Author: Brit Long, MD (@long_brit, EM Attending Physician, San Antonio, TX) // Edited by: Alex Koyfman, MD (@EMHighAK, EM Attending Physician, UTSW / Parkland Memorial Hospital)
Welcome back to emDocs Cases! Today we have case-based discussion on a core EM topic, with a look at some controversy and cutting-edge treatments.
A 28-year-old female presents with right sided headache and one episode of vomiting, but no abdominal pain. The headache is not sudden in onset, but has rather worsened gradually over the last several hours. She denies fever, neck stiffness/pain, trauma, ingestion, vision changes/eye pain, and any other complaints. She has had several headaches in the past similar to the present headache. Her VS and exam are normal, including gait, cerebellar system, motor/sensory, reflexes, gait, and cranial nerves.
How are headaches classified?
Headaches affect over 50% of patients annually, with close to 4% of ED visits for headache.1-3 Women are more commonly affected.4-6 In the ED, physicians must first evaluate for potentially life-threatening causes of headache, as well as treat patient symptoms.
Primary headaches are not life-threatening, but they can cause significant morbidity. These headaches include tension, migraine, cluster, paroxysmal hemicranias, hemicrania continua, trigeminal neuralgia, and medication overuse.6-12
Secondary headaches are dangerous and may result in death if not diagnosed and treated. These include intracranial hemorrhage, sentinel bleed, meningitis, encephalitis, abscess, tumor, carotid/vertebrobasilar dissection, reversible cerebral vasoconstriction syndrome (RCVS), cerebral venous thrombosis, temporal arteritis, idiopathic intracranial hypertension, hypertensive encephalopathy, posterior reversible encephalopathy syndrome (PRES), acute hydrocephalus (e.g., colloid cyst obstructing third ventricle), pituitary apoplexy, acute angle closure glaucoma, and carbon monoxide poisoning.6-12
What evaluation is necessary in the ED?
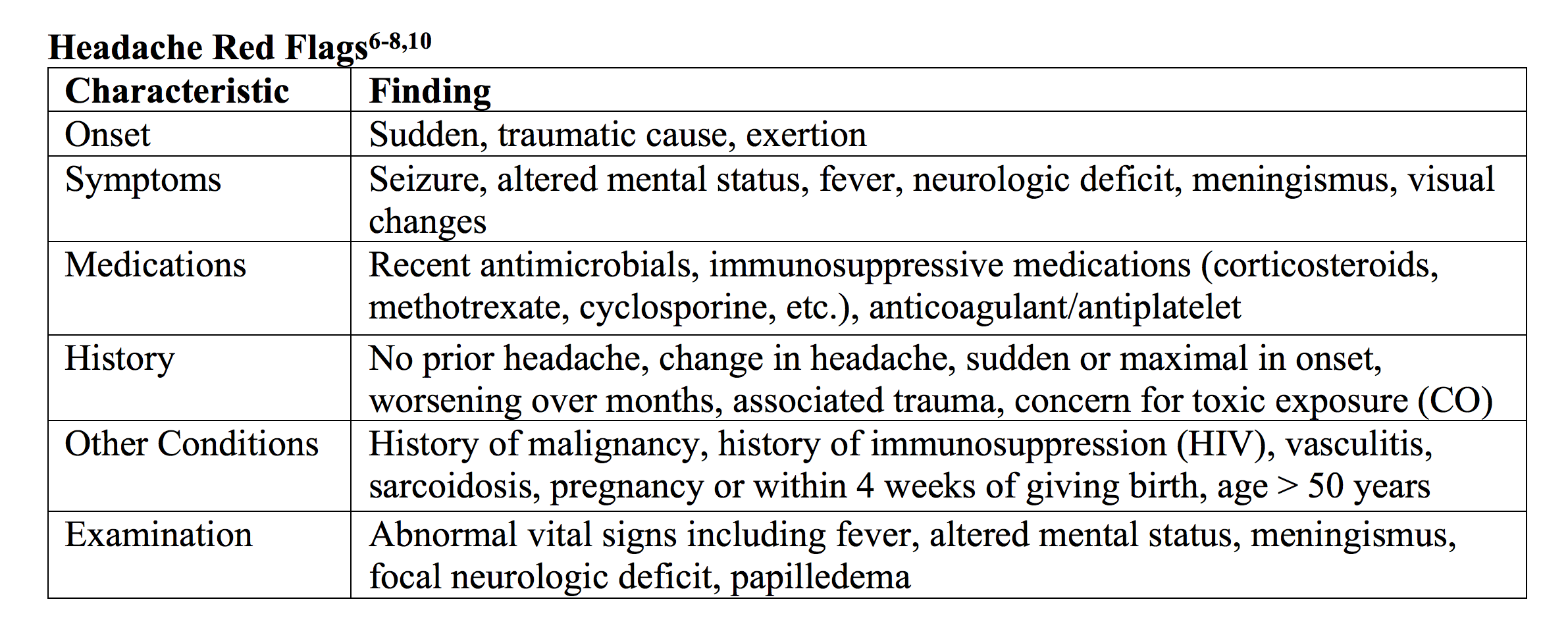
The most important component of the ED evaluation is focused history and physical exam (including HEENT and neurologic systems). This evaluation comes down to looking closely for “red flags”.6-8 Patients with a benign headache should have no major change in headache pattern, no red flag on history and exam, and no high-risk comorbidity.6-8,10
What is a primary, or benign, headache?
Most headaches managed in the ED are benign, with 90% of these headaches classified as tension, migraine, or cluster. These differ in symptoms, but our job in the ED is to not diagnose the specific type of primary headache, but rather exclude a secondary dangerous headache.3,4,7-13
Migraines have several criteria for diagnosis, shown in the table below. Several factors increase the likelihood of migraine headache, including nausea/vomiting, photophobia, and limitation in work/daily function due to headache (2 of 3 of these criteria possess sensitivity over 80%).3-5,12,13

What treatments are available, and which medications are efficacious?
Emergency physicians have another major role in the care of these patients by treating symptoms. This is one area where we can truly help patients. Treatment of nausea, vomiting, and pain should be a primary goal in ED care, no matter the headache etiology.6-12 Over twenty different types of medications are available, many with different routes (parenteral, intranasal, subcutaneous, and oral). Many of these medications are provided in the “headache cocktail”, which varies based on the physician, institution, patient preferences, and other factors. The best medication should provide fast, sustained pain relief, while having little to no side effects. Unfortunately, there is no perfect medication, and over one third of patients managed in the ED for headache experience sustained pain relief.10,14 Medication complications include vascular problems, extrapyramidal effects, and gastrointestinal issues such as gastritis or hemorrhage.14,15 The American Headache Society released updated recommendations in 2016 for headache treatment.9

As you can see, clinicians have a large number of options…What should you choose?
Many studies have evaluated medication efficacy for benign headaches. The rest of this post will look at some of the more common medications used for headache treatment in the ED.
1. Antidopaminergic agents – This is one of the best classes for symptom management, including headache pain and nausea relief.6-13 This class consists of phenothiazines and butyrophenones. Drowsiness is the most common side effect, and abnormal movements such as dystonia and akathisia may occur as well (more common with faster infusion rates).6,9,10
Chlorpromazine, prochlorperazine, and promethazine are phenothiazines. Chlorpromazine is provided in 0.1 mg/kg IV, with studies suggesting improved pain, photophobia, and phonophobia in migraines, with NNT of 2 for pain relief at one hour.16-21 Prochlorperazine is more commonly used in the U.S., with dosing 10 mg IV providing pain relief in up to 90% of patients.22-30 This medication has been compared to magnesium, valproic acid, sumatriptan, octreotide, and ketorolac, with literature suggesting superiority of prochlorperazine.22-30 Promethazine can be used in doses of 25 mg IM or IV (IV administration can produce soft tissue injury if the medication extravasates).5,31-33 Fewer studies have evaluated its use in the ED.
Butyrophenones include droperidol and haloperidol. Droperidol possesses strong literature support as an analgesic and antiemetic in headaches, with doses ranging from 0.1-8.25 mg IM providing effective pain relief. It may be provided IV as well.6-13,34-36 However, it possesses an FDA Black Box warning for QTc prolongation. Haloperidol provides analgesia that is comparable or better to other previously discussed medications.9-11,38-40 When compared to placebo, haloperidol provides pain relief in 80% of patients. 39
One of the most common medications used in a “headache cocktail” is metoclopramide, an antidopaminergic and serotonin receptor antagonist, often administered 10 mg IV or IM.9-11,24,26,40-45 This medication has significant literature support, with one meta-analysis suggesting a NNT of 4 for pain reduction.43 Akathisia is a potential side effect, which can be reduced with slower rate of infusion.9-11,40-44
2. Triptans – These medications are serotonin receptor agonists (5HT1B/1D), primarily used in the outpatient setting.8-13,21,23,46-48 One of the more common agents is sumatriptan 2.5-6 mg given subcutaneously, with an NNT of 2.5 for pain relief when compared to placebo.9-13,47 It can also be administered intranasally (10-20 mg) or PO (100 mg).10,11,46-48 Unfortunately, there are many potential side effects such as chest pain, shortness of breath, flushing, and worsening headache, with number needed to harm (NNH) of 4.47 This medication should not be used for patients with cardiovascular disease, uncontrolled hypertension, or pregnancy.9-13,47 To reduce the risk of overuse headache, patients should not use a triptan more than 2 days per week. Close to two thirds of patients may experience recurrent headache.47 Triptans also demonstrate efficacy in cluster headaches, with sumatriptan 6 mg subcutaneously demonstrating pain relief in 75% of patients at 20 minutes and intranasal sumatriptan also beneficial.49-51 Zolmitriptan is given in doses of 5-10 mg.51,52 A maximum of two doses in 24 hours is recommended.
3. NSAIDs – This class can be used for a variety of conditions, with evidence strongly supporting use in headaches. Ketorolac in doses 30 mg IV or 60 mg IM is one of the most commonly evaluated medications.6-13,53-55 IV and IM routes show up to 80% pain relief at 2 hours, with similar pain relief when compared to metoclopramide or chlorpromazine. 9-11,27,54 Naproxen 500-550 mg two times per day can reduce pain if used for patients with headache, but does not decrease headache recurrence.55 If taken daily, gastric protection is recommended, and extended use may cause chronic daily headaches.9-13,55
4. Acetaminophen – This medication is useful for headache therapy, with recent studies evaluating IV dosing.8-13,56,57 Studies have suggested equivalency to dexketoprofen 50 mg, with no adverse events. The medication outperforms the triptan class at 60 minutes in terms of pain relief, though not at 30 or 120 minutes.56,57 More research is needed, but this class is promising.
5. Steroids – Though early studies demonstrated analgesic benefits for acute treatment,58,59 more recent randomized studies do not suggest efficacy for acute pain treatment.60-64 However, steroids can reduce risk of headache recurrence in 24-72 hours, with NNT 9.9-13,65 Another meta-analysis and systematic review suggest similar results.66,67 This must be balanced with potential risks of steroids, especially with older patients and diabetics. The most common steroid utilized is dexamethasone, in doses of 8-16 mg. The most prevalent dose and route evaluated is dexamethasone 10 mg IV.9-13
6. Antihistamines – Diphenhydramine and promethazine are two medications from this class. This is a common component of the ED “headache cocktail”, based on studies suggesting elevated serum histamine and IgE levels in migraine patients, and patients with migraine may have higher prevalence of allergic rhinitis.68-72 Unfortunately, these agents do not possess strong literature support, with one study comparing metoclopramide versus metoclopramide + diphenhydramine suggesting no difference in pain, akathisia, or length of stay.68 This medication class may cause sedation, but likely do not assist in analgesia.9-13
7. Intravenous Fluids – Over 40% of ED headache patients are given IV fluids.4,5,9-13 Patients may have fluid loss from vomiting and decreased oral intake. However, concerning pain relief, a study evaluating IV fluids with metoclopramide versus metoclopramide alone found no difference in acute pain relief.73 If the patient appears dehydrated, IV fluids are helpful, but they otherwise likely do not assist in pain relief.
Going beyond the standard “headache cocktail”…
8. Oxygen – Supplemental oxygen is efficacious in cluster headaches and is recommended by headache guidelines.74,75 If cluster headache is suspected on clinical evaluation, oxygen should be given, though other headaches do not demonstrate a similar response to oxygen.6-13,74,75 In migraine or tension type headaches, oxygen is likely not helpful.
9. Valproic Acid – Though most commonly used for seizures, this medication has been used for headache management in doses of 300-1200 mg IV.9-13,54,76 Randomized controlled trials (RCTs) demonstrate varied efficacy for symptom improvement when compared to ketorolac, metoclopramide, and prochlorperazine.54,76-82 Contraindications include pregnancy, liver disease, and metabolic disorders such as urea cycle defects.
10. Propofol – Propofol demonstrates efficacy in analgesia for refractory headaches.9-13,83-85 Studies have evaluated varying doses of propofol. One study found propofol in 30-40 mg IV boluses (with 10-20 mg boluses every 3-5 minutes) had better pain relief and decreased adverse events when compared with sumatriptan. 85 Another study evaluated propofol 10 mg IV every 5-10 minutes up to 80 mg, finding this strategy was effective in analgesia.86 Propofol is useful in refractory pain relief, though close monitoring for hypotension and respiratory depression is recommended.
11. Ketamine – Finally to the NMDA antagonist that is changing emergency medicine, first in procedural sedation and now analgesia.6,9-13,86-90 Analgesic doses of 0.1-0.3 mg/kg IV as slow push have found ability to decrease pain, though one study suggests feelings of fatigue and insobriety were more common with ketamine.89 Ketamine in 100 mL of NS with slower infusion over 15 minutes may reduce these feelings, versus faster infusion over 5 minutes.91
12. Magnesium – Severe asthma/COPD, preeclampsia/eclampsia, atrial fibrillation…this medication possesses a variety of uses in the ED. For patients with headache, it can be given in doses of 1-2 g IV. However, RCT’s evaluating magnesium are not high quality, and the literature suggests magnesium does not consistently provide analgesia for severe headaches.92-95
13. Nerve Block – This includes several different blocks with an anesthetic, including the occipital nerve block and sphenopalatine ganglion block. The occipital nerve block has been studied in open label trials and observational cohorts, and studies suggest the block is effective in over 65% of patients.9-13,96
Another option is the sphenopalatine ganglion block, which reduces parasympathetic outflow and pain.97-99 Academic Life in EM has a great post on this procedure with video. Several studies suggesting benefit against placebo, though the studies are not well designed. Another study comparing bupivacaine versus saline placebo found no difference in pain relief at 15 minutes,99 though others suggest improved pain at 15 minutes, 30 minutes, and 24 hours.98,100
Intranasal lidocaine is helpful in patients with cluster headaches and should be used if this is suspected.101-105
14. Opioids – You can’t really talk about analgesia without discussing opioids. These are used in over 50% of patients in the ED for headache.9-13 However, we have a significant number of alternative agents. Plus, several societies recommend against opioids for headaches, as these medications may cause headache progression, increase frequency of revisit, and decrease efficacy of other headache treatments. 9-11,106-114 Opioids can also increase depression, anxiety and disability.116 If patients ask specifically for opioids, counseling on the risks of this treatment is recommended.
So when it comes down to it, what medications should you provide?
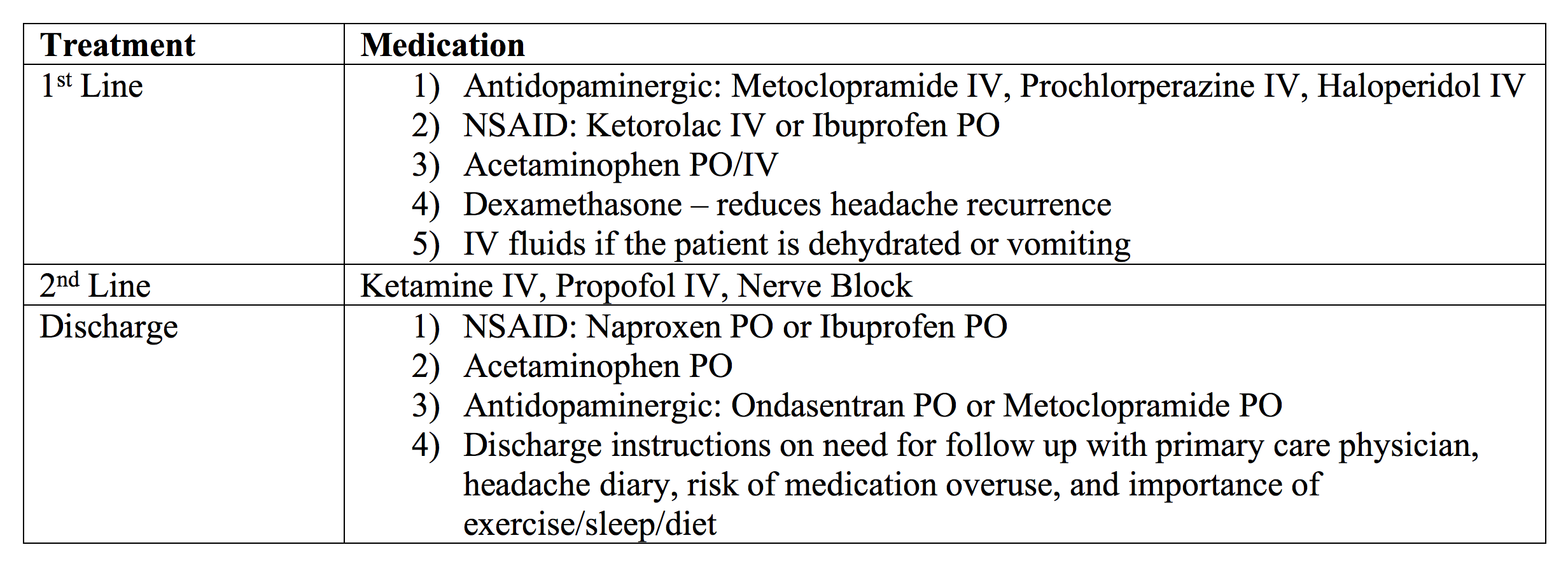
As discussed, you have many choices. Antidopaminergics in combination with an NSAID, acetaminophen, and dexamethasone will reduce pain and nausea. If ketorolac is chosen, recent literature suggests reduced dosing (10 or 15 mg) is as efficacious as 30 mg, with reduced risk of side effects.123 Triptans can be used, but only if there are no contraindications. If no response to first line agents, then nerve block, ketamine, or propofol can be used. Nerve block is useful for rapid pain relief.
Case Conclusion:
The patient feels improved with metoclopramide 10 mg IV, ketorolac 15 mg IV, acetaminophen 975 mg PO, and dexamethasone 10 mg IV. She desires discharge and will follow up with her primary care physician.
Key Points:
– Headache is divided into benign, primary causes and dangerous, secondary etiologies. Focused history and examination are recommended.
– Benign headaches include migraine, tension, cluster, and several others, but a specific diagnosis is not required in the ED.
– Management should also focus on symptom treatment for pain and nausea.
– A combination of medications is advised.
– Antidopaminergics have the strongest literature support. These should be used with NSAIDs and/or acetaminophen.
– Steroids likely decrease headache recurrence.
– Other treatments include ketamine, propofol, and nerve blocks. These are options for refractory headaches to other treatments.
References/Further Reading:
- Pitts SR, Niska RW, Xu J, et al. National Hospital Ambulatory Medical Care Survey: 2006 emergency department summary. Natl Health Stat Rep 2008;(7):1–38.
- National Center for Health Statistics. Centers for Disease Control and Prevention. Available at: http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2011_ed_web_tables.pdf. Accessed July 27, 2017.
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache. https://www.ichd-3.org. Accessed July 2017.
- Friedman BW, Hochberg ML, Esses D, et al. Applying the international classification of headache disorders to the emergency department: an assessment of reproducibility and the frequency with which a unique diagnosis can be assigned to every acute headache presentation. Ann Emerg Med. 2007;49(4):409–419, 419 e401–409.
- Vinson DR. Treatment patterns of isolated benign headache in US emergency departments. Ann Emerg Med. 2002;39(3): 215–222.
- Long B, Koyfman A. Headache. In Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8e.
- Edlow JA, Panagos PD, Godwin SA, et al, American College of Emergency Physicians. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with acute headache. Ann Emerg Med 2008;52(4):407–36.
- Tabatabai RR, Swadron SP. Headache in the emergency department: Avoiding misdiagnosis of dangerous secondary causes. Emerg Med Clin N Am 2016;34: 695–716.
- Orr SL, Friedman BW, Christie S, et al. Management of Adults With Acute Migraine in the Emergency Department: The American Headache Society Evidence Assessment of Parenteral Pharmacotherapies. Headache 2016;56:911-940.
- Friedman BW. Managing Migraine. Ann Emerg Med. 2017;69(2):202-207.
- Friedman BW, West J, Vinson DR, et al. Current management of migraine in US emergency departments: An analysis of the National Hospital Ambulatory Medical Care Survey. Cephalalgia. 2015;35:301-309.
- Gelfand AA, Goadsby PJ. A neurologist’s guide to acute migraine therapy in the emergency room. The Neurohospitalist 2012;2(2):51-59.
- Sinclair AJ, Sturrock A, Davies B, et al. Headache management: pharmacological approaches. Pract Neurol 2015;0:1–13.
- Friedman BW, Hochberg ML, Esses D, et al. Recurrence of primary headache disorders after emergency department discharge: frequency and predictors of poor pain and functional outcomes. Ann Emerg Med. 2008;52:696-704.
- Friedman BW, Bijur PE, Lipton RB. Standardizing emergency department-based migraine research: An analysis of commonly used clinical trial outcome measures. Acad Emerg Med. 2010; 17:72-79.
- Cameron JD, Lane PL, Speechley M. Intravenous chlorpromazine vs intravenous metoclopramide in acute migraine headache. Acad Emerg Med. 1995;2(7):597–602.
- Shrestha M, Singh R, Moreden J, Hayes JE. Ketorolac vs chlorpromazine in the treatment of acute migraine without aura. A prospective, randomized, double-blind trial. Arch Intern Med. 1996;156(15):1725–1728.
- Lane PL, McLellan BA, Baggoley CJ. Comparative efficacy of chlorpromazine and meperidine with dimenhydrinate in migraine headache. Ann Emerg Med. 1989;18(4):360–365.
- Bell R, Montoya D, Shuaib A, Lee MA. A comparative trial of three agents in the treatment of acute migraine headache. Ann Emerg Med. 1990;19(10):1079–1082.
- Bigal ME, Bordini CA, Speciali JG. Intravenous chlorpromazine in the emergency department treatment of migraines: a randomized controlled trial. J Emerg Med. 2002;23(2):141–148.
- Kelly AM, Ardagh M, Curry C, D’Antonio J, Zebic S. Intravenous chlorpromazine versus intramuscular sumatriptan for acute migraine. J Accid Emerg Med. 1997;14(4):209–211.
- Ginder S, Oatman B, Pollack M. A prospective study of i.v. magnesium and i.v. prochlorperazine in the treatment of headaches. J Emerg Med. 2000;18(3):311–315.
- Kostic MA, Gutierrez FJ, Rieg TS, et al. A prospective, randomized trial of intravenous prochlorperazine versus subcutaneous sumatriptan in acute migraine therapy in the emergency department. Ann Emerg Med. 2010;56(1):1–6.
- Jones J, Pack S, Chun E. Intramuscular prochlorperazine versus metoclopramide as single-agent therapy for the treatment of acute migraine headache. Am J Emerg Med. 1996;14(3): 262–264.
- Miller MA, Levsky ME, Enslow W, Rosin A. Randomized evaluation of octreotide vs prochlorperazine for ED treatment of migraine headache. Am J Emerg Med. 2009;27(2):160–164.
- Coppola M, Yealy DM, Leibold RA. Randomized, placebo controlled evaluation of prochlorperazine versus metoclopramide for emergency department treatment of migraine headache. Ann Emerg Med. 1995;26(5):541–546.
- Seim MB, March JA, Dunn KA. Intravenous ketorolac vs intravenous prochlorperazine for the treatment of migraine headaches. Acad Emerg Med. 1998;5(6):573–576.
- Jones EB, Gonzalez ER, Boggs JG, et al. Safety and efficacy of rectal prochlorperazine for the treatment of migraine in the emergency department. Ann Emerg Med. 1994;24(2):237–241.
- Jones J, Sklar D, Dougherty J, White W. Randomized double blind trial of intravenous prochlorperazine for the treatment of acute headache. JAMA. 1989;261(8):1174–1176.
- Trottier ED, Bailey B, Dauphin-Pierre S, Gravel J. Clinical outcomes of children treated with intravenous prochlorperazine for migraine in a pediatric emergency department. J Emerg Med. 2010;39(2):166–173.
- Information FPDS. http://www.fda.gov/Drugs/DrugSafetyPostmarket Drug Safety Information for Patients and Providers/Drug Safety Information for Healthcare Professionals/ucm182169.htm. Accessed July 2017.
- Scherl ER, Wilson JF. Comparison of dihydroergotamine with metoclopramide versus meperidine with promethazine in the treatment of acute migraine. Headache. 1995;35(5): 256–259.
- Davis CP, Torre PR, Williams C, et al. Ketorolac versus meperidine-plus-promethazine treatment of migraine headache: evaluations by patients. Am J Emerg Med. 1995;13(2): 146–150.
- Richman PB, Allegra J, Eskin B, et al. A randomized clinical trial to assess the efficacy of intramuscular droperidol for the treatment of acute migraine headache. Am J Emerg Med. 2002;20:39-42.
- Silberstein SD, Young WB, Mendizabal JE, et al. Acute migraine treatment with droperidol: A randomized, double-blind, placebo-controlled trial. Neurology 2003; 60:315.
- Miner JR, Fish SJ, Smith SW, Biros MH. Droperidol vs. prochlorperazine for benign headaches in the emergency department. Acad Emerg Med. 2001;8(9):873–879.
- Weaver CS, Jones JB, Chisholm CD, et al. Droperidol vs prochlorperazine for the treatment of acute headache. J Emerg Med. 2004;26(2):145–150.
- Gaffigan ME, Bruner DI, Wason C, et al. A Randomized Controlled Trial of Intravenous Haloperidol vs. Intravenous Metoclopramide for Acute Migraine Therapy in the Emergency Department. J Emerg Med 2015; 49:326.
- Honkaniemi J, Liimatainen S, Rainesalo S, Sulavuori S. Haloperidol in the acute treatment of migraine: a randomized, double-blind, placebo-controlled study. Headache 2006; 46:781.
- Kelley NE, Tepper DE. Rescue therapy for acute migraine, part 2: neuroleptics, antihistamines, and others. Headache 2012; 52:292.
- Acute migraine treatment in emergency settings. Comparative Effectiveness Review Summary Guides for Clinicians. Agency for Healthcare Research and Quality. www.ncbi.nlm.nih.gov/books/NBK164542/.
- Orr SL, Aubé M, Becker WJ, et al. Canadian Headache Society systematic review and recommendations on the treatment of migraine pain in emergency settings. Cephalalgia 2015; 35:271.
- Colman I, Brown MD, Innes GD, et al. Parenteral metoclopramide for acute migraine: meta-analysis of randomised controlled trials. BMJ 2004; 329:1369.
- Salazar G, Fragoso M, Vergez L, Sergio P, Cuello D. Metoclopramide as an analgesic in severe migraine attacks: an open, single-blind, parallel control study. Recent Pat CNS Drug Discov. 2011;6(2):141–145.
- Friedman BW, Esses D, Solorzano C, et al. A randomized controlled trial of prochlorperazine versus metoclopramide for treatment of acute migraine. Ann Emerg Med. 2008;52(4):399–406.
- Diener HC. Efficacy and safety of intravenous acetylsalicylic acid lysinate compared to subcutaneous sumatriptan and parenteral placebo in the acute treatment of migraine. A double-blind, double-dummy, randomized, multicenter, parallel group study. The ASASUMAMIG study group. Cephalalgia. 1999;19(6): 581–588; discussion 542.
- Akpunonu BE, Mutgi AB, Federman DJ, et al. Subcutaneous sumatriptan for treatment of acute migraine in patients admitted to the emergency department: a multicenter study. Ann Emerg 1995;25(4):464–469.
- Loder E. Triptan therapy in migraine. N Engl J Med. 2010;363:63-70.
- Treatment of acute cluster headache with sumatriptan. The Sumatriptan Cluster Headache Study Group. N Engl J Med 1991; 325:322.
- Ekbom K, Monstad I, Prusinski A, et al. Subcutaneous sumatriptan in the acute treatment of cluster headache: a dose comparison study. The Sumatriptan Cluster Headache Study Group. Acta Neurol Scand 1993; 88:63.
- van Vliet JA, Bahra A, Martin V, et al. Intranasal sumatriptan in cluster headache: randomized placebo-controlled double-blind study. Neurology 2003; 60:630.
- Cittadini E, May A, Straube A, et al. Effectiveness of intranasal zolmitriptan in acute cluster headache: a randomized, placebo-controlled, double-blind crossover study. Arch Neurol 2006; 63:1537.
- Taggart E, Doran S, Kokotillo A, et al. Ketorolac in the treatment of acute migraine: a systematic review. Headache. 2013;53: 277-287.
- Friedman B, Garber L, Yoon A, et al. Randomized trial of IV valproate vs metoclopramide vs ketorolac for acute migraine. 2014;82(11):976-983.
- Suthisisang CC,Poolsup N, Suksomboon N, et al. Meta-analysis of the efficacy and safety of naproxen sodium in the acute treatment of migraine. 2010 May;50(5):808-18.
- Turkcuer I, Serinken M, Eken C, et al. Intravenous paracetamol versus dexketoprofen in acute migraine attack in the emergency department: a randomised clinical trial.Emerg Med J. 2014;31(3):182-185.
- Leinisch E, Evers S, Kaempfe N, et al. Evaluation of the efficacy of intravenous acetaminophen in the treatment of acute migraine attacks: a double-blind, placebo-controlled parallel group multicenter study. 2005;117(3):396-400.
- Saadah HA. Abortive migraine therapy in the office with dexamethasone and prochlorperazine. Headache. 1994;34(6):366–370.
- Stiller J. Management of acute intractable headaches using i.v. therapy in an office setting. Headache. 1992;32(10):514–515.
- Rowe BH, Colman I, Edmonds ML, Blitz S, Walker A, Wiens S. Randomized controlled trial of intravenous dexamethasone to prevent relapse in acute migraine headache. Headache. 2008; 48(3):333–340.
- Donaldson D, Sundermann R, Jackson R, Bastani A. Intravenous dexamethasone vs placebo as adjunctive therapy to reduce the recurrence rate of acute migraine headaches: a multicenter, double-blinded, placebo-controlled randomized clinical trial. Am J Emerg Med. 2008;26(2):124–130.
- Kelly AM, Kerr D, Clooney M. Impact of oral dexamethasone versus placebo after ED treatment of migraine with phenothiazines on the rate of recurrent headache: a randomised controlled Emerg Med J. 2008;25(1):26–29.
- Friedman BW, Greenwald P, Bania TC, et al. Randomized trial of IV dexamethasone for acute migraine in the emergency department. Neurology. 2007;69(22):2038–2044.
- Baden EY, Hunter CJ. Intravenous dexamethasone to prevent the recurrence of benign headache after discharge from the emergency department: a randomized, double-blind, placebo controlled clinical trial. CJEM. Nov 2006;8(6):393–400.
- Colman I, Friedman BW, Brown MD, et al. Parenteral dexamethasone for acute severe migraine headache: meta-analysis of randomised controlled trials for preventing recurrence. BMJ 2008; 336:1359.
- Singh A, Alter HJ, Zaia B. Does the addition of dexamethasone to standard therapy for acute migraine headache decrease the incidence of recurrent headache for patients treated in the emergency department? A meta-analysis and systematic review of the literature. Acad Emerg Med 2008; 15:1223.
- Sumamo Schellenberg E, Dryden DM, Pasichnyk D, et al. Acute migraine treatment in emergency settings. Agency for Healthcare Research and Quality. www.ncbi.nlm.nih.gov/books/NBK115368/ (Accessed on September 30, 2013).
- Friedman BW, Cabral L, Adewunmi V, et al. Diphenhydramine as adjuvant therapy for acute migraine: an emergency department–based randomized clinical trial. Ann Emerg Med. 2016;67:32-39.
- Gazerani P, Pourpak Z, Ahmadiani A, Hemmati A, Kazemnejad A. A Correlation between Migraine, Histamine and Immunoglobulin E. Iran J Allergy Asthma Immunol. 2003;2:17–24.
- Aamodt AH, Stovner LJ, Langhammer A, Hagen K, Zwart JA. Is headache related to asthma, hay fever, and chronic bronchitis? The Head-HUNT Study. 2007;47:204–12.
- Ku M, Silverman B, Prifti N, Ying W, Persaud Y, Schneider A. Prevalence of migraine headaches in patients with allergic rhinitis.Ann Allergy Asthma Immunol. 2006;97:226–30.
- Gupta S, Nahas SJ, Peterlin BL. Chemical mediators of migraine: preclinical and clinical observations. 2011;51:1029–45.
- Balbin JEB, Nerenberg R, Baratloo A. Intravenous fluids for migraine: a post hoc analysis of clinical trial data. 2016;34(4):713-716.
- Obermann M, Holle D, Naegel S, et al. Pharmacotherapy options for cluster headache. Expert Opin Pharmacother 2015; 16:1177.
- May A, Leone M, Afra J, et al. EFNS guidelines on the treatment of cluster headache and other trigeminal-autonomic cephalalgias. Eur J Neurol 2006; 13:1066.
- Leniger T, Pageler L, Stude P, et al. Comparison of intravenous valproate with intravenous lysine-acetylsalicylic acid in acute migraine attacks. 2005;45(1):42-46.
- Tanen DA, Miller S, French T, Riffenburgh RH. Intravenous sodium valproate versus prochlorperazine for the emergency department treatment of acute migraine headaches: a prospective, randomized, double-blind trial. Ann Emerg Med. 2003; 41(6):847–853.
- Foroughipour M, Ghandehari K, Khazaei M, et al. Randomized clinical trial of intravenous valproate (orifil) and dexamethasone in patients with migraine disorder. Iran J Med Sci. 2013;38:150-155.
- Shahien R, Saleh SA, Bowirrat A. Intravenous sodium valproate aborts migraine headaches rapidly. Acta Neurol Scand. 2011; 123(4):257–265.
- Edwards KR, Norton J, Behnke M. Comparison of intravenous valproate versus intramuscular dihydroergotamine and metoclopramide for acute treatment of migraine headache. Headache. 2001;41(10):976–980.
- Hering R, Steiner TJ. Sodium valproate for acute migraine Cephalalgia. 1994;14(4):305–306.
- Mathew NT, Kailasam J, Meadors L, Chernyschev O, Gentry P. Intravenous valproate sodium (depacon) aborts migraine rapidly: a preliminary report. Headache. 2000;40(9):720–723.
- Soleimanpour H,Ghafouri RR, Taheraghdam A, et al. Effectiveness of intravenous dexamethasone versus propofol for pain relief in the migraine headache: a prospective double blind randomized clinical trial. BMC Neurol. 2012 Sep 29;12:114.
- Soleimanpour H, Taheraghdam A, Ghafouri R, et al. Improvement of refractory migraine headache by propofol: case series.Int J Emerg Med. 2012;5(1):19.
- Moshtaghion H, Heiranizadeh N, Rahimdel A, et al. The Efficacy of Propofol vs. Subcutaneous Sumatriptan for Treatment of Acute Migraine Headaches in the Emergency Department: A Double-Blinded Clinical Trial.Pain Pract. 2015;15(8):701-705.
- Gorlin AW, Rosenfeld DM, Ramakrishna H. Intravenous sub-anesthetic ketamine for perioperative analgesia. J Anaesthesiol Clin Pharmacol 2016;32(2):160–7.
- Kurdi MS, Theerth KA, Deva RS. Ketamine: current applications in anesthesia, pain, and critical care. Anesth Essays Res 2014;8(3):283–9.
- Beaudoin FL,Lin C, Guan W, Merchant RC. Low-dose ketamine improves pain relief in patients receiving intravenous opioids for acute pain in the emergency department: results of a randomized, double-blind, clinical trial. Acad Emerg Med. 2014 Nov;21(11):1193-202.
- Nicolodi M, Sicuteri F. Exploration of NMDA receptors in migraine: therapeutic and theoretic implications. Int J Clin Pharmacol Res. 1995;15(5-6):181-189.
- Lauritsen C, Mazuera S, Lipton RB, et al. Intravenous ketamine for subacute treatment of refractory chronic migraine: a case series. The Journal of Headache and Pain. 2016;17:106.
- Motov S,Mai M, Pushkar I, et al. A prospective randomized, double-dummy trial comparing IV push low dose ketamine to short infusion of low dose ketamine for treatment of pain in the ED. Am J Emerg Med. 2017 Aug;35(8):1095-1100.
- Corbo J, Esses D, Bijur P, et al. Randomized clinical trial of intravenous magnesium sulfate as an adjunctive medication for emergency department treatment of migraine headache.Ann Emerg Med. 2001;38(6):621-627.
- Shahrami A, Assarzadegan F, Hatamabadi H, et al. Comparison of therapeutic effects of magnesium sulfate vs. dexamethasone/metoclopramide on alleviating acute migraine headache.J Emerg Med. 2015;48(1):69-76.
- Cete Y, Dora B, Ertan C, et al. A randomized prospective placebo-controlled study of intravenous magnesium sulphate vs. metoclopramide in the management of acute migraine attacks in the Emergency Department. 2005;25(3):199-204.
- Bigal M, Bordini C, Tepper S, Speciali J. Intravenous magnesium sulphate in the acute treatment of migraine without aura and migraine with aura. A randomized, double-blind, placebo-controlled study. 2002;22(5):345-353.
- Mellick LB,McIlrath ST, Mellick GA. Treatment of headaches in the ED with lower cervical intramuscular bupivacaine injections: a 1-year retrospective review of 417 patients. 2006 Oct;46(9):1441-9.
- Ashkenazi A, Levin M. Greater occipital nerve block for migraine and other headaches: Is it useful? Current Pain and Headache Reports 2007;11(3):231-235.
- Maizels M, Scott B, Cohen W, Chen W. Intranasal lidocaine for treatment of migraine: a randomized, double-blind, controlled trial. JAMA. 1996;276(4):319-321.
- Schaffer J, Hunter B, Ball K, Weaver C. Noninvasive sphenopalatine ganglion block for acute headache in the emergency department: a randomized placebo-controlled trial. Ann Emerg Med. 2015;65(5):503-510.
- Cady R, Saper J, Dexter K, Manley H. A double-blind, placebo-controlled study of repetitive transnasal sphenopalatine ganglion blockade with tx360(®) as acute treatment for chronic migraine. Headache. 2015;55(1):101-116.
- Robbins L. Intranasal lidocaine for cluster headache. Headache. 1995:35:83.
- Morgan A, Jessop V. Best BETs from the Manchester Royal Infirmary. BET 2: should intranasal lidocaine be used in patients with acute cluster headache? Emerg Med J 2013; 30:769.
- Costa A, Pucci E, Antonaci F, et al. The effect of intranasal cocaine and lidocaine on nitroglycerin-induced attacks in cluster headache. Cephalalgia 2000; 20:85.
- Hardebo JE, Elner A. Nerves and vessels in the pterygopalatine fossa and symptoms of cluster headache. Headache 1987; 27:528.
- Kittrelle JP, Grouse DS, Seybold ME. Cluster headache. Local anesthetic abortive agents. Arch Neurol 1985; 42:496.
- Langer-Gould A, Anderson W, Armstrong M, et al. The American Academy of Neurology’s top five choosing wisely recommendations. 2013;81(11):1004-1011.
- Loder E, Weizenbaum E, Frishberg B, et al. Choosing wisely in headache medicine: the American Headache Society’s list of five things physicians and patients should question. 2013;53(10):1651-1659.
- Bigal ME, Rapoport AM, Lipton RB, et al. Assessment of migraine disability using the migraine disability assessment (MIDAS) questionnaire: a comparison of chronic migraine with episodic migraine. Headache. 2003;43(4): 336–342.
- Silberstein SD, Olesen J, Bousser MG, et al. The international classification of headache disorders, 2nd Edition (ICHD-II)—revision of criteria for 8.2 Medication-overuse headache. Cephalalgia. 2005;25(6):460–465.
- Dodick D, Freitag F. Evidence-based understanding of medication-overuse headache: clinical implications. Headache. 2006;46(suppl 4):S202–S211.
- Bigal M, Serrano D, Buse D, et al. Acute migraine medications and evolution from episodic to chronic migraine: a longitudinal population-based study. 2008;48(8):1157-1168.
- Colman I, Rothney A, Wright S, et al. Use of narcotic analgesics in the emergency department treatment of migraine headache. 2004;62(10):1695-1700.
- Burstein R, Collins B, Jakubowski M. Defeating migraine pain with triptans: a race against the development of cutaneous allodynia.Ann Neurol. 2004;55(1):19-26.
- Friedman B, Kapoor A, Friedman M, et al. The relative efficacy of meperidine for the treatment of acute migraine: a meta-analysis of randomized controlled trials.Ann Emerg Med. 2008;52(6):705-713.
- Ho TW, Rodgers A, Bigal ME. Impact of recent prior opioid use on rizatriptan efficacy. A post hoc pooled analysis. Headache. 2009;49(3):395–403.
- Buse DC, Pearlman SH, Serrano D, et al. Rates of opioid use and dependence by sociodemographics, medical and psychiatric comorbidities, and headache-related disability among persons with Episodic Migraine (EM) in the US population: results of the American Migraine Prevalence and Prevention (AMPP) study. Headache. 2011;51:48.
- Lewis D, Middlebrook MT, Deline C. Naproxen sodium for chemoprophylaxis of adolescent migraine. Ann Neurol. 1994;36:542.
- Bellavance AJ, Meloche JP. A comparative study of naproxen sodium, pizotyline and placebo in migraine prophylaxis. 1990;30(11):710–715.
- Welch KM, Ellis DJ, Keenan PA. Successful migraine prophylaxis with naproxen sodium. Neurology. 1985;35(9): 1304–1310.
- Sargent J, Solbach P, Damasio H, et al. A comparison of naproxen sodium to propranolol hydrochloride and a placebo control for the prophylaxis of migraine headache. Headache. 1985;25(6):320–324.
- Ziegler DK, Ellis DJ. Naproxen in prophylaxis of migraine. Arch Neurol. 1985;42(6):582–584.
- Bigal ME, Lipton RB. Excessive acute migraine medication use and migraine progression. Neurology. 2008;71(22): 1821–1828.
- Motov S, Yasavolian M, Likourezos A, et al. Comparison of Intravenous Ketorolac at Three Single-Dose Regimens for Treating Acute Pain in the Emergency Department: A Randomized Controlled Trial. Ann Emerg Med.2017 Aug;70(2):177-184.
- Moore RA, Wiffen PJ, Derry S, et al. Non-prescription (OTC) oral analgesics for acute pain – an overview of Cochrane reviews. Cochrane Database Syst Rev. 2015 Nov 4;(11):CD010794.









6 thoughts on “emDocs Cases: Headache Management in the ED”
An excellent summary! As you point out, in the “headache cocktail” the anti-dopaminergic agents seem to do the heavy lifting in relieving symptoms in all types of headaches. I do have some issue with the evidence that says that adding anti-histamines to the migraine cocktail does not have an affect on subsequent akathisia or other EPS side effects. I certainly believe that benadryl does not improve pain, but in my practice when I stopped giving benadryl with compazine, everyone seemed to get akathisia! I know, anecdotal, but I still give compazine + benadryl (plus decadron if classic migraine).
Pingback: emDOCs.net – Emergency Medicine EducationPain Profiles: Prochlorperazine versus Ketamine for Headache - emDOCs.net - Emergency Medicine Education
Pingback: emDOCs.net – Emergency Medicine EducationPain Profiles: ED Migraine Management - The New Kid on the “Block” - emDOCs.net - Emergency Medicine Education
Pingback: Headache – Emergency medicine tidbits
Pingback: March 18th Didactics – Lakeland Health EM Blog
Pingback: Beyond the Bleed: Acute Hydrocephalus as a Cause of Headache - JEMS