Author: Jackie Nguyen, MD (EM Resident Physician, UTSW – Dallas, TX); Joshua Kern, MD (Assistant Professor of EM/Attending Physician, UTSW – Dallas, TX) // Reviewed by: Sophia Görgens, MD (EM Resident Physician, Zucker-Northwell NS/LIJ, NY); Cassandra Mackey, MD (Assistant Professor of Emergency Medicine, UMass Chan Medical School); Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Welcome to EM@3AM, an emDOCs series designed to foster your working knowledge by providing an expedited review of clinical basics. We’ll keep it short, while you keep that EM brain sharp.
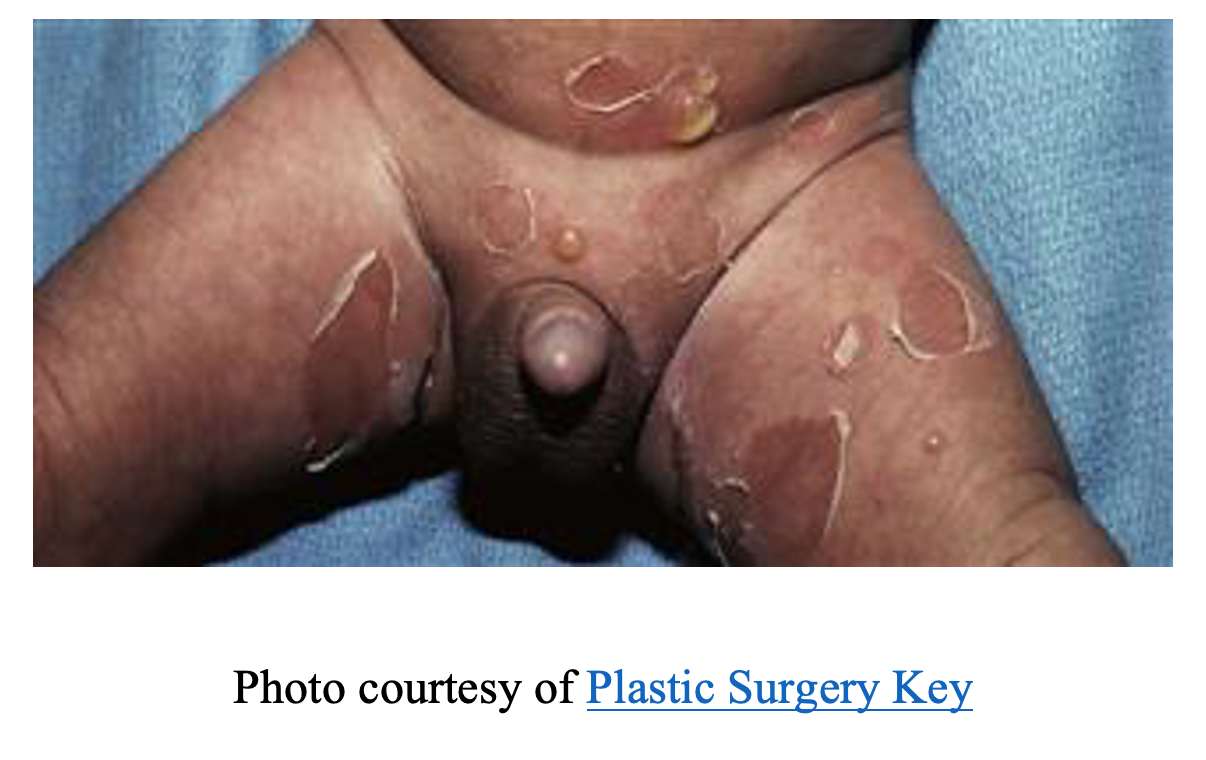
A 9-month-old male with no medical history born full term presents with a rash and fever for 4 days. Mom reports the rash began in the axillae and groin and spread to the trunk. She notes the rash started as small, erythematous lesions that have progressed to bullae which are unroofing. The rash is associated with intermittent fevers (Tmax of 102°F) and diarrhea. The patient’s vital signs include T 101.2F, BP 93/56, HR 163, RR 40, SpO2 of 99% on room air. On physical exam, the patient appears pale with a prolonged capillary refill. His skin exam is significant for an erythematous rash with scattered ruptured bullae with brown crust and a collarette of scales across the trunk, axillae, perineal and flexural thigh areas.
What is the diagnosis?
Definition
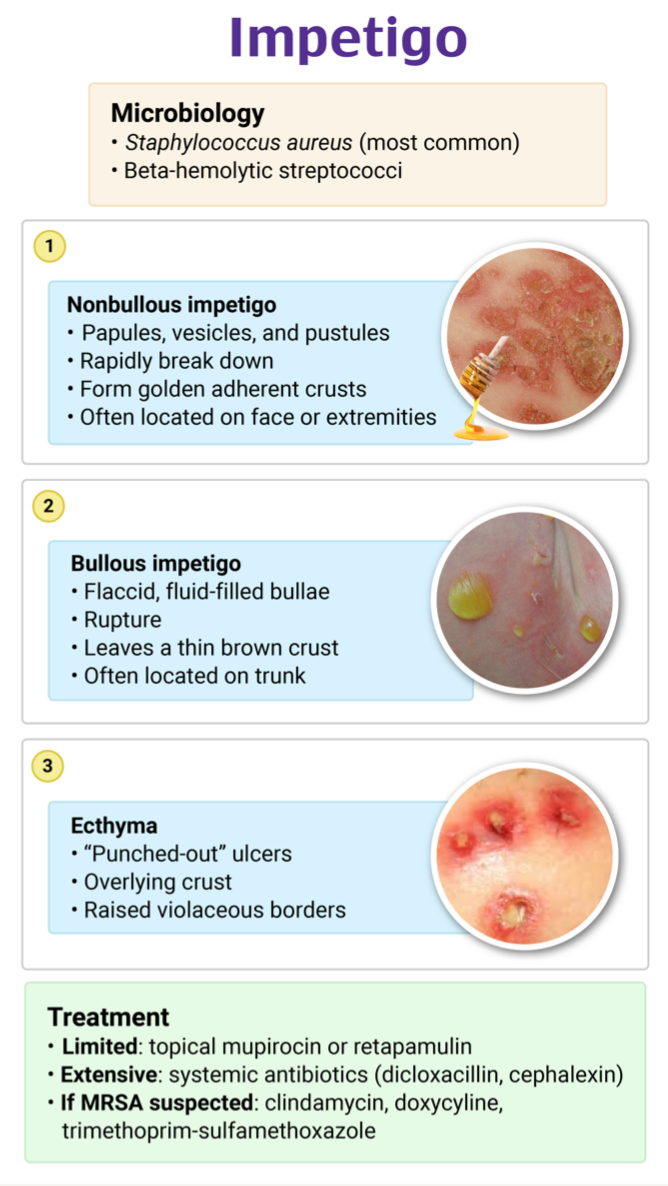
- Impetigo is a bacterial infection of the superficial keratin layer of the skin1, 2
- Two forms:
- Non-bullous impetigo (impetigo contagiosa) accounts for approximately 70% of cases
- Further divided into primary (direct infection of healthy, intact epidermis) or secondary (infection after trauma or insult to the skin)
- Bullous impetigo accounts for approximately 30% of cases
- Non-bullous impetigo (impetigo contagiosa) accounts for approximately 70% of cases
Epidemiology
- Highly contagious and more frequently affecting the pediatric population, predominately ages 2-5 years of age1-4
- >162 million children are thought to be affected by impetigo worldwide at one time
- Bullous impetigo more often affects neonates and infants
- >162 million children are thought to be affected by impetigo worldwide at one time
- Spread through direct skin-to-skin contact after exposure to excoriated lesions
- Can also be spread through fomites
- Often swiftly disseminated in schools, daycares, nurseries, etc. or through use of shared grooming devices.
- Incidence is highest in the summertime and greatest in areas of poor socio-economic status, crowding, and/or tropical to sub-tropical climates
- Personal hygiene is directly related to inoculation
- Diabetes mellitus also increases the risk of developing impetigo
- Staphylococcus aureus and group A Streptococcus (GAS) are the most commonly implicated pathogens, but can also be a result of anaerobic bacteria
- Can be infected by one of the two or a combination of them
- Bullous impetigo is exclusively caused by Staphylococcus aureus
- MRSA becoming increasingly more prevalent
- Can be infected by one of the two or a combination of them
Pathophysiology
- Individual can be colonized with the responsible bacterial pathogen or be inoculated with contact with a lesion1, 2
- Can be colonized in the pharynx, nasal passages, axillae, or perineal regions
- Intradermal inoculation of bacteria occurs after some insult to the skin leading to minor trauma or disrupted skin
- Can have skin disruption through eczema, scabies, herpetic lesions, insect bites, etc.
- Can also have infection of healthy, intact skin although the mechanism of inoculation is unclear
- In bullous impetigo, the exfoliative toxins from Staphylococcus aureus cause cell adhesion loss in the keratin layer of the epidermis
- This results in the characteristic flaccid bullae
Clinical Presentation
- Rash characterized by honey-colored crusted lesions on an erythematous base
- Generally painless, but can sometimes be pruritic and burn1-3
- Begins as blanchable erythematous maculopapular lesions that progress to vesicles and pustules
- In bullous impetigo, vesicles and pustules progress to flaccid bullae that rupture easily
- Brown crust and collarette of scales remain after rupture

-
- These will rupture leaving behind the characteristic lesions after about one week
- Non-bullous impetigo typically affects the face around the nares and/or the extremities
- Bullous impetigo typically affects the extremities, trunk, and intertriginous areas
Extra-mucocutaneous manifestations
- Can have mild systemic symptoms like fever, anorexia, diarrhea, and malaise although this is more uncommon1, 2
- Can also have regional lymphadenopathy
Diagnosis
- Diagnosis is primarily clinical1, 2, 5
- May be difficult to differentiate bullous impetigo and similar rashes such as SJS/TEN, blistering autoimmune rashes, etc
- Can distinguish bullous impetigo from mimickers as systemic involvement is rare, is Nikolsky sign negative, does not involve mucosal surfaces, and begins as small vesicles that progress to flaccid bullae which rupture leaving scales and crusting
- Fram stain and culture are not often performed, but should be considered in recurrent cases or if there are concerns for MRSA
- Skin biopsy may be performed if refractory to treatment
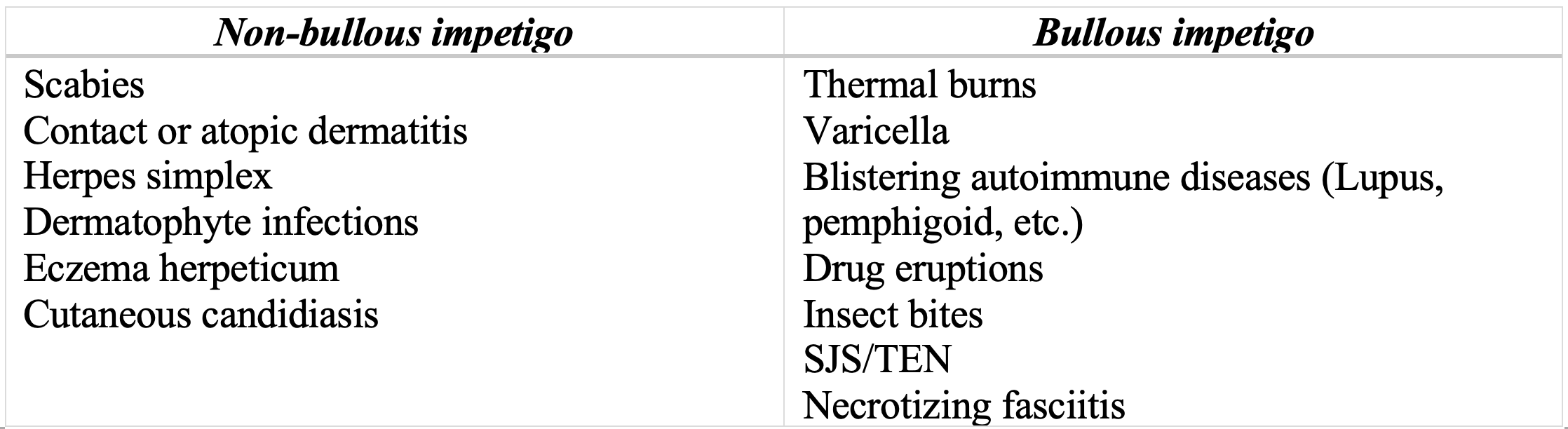
Differential Diagnoses1, 2
Complications
- Rare but can occur1, 2
- Infection can progress to cellulitis, sepsis, osteomyelitis, lymphadenitis, meningitis, septic arthritis, and staphylococcal scalded skin syndrome
- Poststreptococcal glomerulonephritis is the most serious complication and affects 5% of patients1, 2
- Can be asymptomatic with microscopic hematuria but can progress to fulminant nephritis with gross hematuria, generalized edema, hypertension, and fever
- Occurs 1-2 weeks after initial infection
- Typically, patients are asymptomatic with favorable prognosis
- More often seen as a complication of pharyngitis
- Antibiotic treatment of impetigo has not demonstrated decreased incidence or prevention of developing glomerulonephritis2, 6
- Growing evidence to suggest Group A streptococcal skin infections like impetigo lead to rheumatic fever7, 8, 9
- Mechanism not yet elucidated but thought to trigger immune-mediated reaction resulting in rheumatic fever development
Treatment
- Impetigo is a self-limited disease and can resolve spontaneously in 2-3 weeks1, 6, 10
- Topical antibiotics that cover Staphylococcus aureus and group A Streptococcus are often given for non-bullous impetigo to lessen the duration of disease and prevent the spread5
- Treatment can also decrease complication rates
- Mupirocin and retapamulin are the first line treatments
- Applied to the affected area two to three times daily for five days
- Triple antibiotics ointments are not effective treatments and are not recommended
- Crust should be gently removed with soap and water prior to antibiotic application
- For bullous impetigo or extensive non-bullous impetigo (greater than five lesions, deeper tissue involvement, and/or oral cavity involvement), systemic antibiotics should be prescribed for seven days1, 6, 10
- Treatments of choice include cephalosporins like cephalexin, amoxicillin-clavulanate, dicloxacillin
- If confirmed MRSA infection, utilize antibiotics that will provide appropriate coverage like doxycycline, trimethoprim / sulfamethoxazole, or clindamycin
- Important to avoid other people and maintain personal hygiene through handwashing and cleaning of linens and clothes
- Children can return to school/daycare 24 hours after initiating adequate antimicrobial therapy as they are no longer contagious
- Sores can be covered with gauze or bandage to prevent contact
Prognosis
- The majority heal with no complication, and scarring and pigmentation changes are rare2
Pearls
- Impetigo is a bacterial infection of the superficial epidermis often caused by S. aureus and GAS
- The rash is often characterized by vesicles/pustules that rupture leaving honey-color crusted lesions or bullae leaving collarette of scales and brown crust
- Lesions are highly contagious and should be treated with topical or oral antibiotics especially in extensive cases of non-bullous impetigo and all cases for bullous impetigo
- Prognosis is generally good with no scarring; complications are rare but can include glomerulonephritis

A healthy 5-year-old girl presents to the ED with her mother for a rash that has worsened over several days. The rash was initially located only around the nose and mouth but is now spreading to the arms. Physical exam reveals a well-appearing child with erythematous lesions and honey-colored crusts around her nose and mouth. Several lesions are also present on each of her upper extremities. Which of the following is the best treatment?
A) Oral cephalexin
B) Topical antifungal agent
C) Topical corticosteroids
D) Topical mupirocin
Answer: A
Impetigo is a superficial bacterial skin infection, most common in children ages 2 to 5 years. It is highly communicable, spreading easily among individuals in close contact. Risk factors include warm temperatures, poverty, crowding, poor hygiene, and scabies. The most commonly affected areas are the face, neck, and extremities. Lesions start as erythematous papules that form vesicles, which rupture to form honey-colored crusts. Diagnosis is made clinically, based on the appearance of the rash. Localized infection with a small number of lesions may be treated topically, either with mupirocin or retapamulin. For patients with larger infections or numerous lesions, oral antibiotics are recommended. Oral cephalexin or trimethoprim-sulfamethoxazole are appropriate choices.
A topical antifungal agent (B) is not effective for treating impetigo. Topical mupirocin (D) is appropriate for a localized infection, but this patient has lesions on her face and both of her upper extremities. Topical corticosteroids (C) are effective for treating eczema but not impetigo.
Further FOAMed
References
- Hartman-Adams H, Banvard C, Juckett G. Impetigo: diagnosis and treatment. Am Fam Physician. Aug 15 2014;90(4):229-35.
- Johnson MK. Impetigo. Adv Emerg Nurs J. Oct/Dec 2020;42(4):262-269. doi:10.1097/tme.0000000000000320
- Nardi NM, TJ. S. Impetigo. Treasure Island (FL): StatPearls Publishing. 2022. https://www.ncbi.nlm.nih.gov/books/NBK430974/
- Bowen AC, Mahé A, Hay RJ, et al. The Global Epidemiology of Impetigo: A Systematic Review of the Population Prevalence of Impetigo and Pyoderma. PLoS One. 2015;10(8):e0136789. doi:10.1371/journal.pone.0136789
- Brazel M, Desai A, Are A, Motaparthi K. Staphylococcal Scalded Skin Syndrome and Bullous Impetigo. Medicina (Kaunas). 2021;57(11):1157. Published 2021 Oct 24. doi:10.3390/medicina57111157
- Stevens DL, Bisno AL, Chambers HF, et al. Practice Guidelines for the Diagnosis and Management of Skin and Soft Tissue Infections: 2014 Update by the Infectious Diseases Society of America. Clinical Infectious Diseases. 2014;59(2):e10-e52. doi:10.1093/cid/ciu296
- Parks T, Smeesters PR, Steer AC. Streptococcal skin infection and rheumatic heart disease. Current Opinion in Infectious Diseases. 2012;25(2):145-153.
- Carapetis JR, Beaton A, Cunningham MW, et al. Acute rheumatic fever and rheumatic heart disease. Nat Rev Dis Primers. 2016;2:15084. Published 2016 Jan 14. doi:10.1038/nrdp.2015.84
- Impetigo: Information For Clinicians. Published 2022. Accessed December 12, 2022. https://www.cdc.gov/groupastrep/diseases-hcp/impetigo.html
- May PJ, Tong SYC, Steer AC, et al. Treatment, prevention and public health management of impetigo, scabies, crusted scabies and fungal skin infections in endemic populations: a systematic review. Tropical Medicine & International Health. 2019;24(3):280-293. doi:https://doi.org/10.1111/tmi.13198








