Author: Anna Pickens, MD (@AnnaEMin5, Creator of EMin5) // Edited by: Alex Koyfman, MD (@EMHighAK), Brit Long, MD (@long_brit), and Manpreet Singh, MD (@MprizzleER)
Welcome to this week’s edition of EMin5 by Dr. Anna Pickens. Today we are focusing on Mumps!

Mumps is a virus that, especially before the vaccine came out, mostly affects kids.
However in recent years we have been seeing some outbreaks again. According to the CDC, about 1,900 cases have been reported in 2018 as of October:

Mumps is an RNA virus that is spread like many other URIs – through respiratory droplets, direct contact and fomites.
The timeline for transmission can be a little tricky, because it takes about 2 weeks for any symptoms to show up, and the first few days, Mumps looks like any other non specific viral syndrome. Only after a few days do patients develop some of the classic features such as parotitis that tip us off that we might be dealing with mumps.
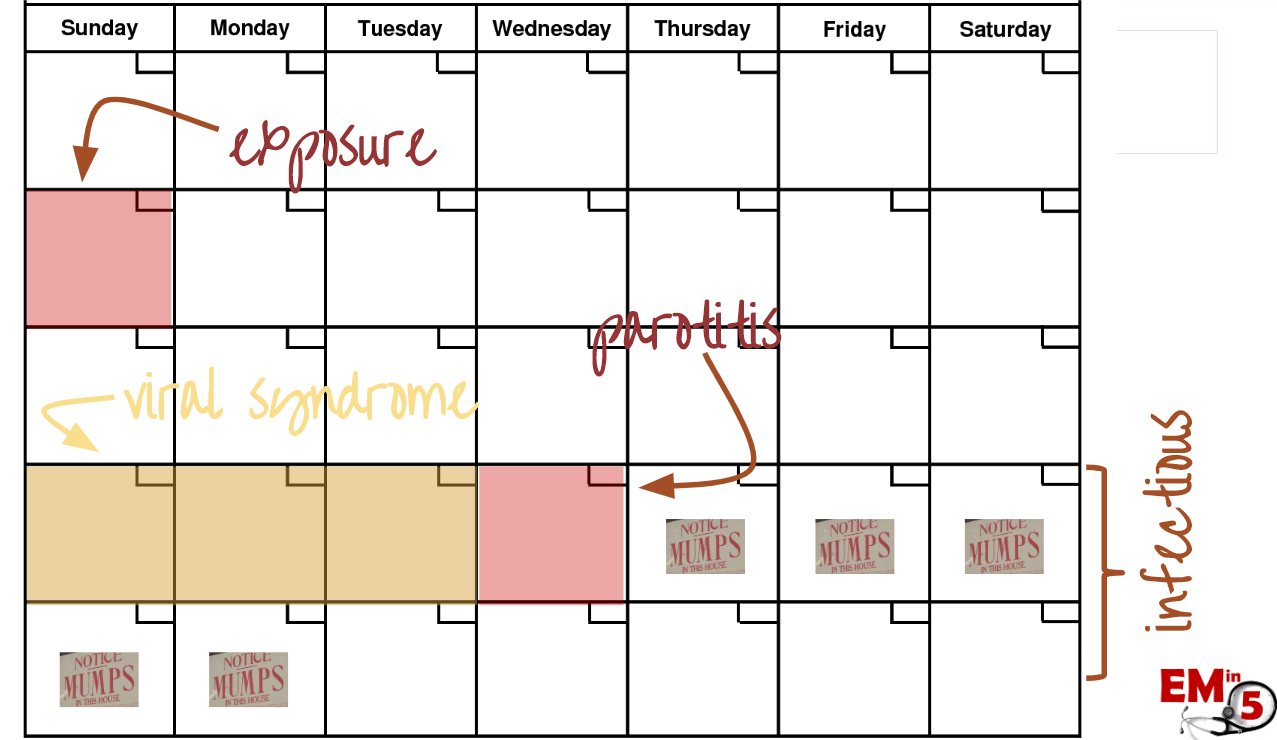
And unlucky for the friends and family of the patient, the highest level of viral shedding takes place in the few days BEFORE those classic symptoms start.
So first patients will get that classic viral syndrome of malaise, headache, myalgias, fevers, etc

Then a few days later they might develop some of the classic findings that Mumps is so famous for, such as parotitis.

Parotitis is by far the most common, as up to 90% of patients with mumps develop this classic swelling. Parotitis is an infection of the duct epithelium of the parotid gland, and in addition to making the patient look like a chipmunk, it can be painful and somewhat tense. It should NOT, however, be warm and red (then think cellulitis). This swelling can last up to 10 days.
- Interesting fact: now that we have the MMR vaccine, the most common cause of parotitis is actually from other viruses, such as CMV, parainfluenza, influenza, coxsackie, echovirus and HIV. But certainly think of Mumps if you see it.
Another common symptom in Mumps is orchitis:
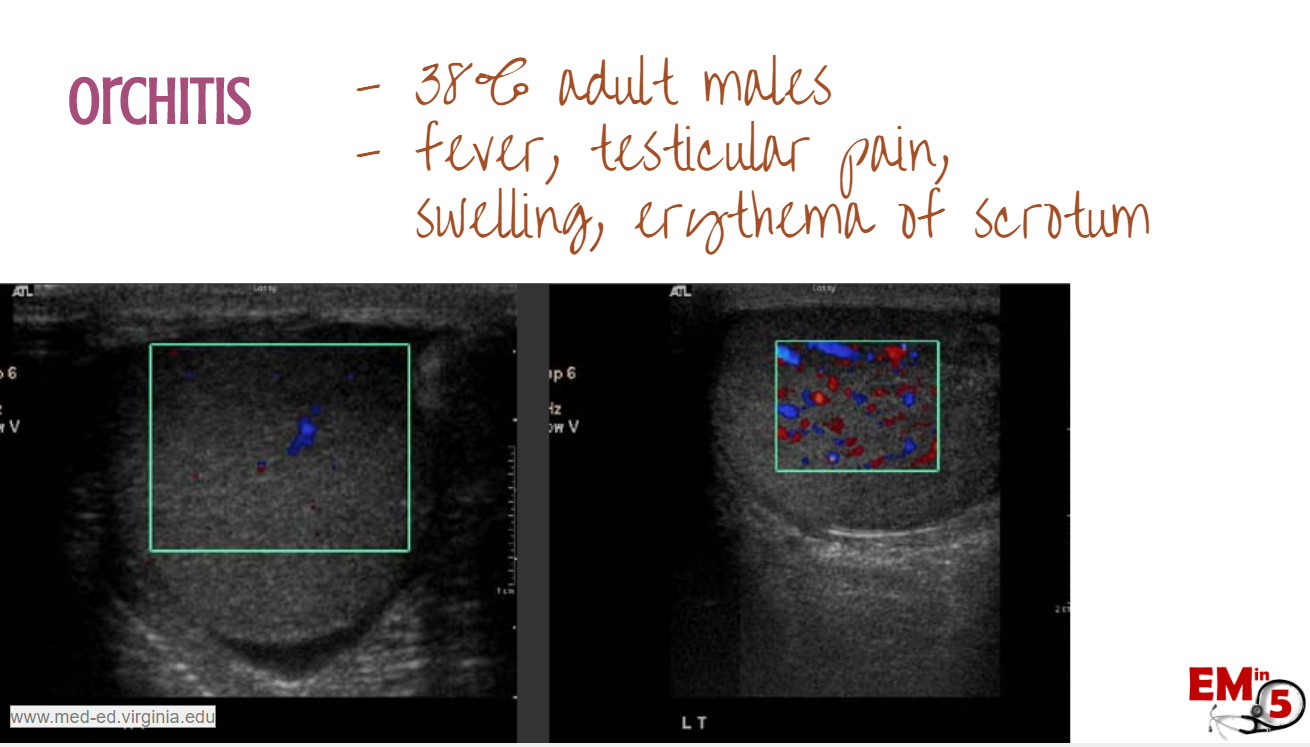
We see it in 38% of adult males, and it can result in painful swelling of the testes, along with fever. On ultrasound, you may see edema of the testes and increased vascular flow.
The female equivalent of oophoritis is much less common (7% post pubertal).
Interestingly, if we tested everyone’s CSF with mumps, we would find that about 50% had evidence of mumps aseptic meningitis.
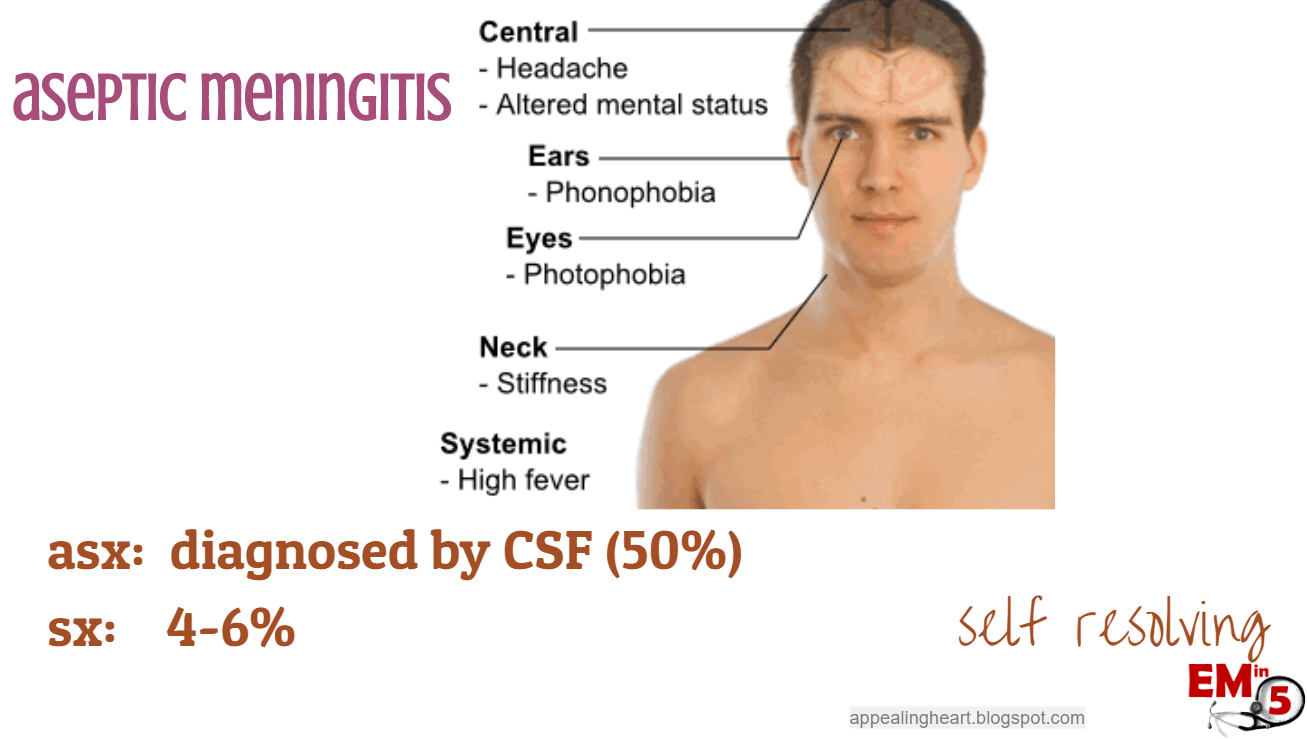
But only about 4-6% have actual symptoms of meningitis. And since it is self resolving, there is really no reason to test for it unless we need to rule out bacterial meningitis.
Mumps can also cause Guillain-Barre, arthritis, pancreatitis, and myocarditis.
AND, before the vaccine, mumps was the #1 cause of unilateral sensorineural hearing loss.
- Personal anecdote: My grandmother was deaf in one ear after she got Mumps as a child, and recalled well her Dad hanging a curtain across the living room to separate her from the other siblings while she was in isolation.
Pregnancy: If you do diagnose a pregnant patient with mumps, you can let them know that there are no known associated birth defects, but there is a possible increased risk of miscarriage in the first trimester (studies differ in this finding).

Mumps is really a clinical diagnosis, but it can be detected in the saliva, CSF and urine through viral culture.

Treatment is mainly supportive – antipyretics, push the fluids to prevent dehydration, and lots of snuggles and chicken soup.

However, because Mumps is so contagious, the CDC does recommend telling patients to stay home from work and school for 5 days after one of the classic symptoms starts (such as parotitis). Also make sure to ask families about their vaccine status to see if anyone needs an update.
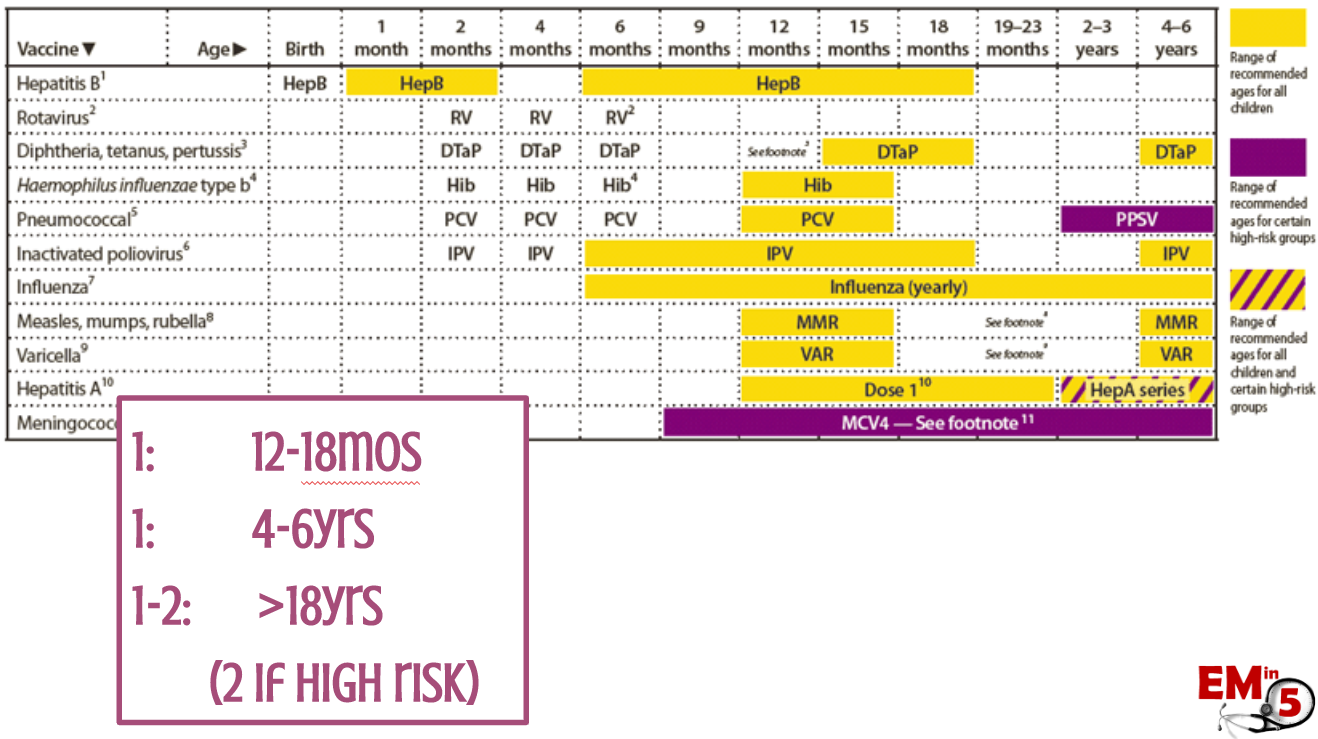
The MMR vaccine is pretty effective.

It is recommended at 12-18 months, 4-6 years, and then again around 18 years old. And if you are “high risk” (living in a dormitory, working in healthcare – here’s looking at you!) then it is recommended to have a second one as an adult.
And if your child is unvaccinated during a school outbreak, the CDC recommends that the child stay home for 25 days (!) after the last parotitis episode onset. Another reason to vaccinate.
So next time you see some parotid swelling… think Mumps, isolate for 5 days, and get their friends vaccinated!
Suggested/Further Reading:
- CDC: https://www.cdc.gov/mumps/index.html
- Pediatric EM Morsels: https://pedemmorsels.com/mumps/
- AAFP: https://www.aafp.org/afp/2017/0615/p786.html








