Author: Katherine M. Buckley, MD (EM Resident Physician, UT Southwestern, Dallas, TX) // Reviewed by: Alex Koyfman, MD (@EMHighAK) and Brit Long, MD (@long_brit)
Welcome to EM@3AM, an emDOCs series designed to foster your working knowledge by providing an expedited review of clinical basics. We’ll keep it short, while you keep that EM brain sharp.
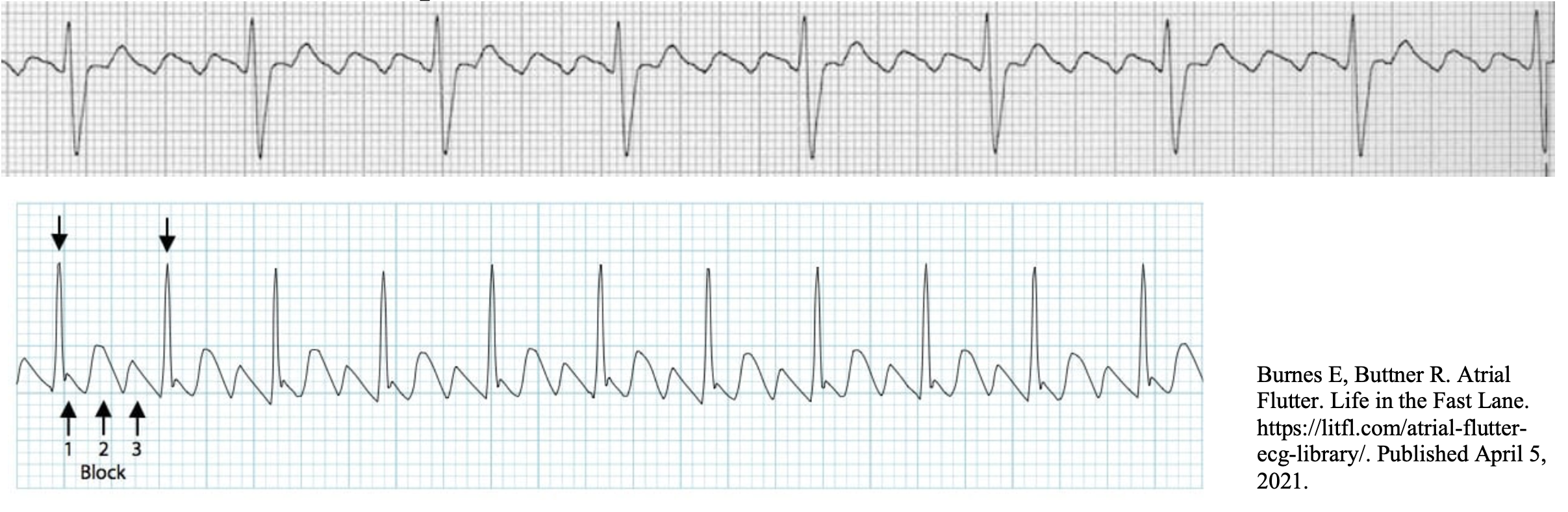
Case: A 70-year-old male with insulin-dependent diabetes, coronary artery disease, and one-vessel CABG presents with palpitations and angina for one day. He is in no acute distress. His vital signs include BP 148/96, HR 150, RR 18, SpO2 96%, and T 37.2C. Below is his EKG. What is this rhythm, and what are two first-line medications for rate control?

Answer: Atrial flutter with 2:1 block; CCB or beta-blockers
Classification:
- Narrow, regular-complex tachydysrhythmia due to a single reentrant circuit within the atria
- Can be irregular if there is an AV block
- Atrial rate commonly 300 beats/min but can range between 250-350 bpm2
- Ventricular rate determined by AV conduction ratio
- Ratio of 2:1 is most common and produces a ventricular rate of 150 beats/min
- 3:1 → 100 bpm
- 4:1 → 75 bpm
- Typical atrial flutter:
- Reentrant arrhythmia due to an impulse that rotates around the right atrium
- The slow area of conduction that sustains the circuit is the cavotricuspid isthmus (tissue located between the IVC and tricuspid annulus)3
- Circuit typically rotates in a counterclockwise direction → “sawtooth” EKG pattern
- Negative flutter waves in inferior leads II, III, aVF and positive atrial deflections in V14
- Negative flutter waves in inferior leads II, III, aVF and positive atrial deflections in V14

-
- If re-entry is clockwise, this is “reverse” typical flutter
- Positive flutter waves in inferior leads and negative atrial deflections in V1
- Less common clinically
- If re-entry is clockwise, this is “reverse” typical flutter

- Atypical atrial flutter:
- Atrial tachycardias that are caused by a reentrant circuit that do not involve the cavotricuspid isthmus but any portion of the atria5
- Typically associated with structural heart disease, cardiac surgery, or ablation5
- ECG will be different than typical/reverse flutter
- Often more refractory to treatment
Pathogenesis/Risk Factors:
- 80% of patients with atrial flutter are male6
- Incidence in the US is 200,000 new cases per year5
- Uncommon to occur in a structurally normal heart or without a predisposing event or preexisting comorbidity
- Similar risk factors for AFib: pulmonary disease, diabetes, HTN, older age, obesity, and thyrotoxicosis5
- Can occur after starting an antiarrhythmic drug for AFib
- Patients can develop atypical atrial flutter after AFib ablation due to circuits created by scarring
Clinical Presentation:
- Flutter can either be paroxysmal or persistent, and patients can either be asymptomatic or symptomatic
- Symptoms are largely dependent on the ventricular rate
- Dyspnea, angina, or palpitations, and less likely hypotension or syncope
- A rapid ventricular rate decreases the ventricular filling time and, this coupled with asynchronous atrial to ventricular contraction, can lead to heart failure2
- Chronic flutter with RVR can lead to tachycardia-induced cardiomyopathy4
- Flutter has at least as high of a risk for thromboembolic event as AFib → same risk stratification for anticoagulation as in AFib7
Management:
- Adenosine can transiently block the AV node to reveal flutter waves and can help diagnose

- Rate control
- Indications: immediate rate control to reduce symptoms in stable patient or chronic therapy to prevent symptoms or cardiomyopathy9
- Since the rate is determined by the AV node, drugs that slow AV conduction are used
- Diltiazem: increases refractory of AV node → slows conduction through AV node → decreases ventricular rate
- Initial: 0.25 mg/kg (10-20 mg) IV bolus over 2 minutes
- Second (if no reduction in HR by 20% or HR >100 bpm): 0.35 mg/kg (15-25 mg) IV9
- Infusion: 5 mg/h, titrate by 5 mg/h to max of 15 mg/h (to 20% reduction in HR or HR < 100)
- Transition to 60-90 mg PO during/after infusion
- Stop infusion about 2h after oral dose2
- Contraindicated in patients with severe heart failure or AV-block
- Esmolol: quick onset and short duration of action9
- Initial: 0.5 mg/kg bolus over 1 min followed by 50 mcg/min infusion
- Second: if no response after 4 min, another bolus followed by infusion of 100 mcg/min
- Third: if no response after 4 min, then final bolus followed by 150 mcg/min infusion
- Infusion can be increased to max of 200 mcg/min if no response after third bolus
- Alternate option: start infusion at 50 mcg/min without a bolus and increase the rate by 50 mcg/min q30min
- Metoprolol: 5 mg IV q5min to 15 mg total
- Risk stratify for anticoagulation
- Rhythm Conversion:
- If patient is unstable/RVR is causing hypotension, myocardial ischemia, or pulmonary edema → synchronized cardioversion, starting at 50 J2
- If patient is at increased risk for thromboembolic event, can give DOAC or LMWH (in patients with renal impairment, prosthetic valve, mitral stenosis) before or immediately after conversion2
- If patient is stable and symptomatic, refer to the Ottawa Aggressive Protocol for synchronized cardioversion management guidelines
- Conversion rate of 85% and ED mean length of stay of 12h10
- Consider electrical conversion if clear history of arrhythmia for < 48h or if unclear history and patient is anticoagulated on warfarin with therapeutic INR for 3 consecutive weeks10
- Higher rate of success with anterior-posterior electrode position compared to the anterior-lateral position11
- Ottawa Aggressive Protocol:
- If patient is unstable/RVR is causing hypotension, myocardial ischemia, or pulmonary edema → synchronized cardioversion, starting at 50 J2

- Pharmacologic conversion with antiarrhythmics (procainamide, ibutilide, flecainide) for the stable low-risk patient2
- Ibutilide is the most effective and can convert approximately 60% of patients5
- > 60 kg- 1 mg IV over 10 min4
- < 60 kg- 10 mcg/kg IV over 10 min4
- Due to risk of torsades, it is contraindicated in patients with hypokalemia, prolonged QT, or heart failure
- Ibutilide is the most effective and can convert approximately 60% of patients5
Anticoagulation:
- Clear guidelines remain controversial
- Use a scoring system such as CHADS, CHA2DS2-VASc for evaluation and determination of risk of thromboembolic event.
- No difference in risk of thromboembolic event between pharmacologic versus electrical cardioversion11
- Thromboemboli is due to existing thrombi within the atrium at the time of conversion or the formation of one after conversion in the setting of depressed atrial function
- Cardiovert without anticoagulation if there is a very clear history that onset of flutter was < 48h and patient with low risk of stroke10
- Thromboembolic event rate without anticoagulation in this cohort of patients is around 0.7%11
- Rate does increase with increasing CHA2DS2-VASc score (0.4% with a score of 0 versus 2.3% in those with a score of 5 or greater)11
- If < 48h and patient at high risk of stroke (mechanical valve, rheumatic heart disease, history of TIA/stroke), proceed with rate control, and patient should receive OAC for 3 weeks before and 4 weeks following cardioversion12
- If timeframe unknown or high risk of stroke, can perform transesophageal echocardiography to evaluate for left atrial thrombus
- If no thrombus identified, can proceed with cardioversion
- Must be pretreated with heparin and continue with OAC for four weeks
- If thrombus identified, defer cardioversion
- If no thrombus identified, can proceed with cardioversion

Disposition:
- Admit:
- On-going medical management (pulmonary edema, myocardial ischemia, respiratory distress)
- Infusion for rate control
- Longer duration of symptoms prior to ED presentation
- Discharge
- Consider cardiology consult prior to discharge
- About 90% of patients with atrial flutter electrically converted can be discharged with low incidence of stroke in one year2
- Anticoagulation as discussed above
Atrial flutter vs. atrial fibrillation:
- Atrial flutter is due to one reentrant circuit whereas AFib is due to multiple reentrant circuits firing at random
- Disorganized atrial contraction in AFib leads quivering of the atrium, poor ventricular filling, and decreased cardiac output
- AFib EKG: irregularly irregular rhythm and the absence of P-waves
- Both are managed by rhythm conversion or rate control
- Atrial flutter is responsive to less energy with electrical conversion (AFib requires 150-200J)2
- Patients with flutter have less risk of hemodynamic instability due to the organized contraction of the atria
- Both increase the risk of embolism and share the same risk stratification for anticoagulation
Pearls:
- A regular, narrow-complex tachycardia with a rate of 150 beats/min (+/- 5 beats/min) strongly suggests atrial flutter with 2:1 conduction2
- CCB and beta-blockers for rate control in the stable patient
- Synchronized cardioversion (25-50J) in the unstable patient
- Adenosine can slow down rate long enough to expose flutter waves
- Flutter also requires thromboembolic risk stratification for anticoagulation

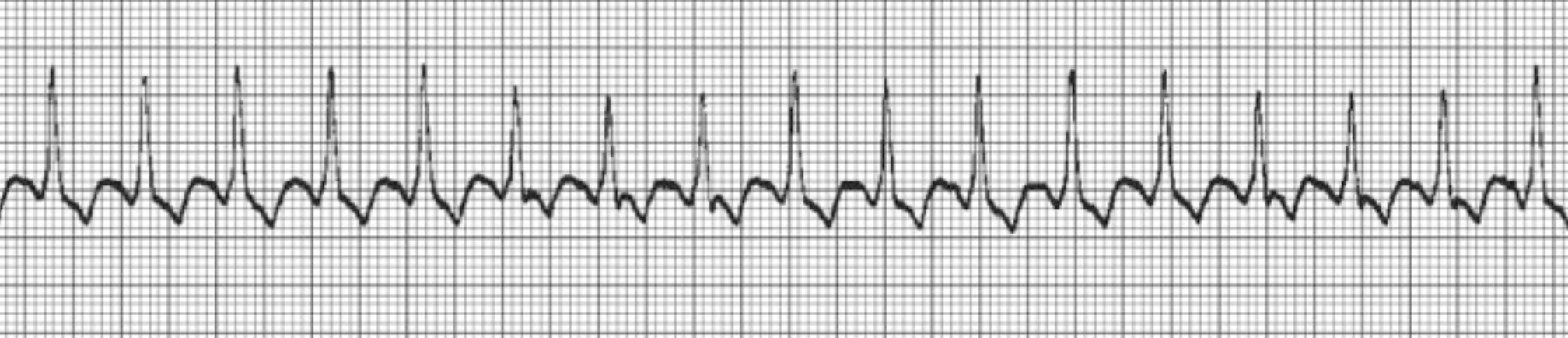
A 67-year-old man with a history of coronary artery disease and congestive heart failure presents to the emergency department with 3 days of palpitations and fatigue. A rhythm strip is obtained and shown above. Which of the following is the most likely diagnosis?
A) Atrial fibrillation
B) Atrial flutter
C) Junctional escape rhythm
D) Multifocal atrial tachycardia
Answer: B
Atrial flutter is a cardiac dysrhythmia characterized by a regular, narrow QRS complex, supraventricular tachycardia. It occurs most often due to underlying structural heart disease such as heart failure, chronic obstructive pulmonary disease, or obstructive sleep apnea, which causes remodeling of myocardial tissue over time. This remodeling alters electrical conduction through myocardial tissue, causing the atrial automaticity foci to be extremely irritable, which results in a rapid series of atrial depolarizations. Since the atrioventricular (AV) node has a long refractory period, only one out of a series of atrial depolarizations conducts through the ventricles. The ratio of nonconducted to conducted atrial beats through the AV node can further characterize atrial flutter. In this patient’s electrocardiogram, for every two atrial beats, there is one ventricular beat indicated by the QRS complex. Therefore, the atrial flutter in the electrocardiogram is 2:1.

Atrial fibrillation (A) is characterized by an irregularly irregular rhythm with a narrow QRS complex in the absence of P waves. Junctional escape rhythm (C) is characterized by a narrow QRS complex rhythm with a rate of 40–60 beats/minute, without association between atrial activity and the QRS complexes. Multifocal atrial tachycardia (D) is characterized by an irregular rhythm with at least three different P wave morphologies in the same lead, suggestive of separate atrial activity arising from multiple different ectopic foci.
Further Reading:
FOAMed
- ALiEM – Calcium before Diltiazem
- Dr. Smith’s ECG Blog – Atrial Flutter mimics STE
- EM Docs – Unstable AFib
- LITFL – Atrial Flutter
References
- Burnes E, Buttner R. Atrial Flutter. Life in the Fast Lane. https://litfl.com/atrial-flutter-ecg-library/. Published April 5, 2021.
- Tintinalli JE, Ma OJ, Yealy DM, et al. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 9th ed. New York, NY: McGraw Hill Education; 2020.
- Daoud EG, Morady F. Pathophysiology of Atrial Flutter. Annual Review of Medicine. 1998;49(1). doi:10.1146/annurev.med.49.1.77
- Wellens HJJ. Contemporary Management of Atrial Flutter. Circulation. 2002;106(6):649-652. doi:10.1161/01.cir.0000027683.00417.9a
- Phang R, Prutkin J, Ganz L. Overview of Atrial Flutter. UpToDate. www.uptodate.com. Published March 9, 2021.
- Cosío FG. Atrial Flutter, Typical and Atypical: A Review. Arrhythmia & Electrophysiology Review. 2017;6(2). doi:10.15420/aer.2017.5.2
- Halligan SC, Gersh BJ, Brown RD, et al. The Natural History of Lone Atrial Flutter. Annals of Internal Medicine. 2004;140(4). doi:10.7326/0003-4819-140-4-200402170-00008
- Smith S. What happens when you give adenosine to a patient with this rhythm? Dr. Smith’s ECG Blog. http://hqmeded-ecg.blogspot.com/2017/08/what-happens-when-you-give-adenosine-to.html. Published August 23, 2017.
- Ganz L, Prutkin J. Control of Ventricular Rate in Atrial Flutter. UpToDate. www.uptodate.com. Published May 19, 2020.
- Stiell IG, Clement CM, Perry JJ, et al. Association of the Ottawa Aggressive Protocol with Rapid Discharge of Emergency Department Patients with Recent-Onset Atrial Fibrillation or Flutter. CJEM. 2010;12(03):181-19. doi:10.1017/s1481803500012227
- Brandes A, Crijns HJ, Rienstra M, et al. Cardioversion of Atrial Fibrillation and Atrial Flutter Revisited: Current Evidence and Practical Guidance for a Common Procedure. EP Europace. 2020;22(8):1149-1161. doi:10.1093/europace/euaa057
- Stiell IG, Macle L. Canadian Cardiovascular Society Atrial Fibrillation Guidelines 2010: Management of Recent-Onset Atrial Fibrillation and Flutter in the Emergency Department. Canadian Journal of Cardiology. 2011;27(1):38-46. doi:10.1016/j.cjca.2010.11.014
- Burnes E, Buttner R. Atrial Fibrillation. Life in the Fast Lane. https://litfl.com/atrial-fibrillation-ecg-library/. Published June 6, 2021.








