Originally published at EM Cases – Visit to listen to accompanying podcast. Reposted with permission.
Follow Dr. Anton Helman on twitter @EMCases
In the U.S. over the last 15 years there has been a faster increase in emergency radiology imaging utilization than any other physician service including major procedures and lab tests. In Canada, we run up an annual radiology bill of more than 2.2 billion dollars. This escalation in imaging is likely due to a variety of factors including availability of technology, inappropriate imaging referrals, increasing patient expectations, overuse of follow-up imaging, vague reports, incidental findings, increasingly busy practices and a paucity of resources and guidelines in emergency radiology.
Some of the recommendations from a recent Canadian Choosing Wisely Campaign for emergency radiology go like this: Avoid imaging for low back pain, minor head trauma or uncomplicated headache unless red flags are present. Don’t start with CT for children suspected of appendicitis. Don’t order CT head routinely in the workup of syncope with a normal neurologic clinical exam. These are all very practical reminders.
But still we can do better. In a recent Canadian study, a whopping one in seven ED patients received a CT scan, and physician knowledge about the quantitative risks associated with CT radiation dosing was limited. There is a huge variation in utilization of CT among ED physicians. In one study, ‘low users’ ordered an average of 78 CT scans per 1,000 patient visits, as compared to the ‘high users’ who ordered 135 CT scans per 1,000 patient visits. We can minimize potentially harmful imaging while at the same time improve our diagnostic accuracy by gaining more knowledge about the specific indications of various imaging modalities in common clinical scenarios, thinking carefully about how the likelihood ratios change from pre to post imaging, understanding the limitations of different imaging modalities, predicting the radiation effects, and knowing when we really need to push for advanced imaging like MRI.
So, with the help of ‘the walking encyclopedia of EM’ Dr. Walter Himmel and North York General’s Deputy Chief of Radiology Dr. Ryan Margau, we’ll discuss a few emergency radiology controversies, pearls and pitfalls: Which patients with chest pain suspected of ACS require a CXR? What CXR findings do ED docs tend to miss? How should we workup solitary pulmonary nodules found on CXR or CT? Is the abdominal x-ray dead or are there still indications for it’s use? Which x-ray views are preferred for detecting pneumoperitoneum? When should we consider ultrasound as a screening test instead of, or before, CT? What are the true indications for contrast in abdominal and head CT? How should we manage the patient who has had a previous CT contrast reaction or “allergy” who really needs a CT with contrast? What is the truth about CT radiation for shared decision making? And many more emergency radiology controversies…
Podcast interview recorded October, 2015, commentary recorded June 2016
Written summary and blog post written by Anton Helman, June 2016
Which patients with chest pain suspected of ACS require a CXR?
Observational studies show that >70% of patients who present with chest pain who are suspected of ACS receive a CXR. Many of these CXRs may not be necessary.
The Canadian ACS Guidelines suggest that patients can forgo CXR if they have:
- No history of CHF
- No history of smoking
- No abnormalities on auscultation
However the study that this was based on could not be validated in subsequent studies.
Another study suggests that it is reasonable to consider forgoing routine chest radiography in adult patients with nontraumatic chest pain that do not demonstrate any of the variables of the modified Rothrock criteria. Note that this study had showed a very low specificity for a significant finding on CXR.
- age over 65
- history of alcohol use
- history of CHF
- fever
- hypoxia
- tachypnea
- decreased breath sounds
Dr. Himmel’s take home message: CXRs should not be routine for patients who present to the ED with chest pain – use your clinical judgement.
Emergency Radiology CXR findings that ED docs tend to miss
There are two areas to scrutinize carefully for every CXR, as these areas overlap with other structures making them difficult to decipher, are:
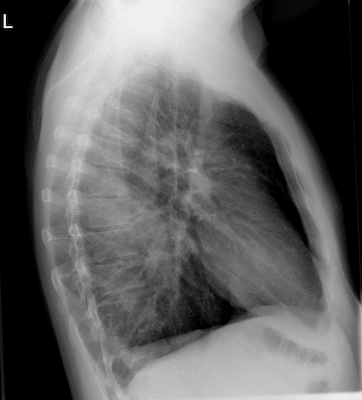
1. Lung apices overlap with the clavicle, so look for any asymmetry between lung apices specifically looking for small pneumothorax, apical/Pancoast tumour or cavitary lung disease such as TB
2. Lung bases overlap with the hemidiaphragms, so carefully scrutinize the lateral view for the normal increasing darkness from the lung apices to the hemidiphragms; if any abnormality is detected then confirm by looking for symmetry on the AP view

Pancoust Tumour in the left lung apex. Lesions in the lung apicies tend to be missed as there is overlap with the clavicle.
Workup for Solitary pulmonary nodule found on CXR or CT
Background: About 5-7% of pulmonary nodules turn out to be cancer and the bigger the nodule the higher the risk of cancer. Pulmonary nodules are very common in smokers – about 50% of smokers over the age of 50 have at least one nodule.
Which nodules found on CXR are benign? Generally speaking benign nodules are:
- have a smooth border AND
- are shown to be stable over at least 2 years (compared to previous imaging) AND
- are heavily calcified.
For patients without ANY high risk factors (age >35 years, smoking or occupational exposure) and all of the above criteria, these nodules do not require followup.
All other nodules require followup as they have more than a 1% chance of being cancerous.
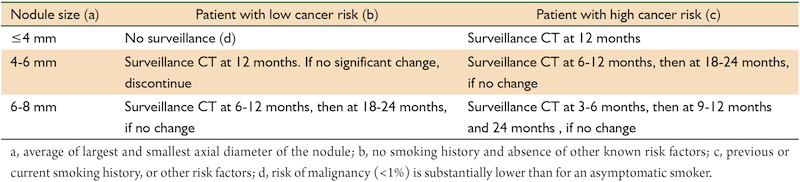
CT is the followup imaging modality of choice, and the updated Fleischner criteria dictate when nodules found on CT need further follow-up according to size, risk factors and whether the nodule is solid, subsolid or ground-glass.
Fleischner Criteria for Solitary Pulmonary Nodules found on CT
Emergency Radiology Question: Is the abdominal x-ray dead?
ED abdominal x-rays, in one observational study, lead to a change in management only 4% of the time. Nonetheless there still remains several indications for the use of abdominal x-rays in emergency radiology.
Indications for ED abdominal x-ray
1. Radio-opaque foreign body – metal, leaded glass or large objects such as packets found in drug mules
2. To look for free air in suspect perforated viscous in patient who is not stable enough to leave the ED for a CT
3. Known chronic diagnosis with multiple frequent recurrent acute exacerbations such as recurrent small bowel obstruction, especially in patients who have had multiple CT scans in the past (note that the sensitivity of x-rays for bowel obstruction is poor – approx 50-70%, but specificity is 98%)
Emergency Radiology Question: Which x-ray views are preferred for detecting pneumoperitoneum?
An upright CXR is one of the preferred x-ray views for detecting pneumoperitoneum, however this requires the patient to be sitting or standing erect for a few minutes prior to shooting the film to allow the air to rise caudally under the hemidiaphragms.
In a patient too sick or altered to remain erect for a few minutes, a left lateral decubitus abdominal view is preferred.
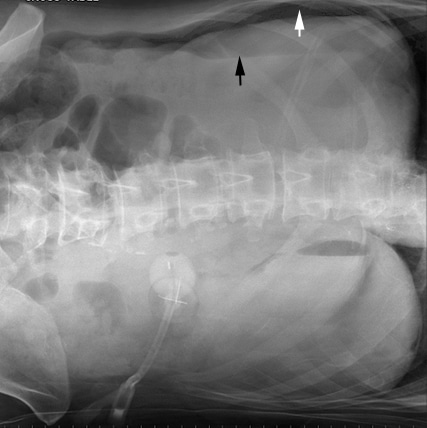
Pneumoperitoneum on left lateral decubitus abdominal x-ray – the preferred x-ray view for patients unable to sit upright
The rule of 3-6-9-12 for bowel obstruction
The small bowel is normally 6cm it is at high risk of rupture.
The large bowel is normally 9cm it is at high risk of rupture.
The cecum is normally 12cm it is at high risk of rupture.
Note that lack of air in the rectum is a late sign of bowel obstruction, so patients who present early in their disease process will often have air in the rectum on x-ray.
Advantages of ultrasound over CT
- Doppler flow allows assessment of blood flow to facilitate diagnosis of ovarian or testicular torsion
- Provides high tissue contrast in biliary tree allowing for improved visualization of gallstones and sludge
- Provides high tissue contrast in solid viscera (liver, kidneys and spleen)
- May visualize abdominal contents better than CT in patients with little adipose tissue
When to consider abdominal ultrasound as a screening test rather than CT
Consider abdominal ultrasound as the initial diagnostic test in suspected uncomplicated appendicitis, nephrolithiasis, or diverticulitis in a young immunocompitant person with a moderate/high pretest probability for the particular diagnosis.
A prospective study in 2009 of more than 1000 hemodynamically stable, non-pregnant adult patients with non-traumatic acute abdominal pain who each received the gamut of emergency radiology tests: plain x-rays, ultrasound and CT, showed that a strategy whereby an ultrasound was done as a screening test (with CT only done if the ultrasound was negative or inconclusive), had a very high sensitivity for diagnoses that required urgent intervention. This strategy reduced CT utilization by 50%.
Indications for IV and/or Oral Contrast in Abdominal CT
There remains a wide variation in practice depending on the local medico-legal environment, the culture of the radiology department, the suspected diagnosis and the preference of the particular radiologist as to whether or not contrast is used for abdominal CT in assessing acute abdominal pain in emergency radiology. The most important variable in determining whether an ED patient receives contrast for their abdominal CT is the radiologist’s preference and skill at reading plain CT vs. contrast CT. Without communication by the ED physician to the radiologist of the most likely diagnosis and the pretest probability of the diagnosis, the default is often contrast CT, which often increases ED length of stay, may cause anaphylactoid reactions and possibly contribute to nephrotoxicity.
The emergency literature shows that the accuracy of plain CT vs. contrast CT for uncomplicated appendicitis, diverticulitis and nephrolithiasis is comparable. However, for patients with undifferentiated abdominal pain, especially elderly patients, contrast CT is more likely to pick up conditions such an unsuspected mesenteric ischemia, portal vien thrombosis and cancer which may be missed on plain CT.
CT with oral contrast makes it easier for the radiologist to assess for bowel obstruction, but on the other hand makes it more difficult for them to assess the bowel wall for ischemia.
Indications for Head CT with Contrast in Emergency Radiology
1. Suspect space occupying lesion such as a brain tumour or abscess on plain CT or on the clinical assessment
Plain CT is neither sensitive nor specific for brain tumours because tumours may be isodense with brain tissue. If a patient with a good clinical picture for a brain tumour has a normal CT, you must go on to a contrast CT. Nonetheless, vasogenic edema seen on plain CT is highly suspicious for a space occupying lesion as apposed to the cytotoxic edema of ischemic stroke. The distinguishing features of vasogenic edema compared to cytotoxic edema are that vasogenic edema spares the gyri vs. cytotoic edema does not, and that cytotoxic edema follows a vascular distribution vs. vasogenic edema does not.
2. Suspect cerebral venous thrombosis
Communication with the radiologist that cerebral venous thrombosis is suspected is paramount because the timing of the images after contrast administration for a CT venogram is longer than for CT angiogram.
3. Suspect carotid or vertebral artery dissection
A CT angiogram of the head and neck are required (as apposed to a CT angiogram of the Circle of Willis used for aneursymal subarachnoid hemorrhage).
4. Distinghishing a traumatic vs. aneurysmal subarachnoid hemorrhage
Occasionally a patient presents to the ED with an altered level of awareness and the history is unclear in terms of whether the patient had a headache and then fell and smashed their head, or whether they just smashed their head. One cannot distinguish traumatic vs aneursysmal subarachnoid hemorrhage based on the distribution of blood on the plain CT alone. It is therefore prudent in patients with an unclear history to follow up the plain CT with a CT angiogram to determine whether an aneurysm is present or not.
Prevention of CT Contrast “Allergy”: An Anaphylactoid Reaction
CT contrast “allergy” is not an IgE mediated phenomenon, and does not cause true anaphylaxis, but rather, it may cause an anaphylactoid type reaction. It is a myth that patients with a history of shellfish or iodine allergy have a higher risk of CT contrast allergy. Nonetheless, patients with multiple allergies in general are more likely to be suffer a CT contrast reaction. Modern contrast has lower osmolality than it used to and is non-ionic, and so the prevalence of CT contrast reaction has dramatically decreased over the years to about 2-3%, with only about 0.1% being serious reactions, and resultant death in less than 1 in 100,000. These are important numbers to take into consideration in shared decision making for the use of contrast CT.
There is no good evidence in the literature to guide hospital protocols for prevention of contrast reactions in patients with a known history of contrast. In particular, premedication with corticosteroids has never been shown to reduce the risk of contrast reactions.
Example Protocol for patients receiving CT contrast in > 12hrs
Prednisone 40mg po + Ranitidine 150mg po 12hrs prior to contrast, repeated 2hrs prior to contrast and Dihphenhydramine 50mg po 1hr prior to contrast
Example Protocol for patients receiving CT contrast in 2 hrs
Hydrocortisone 200mg IV 2hrs prior and Ranitidine 50mg IV + Benadryl 50 IV 1hr prior to contrast
Indications for CT C-spine in Emergency Radiology
While the Canadian C-spine Rules and NEXUS rules are useful in helping decide which patients do not require imaging in emergency radiology, it is less clear which patients who do require imaging should have an x-ray or CT as the their first line imaging modality. Clearly CT is much more accurate than x-ray at detecting significant injuries. This decision needs to take into account 3 factors:
- The patient’s “protoplasm” – Do they have a history of osteoperosis? Are they very elderly? Do they have a history of ankylosing spondylitis?
- The likelihood of obtaining a high quality x-ray image – Is the patient bull-necked? Do they have severe osteoarthritis?
- The mechanism of injury and physical exam – Was it a high risk mechanism of injury such as ejection from a car? Are they altered making the physical exam unreliable? Are there any focal neurological signs?
If you have a moderate-high suspicion for a fracture or dislocation based on the clinical assessment, CT c-spine is the ![]() preferred first line imaging modality. However, for patients in whom you have a very low suspicion for a bony injury, but they fail the NEXUS or Canadian c-spine rules, an x-ray may suffice.
preferred first line imaging modality. However, for patients in whom you have a very low suspicion for a bony injury, but they fail the NEXUS or Canadian c-spine rules, an x-ray may suffice.
The Truth About CT Radiation: A simplified approach to help in shared decision making
- One CXR delivers 0.1mS of radiation which is equivalent to about 10 days of atmospheric radiation in North America
- One head CT delivers the equivalent of about 30-40 CXRs or 8-9 months of atmospheric radiation
- One chest or abdominal CT delivers the equivalent of about 80-100 CXRs or 4 years of atmospheric radiation, which increases the risk of cancer by about 1 in 1000 in a 40 year old patient (up to 1 in 2000 in a younger patient, less in an older patient)
- Approximately 1/3 of people in North America will develop cancer some time in their lives; therefore the risk of cancer after a CT pulmonary angiogram of the chest increases from about 33% to 33.1%, a minuscule difference
- Many centres are employing low dose protocols for CT (eg. CT urogram and CT chest to follow a pulmonary nodule), which minimizes radiation further
- Many centres are employing newer software that minimizes radiation for head CTs
Quote of the Month
“To learn to see – to accustom the eye to calmness, to patience, and to allow things to come up to it; to defer judgment, and to acquire the habit of approaching and grasping an individual case from all sides. This is the first preparatory schooling of intellectuality. One must not respond immediately to a stimulus; one must acquire a command of the obstructing and isolating instincts.”
– Friedrich Nietzsche
Dr. Himmel, Dr. Margau and Dr. Helman have no conflicts of interest to declare.
Key References
Hess EP, Perry JJ, Ladouceur P, Wells GA, Stiell IG. Derivation of a clinical decision rule for chest radiography in emergency department patients with chest pain and possible acute coronary syndrome. CJEM. 2010;12(2):128-34.
Rothrock SG, Green SM, Costanzo KA, Fanelli JM, Cruzen ES, Pagane JR. High yield criteria for obtaining non-trauma chest radiography in the adult emergency department population. J Emerg Med. 2002;23(2):117-24.
Poku JK, Bellamkonda-athmaram VR, Bellolio MF, et al. Failure of prospective validation and derivation of a refined clinical decision rule for chest radiography in emergency department patients with chest pain and possible acute coronary syndrome. Acad Emerg Med. 2012;19(9):E1004-10.
Kirschner J, Shah K, Runde D, et al. Patterns in computed tomography utilization among emergency physicians in an urban, academic emergency department. Emerg Radiol. 2014;21(6):577-81.
Laméris W, Van randen A, Van es HW, et al. Imaging strategies for detection of urgent conditions in patients with acute abdominal pain: diagnostic accuracy study. BMJ. 2009;338:b2431.
Hlibczuk V, Dattaro JA, Jin Z, Falzon L, Brown MD. Diagnostic accuracy of noncontrast computed tomography for appendicitis in adults: a systematic review. Ann Emerg Med. 2010;55(1):51-59.e1.
Keyzer C, Cullus P, Tack D, De maertelaer V, Bohy P, Gevenois PA. MDCT for suspected acute appendicitis in adults: impact of oral and IV contrast media at standard-dose and simulated low-dose techniques. AJR Am J Roentgenol. 2009;193(5):1272-81.
Worrall JC, Jama S, Stiell IG. Radiation doses to emergency department patients undergoing computed tomography. CJEM. 2014;16(6):477-84.
Barbic D, Barbic S, Dankoff J. An exploration of Canadian emergency physicians’ and residents’ knowledge of computed tomography radiation dosing and risk. CJEM. 2015;17(2):131-9.
American College of Radiology. Appropriateness Criteria. https://acsearch.acr.org/list
Tramèr MR, Von elm E, Loubeyre P, Hauser C. Pharmacological prevention of serious anaphylactic reactions due to iodinated contrast media: systematic review. BMJ. 2006;333(7570):675.
Smith-bindman R, Lipson J, Marcus R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med. 2009;169(22):2078-86.
Emerg Radiol. 2014 Dec;21(6):577-81. doi: 10.1007/s10140-014-1237-x. Epub 2014 May 17.
Other FOAMed Resources on Emergency Radiology
Rick Bukada on Contrast is Unnecessary for Most Abdominal CTs on EP Monthly
Journal Jam 3 Ultrasound vs CT for nephrolithiasis on EM Cases
Abdominal x-ray interpretation on Life in the Fast Lane
CT contrast reaction myths on EMDocs
Radiation in Medicine Basics on The Short Coat