Author: Daniel M. Good, MD, MPH (EM Resident Physician, UTSW/Parkland Memorial, Dallas, TX) // Edited by: Alex Koyfman, MD (@EMHighAK) and Brit Long, MD (@long_brit)
Welcome to EM@3AM, an emDOCs series designed to foster your working knowledge by providing an expedited review of clinical basics. We’ll keep it short, while you keep that EM brain sharp.
A 36-year-old male with a history of HIV presents to the ED complaining of dyspnea on exertion and fatigue. He is homeless and has been poorly compliant with his anti-retroviral medications. He reports several weeks of non-productive cough and subjective fever. Pulse is 102/min, respirations 22/min, blood pressure 112/68 mm Hg, temperature 38º C (100.4º F), and pulse oximetry 93% on room air. His conjunctivae are pale. There is a painful ulcer to the distal aspect of the tongue and scattered petechiae on his legs. Skin exam demonstrates scattered petechiae. Laboratory evaluation reveals WBC 2,000/microL (70% PMN, 25% lymphocytes, 4% monocytes, eosinophils 0.9%, basophils 0.1%), hemoglobin of 8.5 g/dL, and platelets 90,000/microL. LDH is 220 U/L (normal 140-280 U/L). CD4 cell count and HIV viral load are pending. What do the exam and lab findings suggest?
Answer: Pancytopenia due to disseminated histoplasmosis
Background & Diagnosis:
- Pancytopenia is a hematologic manifestation of an underlying disease state.
- Cases may be reversible or irreversible.1
- Many of the diseases that cause pancytopenia also cause bicytopenia (decrease in 2 of the 3 peripheral blood lines), thus diagnosis of bicytopenia warrants a similar evaluation to pancytopenia.1
- Pancytopenia is characterized by a decrease in all3 peripheral blood cell lines defined as:1
- Leukocyte count that is low typically manifests in the form of an absolute neutrophil count (ANC) <1,800 cells/microL AND
- Hemoglobin < 13 g/dL in males and < 12 g/dL in non-gravid females AND
- Platelet count < 150,000/microL
Presentation:
- Patients with pancytopenia can be asymptomatic, manifest symptoms associated with the decrease of one or more of the cell lines, or manifest symptoms of the underlying cause of their pancytopenia.
- Anemia – malaise, generalized weakness, fatigue, dyspnea on exertion, headache, orthostatic light-headedness, angina, decreased exercise tolerance, decrease libido2
- Leukopenia/leukopenia – often asymptomatic, but can have recurrent infections2
- Thrombocytopenia – petechiae, purpura, mucosal bleeding2
Pathogenesis & Causes:3
- The pathogenesis of pancytopenia can be classified in 1 of 3 ways, with common causes falling into each category.
- Impaired cell production– results from a congenital or acquired defect in progenitor stem cells, deficient micronutrients, or a myelophthisic process that mechanically restricts the area in which hematopoiesis can occur.
- Aplastic anemia – acquired aplastic anemia is the #1 cause of pancytopenia, but remains rare with an incidence of 2 cases per million people in developed countries.4
- Congenital – Fanconi anemia, dyskeratosis congenita, Shwachman-Diamond syndrome, GATA2 associated syndromes, Amegakaryocytic thrombocytopenia
- Acquired4
- Drugs – Chemotherapeutic agents, antiepileptic drugs, chloramphenicol, steroids, NSAIDs, ethanol abuse, colchicine
- Toxins – Benzene, ingestion of colchicine containing plants (meadow saffron, wild saffron, autumn crocus), mustard gas
- Radiation
- Infection – Hepatitis viruses (A, B, C), HIV, EBV, CMV, HHV-6, parvovirus B19
- Bone marrow infiltration
- Metastatic solid tumors
- Infiltrative leukemia or lymphoma
- Primary myelofibrosis
- Infection – tuberculosis, leishmania, histoplasma
- Nutritional deficiency
- Vitamin B12
- Folate
- Copper
- Myelodysplastic syndrome – acquired clonal stem cell disorder most commonly seen in elderly males. Peripheral smear with hypogranulated neutrophils
- Aplastic anemia – acquired aplastic anemia is the #1 cause of pancytopenia, but remains rare with an incidence of 2 cases per million people in developed countries.4
- Impaired cell production– results from a congenital or acquired defect in progenitor stem cells, deficient micronutrients, or a myelophthisic process that mechanically restricts the area in which hematopoiesis can occur.
- Peripheral cell destruction – immune cell or soluble immune factor mediate lysis of cells
- Autoimmune – Systemic lupus erythematosus, chronic lymphocytic leukemia (CLL), autoimmune lymphoproliferative syndrome (ALPS), and common variable immunodeficiency disease (CVID)
- Splenic sequestration – accumulation and destruction of blood cells in an enlarged spleen. Can be seen in any diseases that cause splenomegaly, such as cirrhosis, congestive heart failure, malignancies, sickle cell disease, and inherited metabolic storage diseases
- Mixture of both
- Paroxysmal nocturnal hemoglobinemia
- Transfusion related graft vs. host disease
- Hemophagocytic lymphohistiocytosis – presents with fever, hepatomegaly, lymphadenopathy, and/or neurologic symptoms
Evaluation:3
- Pancytopenia may not be suspected on initial presentation and instead is found on routinely ordered complete blood counts.
- A careful history should be taken with attention to the following:
- Prior personal or family history of anemia, thrombocytopenia, and/or leukopenia
- Drug or toxin exposure
- Ethanol abuse
- History of eating disorders, bariatric surgery, dietary restrictions, GI malabsorption
- Recent B symptoms (fever, weight loss, night sweats)
- Physical exam for the presence of:
- Fever or focal sign of infection
- Lymphadenopathy
- Hepatosplenomegaly
- Active bleeding, including oro- and nasopharyngeal, vaginal, and gastrointestinal
- Stigmata of underlying cause of pancytopenia
- Laboratory analysis
- Peripheral smear – to evaluate for abnormal peripheral cells indicative of leukemia, lymphoma, myelophthisic processes, cell lysis, macrocytosis
- Reticulocyte count – to evaluate bone marrow response to the pancytopenia
- ESR and CRP – to evaluate for underlying inflammatory process
- HIV and hepatitis serologies – evaluate for underlying causes
- Liver function tests – to evaluate for underlying liver dysfunction
- LDH – to evaluate for hemolysis
- Prothrombin time, partial thromboplastin time, serum ferritin – if DIC or hemophagocytic lymphohistiocytosis is suspected1
- Imaging – guided by history and physical to evaluate for underlying infection or cause of pancytopenia.
Management:
- An initial emergent resuscitation should take place, for any patient with respiratory or cardiovascular compromise.
- An emergent hematology consult should be placed for any patient with potentially life-threating disease (active bleeding, sepsis, cardiorespiratory compromise).
- Transfusion thresholds are similar to those of patients with isolated anemia, neutropenia, and thrombocytopenia.
- Anemia
- Asymptomatic patients: consider transfusion for hemoglobin ≤ 7 g/dL1,5,6
- Known coronary artery disease: consider transfusion for hemoglobin ≤ 8 g/dL5,6
- Symptoms of acute coronary syndrome: transfuse if hemoglobin ≤ 8 g/dL, and continuing transfusing to hemoglobin ≥ 10 g/dL if symptoms persist1,5,6
- Thrombocytopenia1
- Non-bleeding: consider transfusion for platelets of ≤ 10,000/microL
- Clinically significant bleeding: consider transfusion for platelets of ≤ 50,000/microL
- Concurrent oncologic emergencies should be managed similarly to those seen in isolation
- Neutropenic fever – defined as a single oral temperature ≥38.3º C (101º F) or sustain temperature of 38º C (100.4º F) for one hour AND ANC < 500 cells/microL.7
- These patients should receive empiric broad-spectrum antibiotics with anti-pseudomonal coverage – cefepime, meropenem, ceftazidime, and piperacillin-tazobactam are all reasonable monotherapies.7
- Vancomycin should be considered in those with pneumonia, catheter-related infections, skin or soft tissue infections, or those who are hemodynamically unstable, but is recommended for routine coverage outside these indications.7
- Disseminated intravascular coagulation – packed red blood cell transfusion for serious bleeding, platelet transfusion (as above), cryoprecipitate if fibrinogen < 100 mg/dL, and fresh frozen plasma if significant bleeding in the setting of elevated INR and/or partial thromboplastin time.2
- Tumor lysis syndrome – aggressive IV hydration along with a xanthine oxidase inhibitor (rasburicase or allopurinol).2
- Neutropenic fever – defined as a single oral temperature ≥38.3º C (101º F) or sustain temperature of 38º C (100.4º F) for one hour AND ANC < 500 cells/microL.7
- Concurrent hypercalcemia
- Treat with aggressive IV hydration.2
- Concurrent acute renal failure
- Evaluate for hyperkalemia and treat with IV calcium, insulin + glucose, albuterol, bicarbonate, kayexalate, diuretics, and nephrology consult for dialysis as appropriate.2
- Anemia
Disposition:
- Almost all patients with undifferentiated pancytopenia should be admitted, with a hematology consult, for further evaluation. Additional inpatient testing, including flow cytometry, bone marrow biopsy, spleen biopsy, serum protein electrophoresis, vitamin B12, folate, haptoglobin, and coombs test, may be warranted.3

A previously healthy 36-year-old man presents to the emergency department with a three day history of fatigue, gingival bleeding, and worsening shortness of breath. He notes he returned from a volunteer trip to India three months ago and notes that after his return he had intermittent fevers for two weeks. He has also had abdominal pain and bloating, vomiting, and decreased appetite for a few days. Vital signs reveal slight tachycardia and relative hypotension. Exam is otherwise unremarkable. Laboratory work is performed and the complete blood count returns first with the following results: hemoglobin 7.6 g/dL, white blood cell count 2.5 x 109/L, and platelets 40 x 109/L. What infectious agent is most likely responsible for this patient’s symptoms and laboratory values?
A) Dengue
B) Hepatitis B
C) Norovirus
D) Yellow fever
Answer: B
The patient in this question is presenting with viral symptoms and the laboratory evaluation thus far is consistent with pancytopenia. Pancytopenia refers to decreases in all peripheral blood lineages and is considered to be present when all three cells lines are below the normal reference range. Pancytopenia can be associated with a multitude of disease states so a thoughtful history, physical and careful laboratory evaluation can help narrow the diagnosis. A common cause of pancytopenia is viral infection, with hepatitis being the most common. Hepatitis has been shown to cause severe bone marrow aplasia, which leads to the pancytopenia seen. The symptoms usually occur two to three months after acute infection. Of the options given above, this patient most likely had a hepatitis B infection.
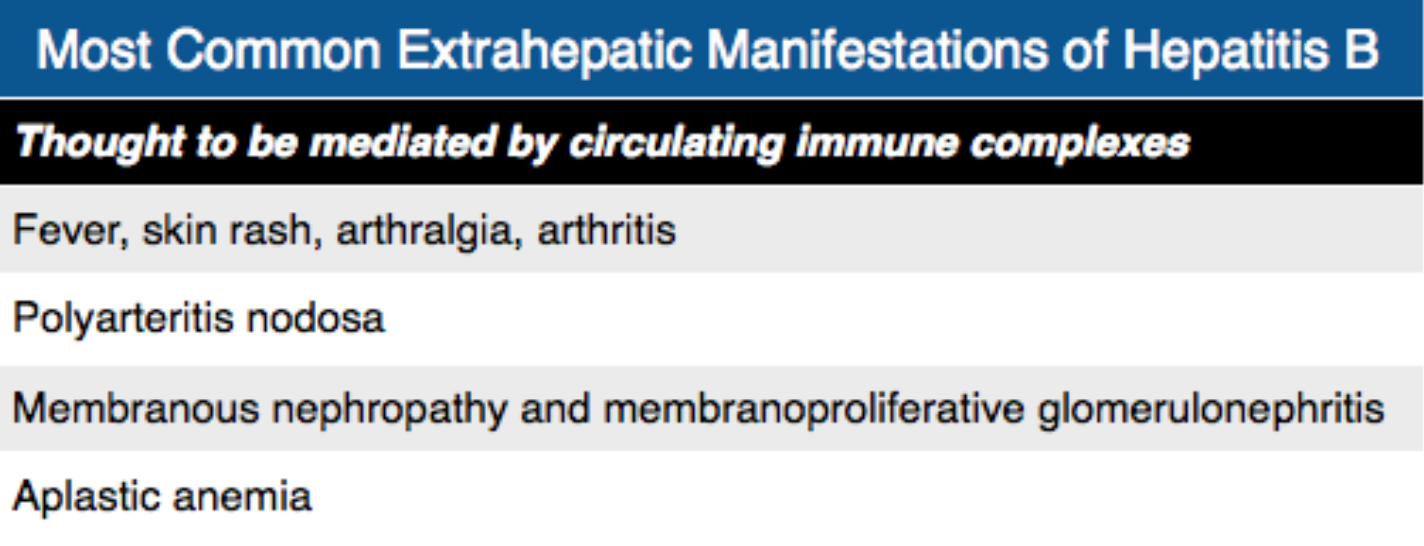
Dengue (A) is a mosquito-borne viral illness or hemorrhagic fever that is usually self-limiting and rarely lethal. Characteristic laboratory abnormalities found in dengue fever include thrombocytopenia but less often leukopenia. Anemia is not associated with the disease unless the patient has hemorrhagic shock. Norovirus (C) is the most common cause of viral gastroenteritis. It generally does not cause significant laboratory abnormalities and does not cause hepatosplenomegaly. Yellow fever (D) is a mosquito-borne disease that can present as an acute viral illness, viral hepatitis or hemorrhagic fever. The initial symptoms are generally those of a viral illness and the disease is self-limited. Some patients can go on to develop worsening infection with hepatitis and hemorrhage. Laboratory values generally show leukopenia and thrombocytopenia but hemoconcentration and increased hemoglobin levels are more typical unless hemorrhage is present. Yellow fever is a good diagnosis to have on the differential in this patient but it is not the most likely cause of his symptoms.
Further Reading:
More FOAMed
- Swaminathan A. CORE EM: Emergency Management of Blast Crisis. EMdocs.net http://www.emdocs.net/core-em-emergency-management-of-blast-crisis/
References
- Berliner N. Approach to the adult with unexplained pancytopenia. Schrier SL, ed. UpToDate. Waltham, MA: UpToDate Inc. https://www.uptodate.com(Accessed on July 28, 2019)
- Walls, RM., & Rosen, P. (2018). Rosen’s emergency medicine: Concepts and clinical practice(9th ed.). Philadelphia, PA: Elsevier/Saunders.
- Gnanaraj J, et al. Approach to pancytopenia: Diagnostic algorithm for clinical hematologists. Blood Rev. 2018; 32(5):361-367.
- Seiff CA. Introduction to acquired and inherited bone marrow failure. Hematol oncol Clin North Am. 2018;32(4):569-580.
- Carson JL, Kleinman S. Indications and hemoglobin thresholds for red blood cell transfusion in the adult. Silvergleid AJ, ed. UpToDate. Waltham, MA: UpToDate Inc. https://www.uptodate.com(Accessed on July 28, 2019)
- Carson JL, et al. Red blood cell transfusion: a clinical practice guideline from the AABB. Ann Intern Med. 2012;157(1):49-58.
- Frierfield AG, et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious disease society of America. Clin Infect Dis. 2011;52(4):e56.








