillation with a ventricular rate in the 140s (Figure 2).
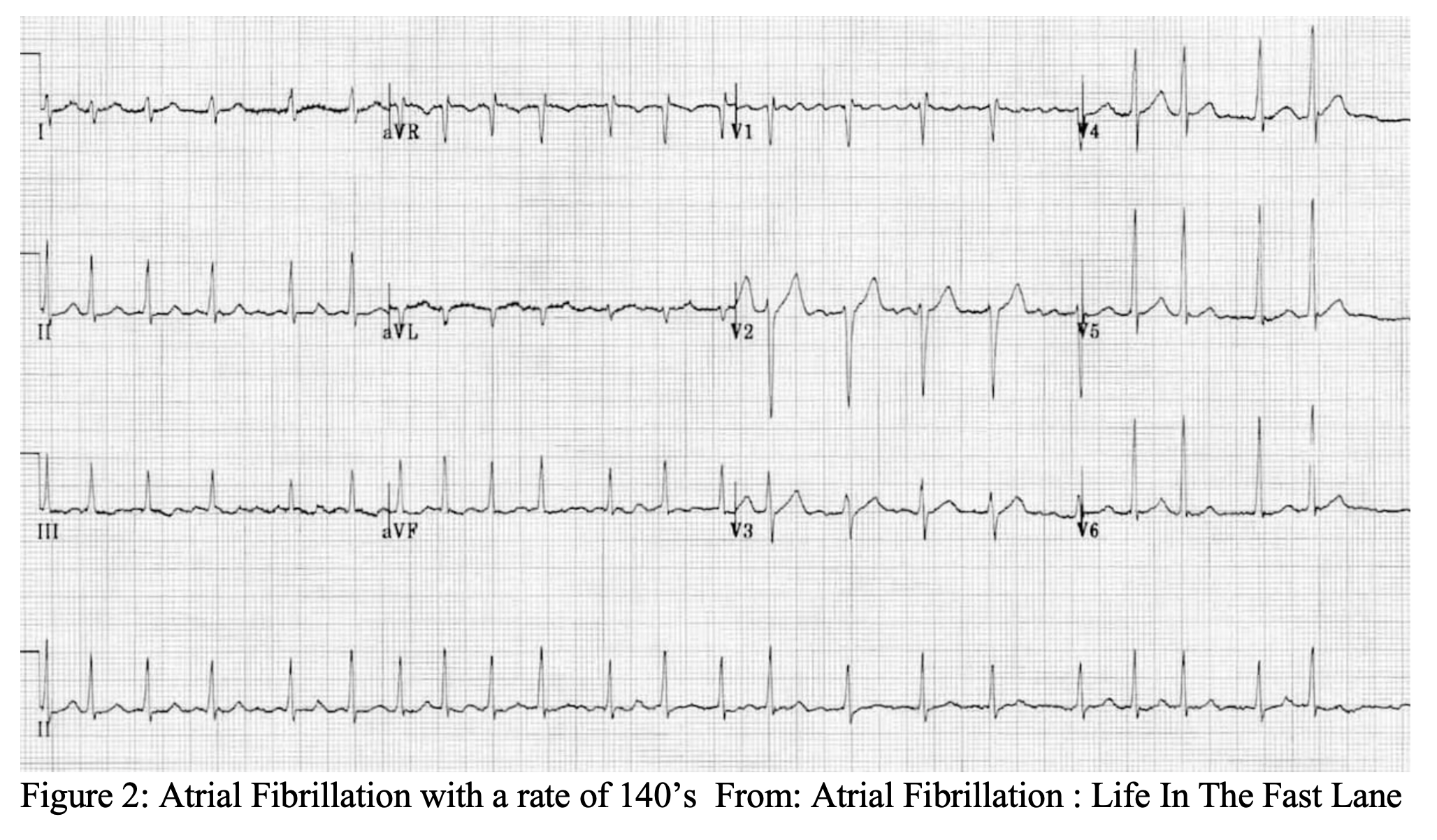
This is rather bizarre. She appears to have spontaneously jumped into 1:1 atrial flutter and then converted to atrial fibrillation. While the patient is stable you ask about medical history, which is only significant for Atrial Fibrillation. She takes flecainide for rhythm control that she started about 1 month ago. She is also on metoprolol.
Flecainide refresher:
Flecainide is a class 1C sodium channel blocker.1 Flecainide blocks fast inward sodium channels during phase 0 depolarization and unbinds slowly during diastole. Thus, flecainide prolongs the refractory period of the heart and displays a rate dependent effect. Via this effect the medication shortens action potential duration though the His-Purkinje system. The medication also inhibits opening of delayed rectifier potassium channels and ryanodine calcium channels effectively increasing action potentials in ventricular myocardium and reducing depolarization of myocardium, respectively.1–3
Flecainide is indicated for atrial fibrillation, atrial flutter, premature ventricular contractions, and prevention of ventricular arrhythmias. It also can be given for sustained fetal tachycardia off label.2
Back to the Case:
On further history our patient mentions that she self-discontinued her metoprolol about a month ago. As it turns out, flecainide is well known to cause patients to spontaneously convert into 1:1 atrial flutter.3 It is for this reason that experts recommend patients taking flecainide also be on an AV nodal blocking agent such as metoprolol or diltiazem.2 Currently, the patient is still in rapid atrial fibrillation. With this new knowledge in hand, you reach for your favorite AV nodal blocker and start her on a diltiazem drip. You discuss the case with the patient’s cardiologist, who recommends continuing the diltiazem drip and admitting her to the cardiac ICU. There she is anticoagulated, cardioverted, then undergoes an ablation in the electrophysiology lab and is discharged on no medications.
Toxicology Corner:
…Two weeks later
The patient presents with her husband who is altered. She believes that he took the remainder of her flecainide in a suicide attempt. His past medical history is significant for ADHD, for which he takes an amphetamine salt derivative. She is unsure how much, if any of this, he may have taken. You recall that amphetamines and sympathomimetics cause ß-adrenergic receptor stimulation increasing the toxicity of flecainide and may lead to a more complicated clinical course with high illness severity.4 He appears toxic, with dusky skin poor perfusion. Vitals show a pulse of 104bpm with a blood pressure of 78/41. The following ECG is obtained.
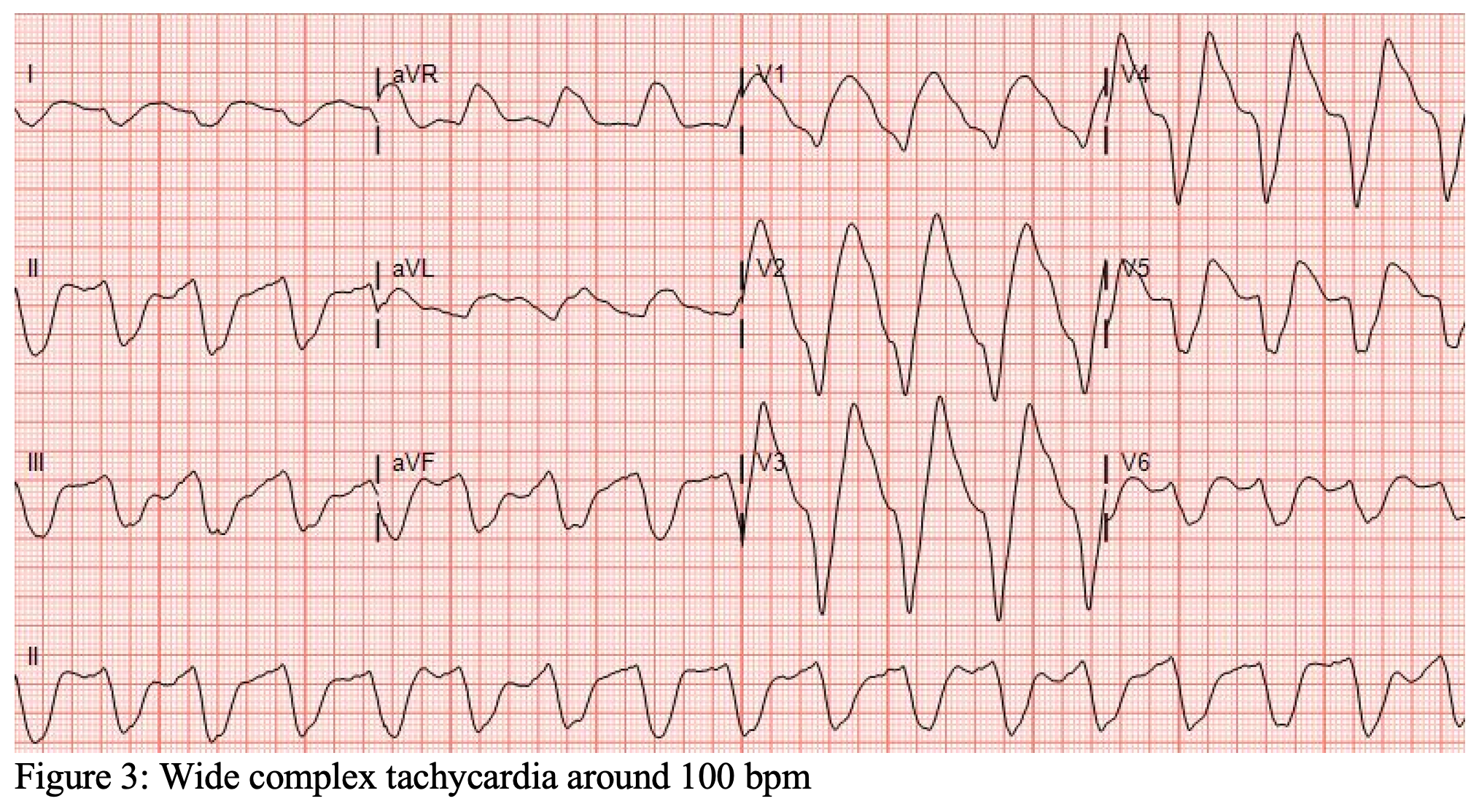
You recognize this as a wide complex tachycardia with a QRS interval of about 240ms. While you are establishing IV access and brining the crash cart over the patient goes into cardiac arrest. You call for backup and start the code. Your nurse informs you that he still does not have IV access. But he has two tibias … break out the drill. An IO is placed for the code, and you run through the ACLS algorithm. You also give additional amps of sodium bicarb, given the suspected ingestion. Four minutes into the arrest you regain a pulse. IV access is obtained, and you quickly add 3 amps of bicarb to a liter of D5W for a quick and dirty bicarb drip. Start at 2-3cc/min and titrate to a blood pH of 7.5 or place a foley and titrate to a urine pH of 8. A post-ROSC ECG is obtained (Figure 4).

Treatment of flecainide toxicity:
Sodium bicarbonate:
It’s not entirely clear why bicarb works for sodium channel blocker drug overdoses. However, research in canines has suggested that the load of sodium likely leads to competitive inhibition and an electrostatic repulsive effect of flecainide from its binding site. Secondly the increased serum pH may facilitate flecainide unbinding from its binding site.4
Dialysis:
Unlikely to be effective given flecainide’s large molecular size, protein binding and high volume of distribution.5 One study has showed less than 1% of orally administered flecainide is removed with hemodialysis.6
Intralipid:
In addition to bicarb, your tox center may recommend IV lipid emulsion therapy (LE). Case reports have demonstrated benefit of LE in flecainide toxicity.7 As with bicarb, the exact mechanism of this antidote is unknown, however, four theories predominate.
First is the Lipid sink theory: The addition of LE into the affected patient forms lipid particles in the blood stream allowing a physiologically inert place for lipophilic drugs to sequester. 8
Second is increased ionotropy and cardiac fatty acid metabolism. LE may increase inotropy of cardiac myocytes, at least in nontoxic conditions. Additionally, myocytes have a preference for metabolism of fatty acids. Work on animals has shown that carnitine and the carnitine palmitoyl transferase 1 enzyme is required for transport into myocytes. Likely suggesting the improved inotropy is at least partially dependent on fatty acid availability for metabolism.8
Third, addition of LE may improve the recovery of inhibited sodium channels independent of the toxin in the presence of LE.8
Fourth, cardioprotection from cell damage. In mice with induced myocardial ischemia reperfusion leads to release of free radicals and cardiac injury. The addition of LE has been shown to decrease reperfusion injury, thought to be secondary to LE’s inhibition of the mitochondrial permeability transition pore (mPTP), which has been shown to post cardiac stress excitotoxicity and apoptosis.8
Despite maximal therapy the patient continues to be unstable. The half-life of flecainide is 20 hours.2 Buckle up. This guy is going to be sick for a while. Luckily for you, your program has a rapidly expanding and well-funded ECMO program.
ECMO:
In terms of pure hemodynamic support, flecainide is largely cardiotoxic. Initiating veno-arterial ECMO can support these patients through their toxidrome. Additionally, the polyvinyl-chloride (PVC) tubing used in ECMO, and the ECMO circuit, increases volume of distribution of drugs and likely slowly sequesters lipophilic drugs (such of flecainide) over time.9–12
Case Conclusion:
After 2 days on ECMO the patient recovers. He is decannulated from ECMO and monitored in the ICU before being downgraded to the psychiatry floor for his ingestion.
Main ECG Pointers:
- Flecainide is a sodium channel blocker, Class 1C used most commonly for rhythm control in a fib/flutter.
- Flecainide is well known to convert patients to 1:1 Atrial Flutter. It is for this reason patients should also take an AV nodal blocker (metoprolol, diltiazem, etc)
- In flecainide toxicity consider sodium bicarbonate and lipid emulsion.
- The toxidrome of flecainide is worsened by co-ingestion of stimulants.
- For severely ill patients with a flecainide ingestion consider ECMO.
References/Further Reading:
- Flecainide | C17H20F6N2O3 – PubChem. Accessed April 5, 2021. https://pubchem.ncbi.nlm.nih.gov/compound/3356
- Flecainide: Drug information – UpToDate. Accessed April 5, 2021. https://www.uptodate.com/contents/flecainide-drug-information?search=flecainide&source=panel_search_result&selectedTitle=1~100&usage_type=panel&kp_tab=drug_general&display_rank=1#F171556
- Andrikopoulos GK. Flecainide: Current status and perspectives in arrhythmia management. World Journal of Cardiology. 2015;7(2):76. doi:10.4330/wjc.v7.i2.76
- Vu NM, Hill TE, Summers MR, Vranian MN, Faulx MD. Management of life-threatening flecainide overdose: A case report and review of the literature. HeartRhythm Case Reports. 2016;2(3):228-231. doi:10.1016/j.hrcr.2015.12.013
- Conard GJ, Ober RE. Metabolism of flecainide. The American Journal of Cardiology. 1984;53(5). doi:10.1016/0002-9149(84)90501-0
- Forland SC, Burgess E, Blair AD, et al. Oral Flecainide Pharmacokinetics in Patients with Impaired Renal Function. The Journal of Clinical Pharmacology. 1988;28(3):259-267. doi:10.1002/j.1552-4604.1988.tb03142.x
- de Schryver N, Hantson P, Haufroid V, Dechamps M. Cardiogenic Shock in a Hemodialyzed Patient on Flecainide: Treatment with Intravenous Fat Emulsion, Extracorporeal Cardiac Life Support, and CytoSorb® Hemoadsorption. Case Reports in Cardiology. 2019;2019:1-5. doi:10.1155/2019/1905871
- Walter E, McKinlay J, Corbett J, Kirk-Bayley J. Review of management in cardiotoxic overdose and efficacy of delayed intralipid use. Journal of the Intensive Care Society. 2018;19(1):50-55. doi:10.1177/1751143717705802
- Preston TJ, Hodge AB, Riley JB, Leib-Sargel C, Nicol KK. In vitro drug adsorption and plasma free hemoglobin levels associated with hollow fiber oxygenators in the extracorporeal life support (ECLS) circuit. Journal of Extra-Corporeal Technology. 2007;39(4):234-237. Accessed April 18, 2021. /pmc/articles/PMC4680688/
- Preston TJ, Ratliff TM, Gomez D, et al. Modified surface coatings and their effect on drug adsorption within the extracorporeal life support circuit. Journal of Extra-Corporeal Technology. 2010;42(3):199-202. Accessed April 18, 2021. /pmc/articles/PMC4679959/
- Shekar K, Fraser JF, Smith MT, Roberts JA. Pharmacokinetic changes in patients receiving extracorporeal membrane oxygenation. Journal of Critical Care. 2012;27(6):741.e9-741.e18. doi:10.1016/j.jcrc.2012.02.013
- Dzierba AL, Abrams D, Brodie D. Medicating patients during extracorporeal membrane oxygenation: The evidence is building. Critical Care. 2017;21(1). doi:10.1186/s13054-017-1644-y








