Here’s another case from Medical Malpractice Insights – Learning from Lawsuits, a monthly email newsletter for ED physicians. The goal of MMI-LFL is to improve patient safety, educate physicians and reduce the cost and stress of medical malpractice lawsuits. To opt in to the free subscriber list, click here.
Chuck Pilcher MD FACEP
Editor, Med Mal Insights
Chest pain, a widened mediastinum, and a discordant CT
What if the radiologist is wrong?
Facts: A 77-year-old obese male (BMI 43) calls 911 from a restaurant when he develops 9/10 chest pain radiating to his right shoulder and jaw with diaphoresis. The pain is dull but occasionally sharp and decreases to 2/10 during transport to the hospital. His past history includes a cardiac bypass 35 years ago and stents 5 years ago. Blood pressure in the ED is initially 100/65 mm Hg but dips as low as 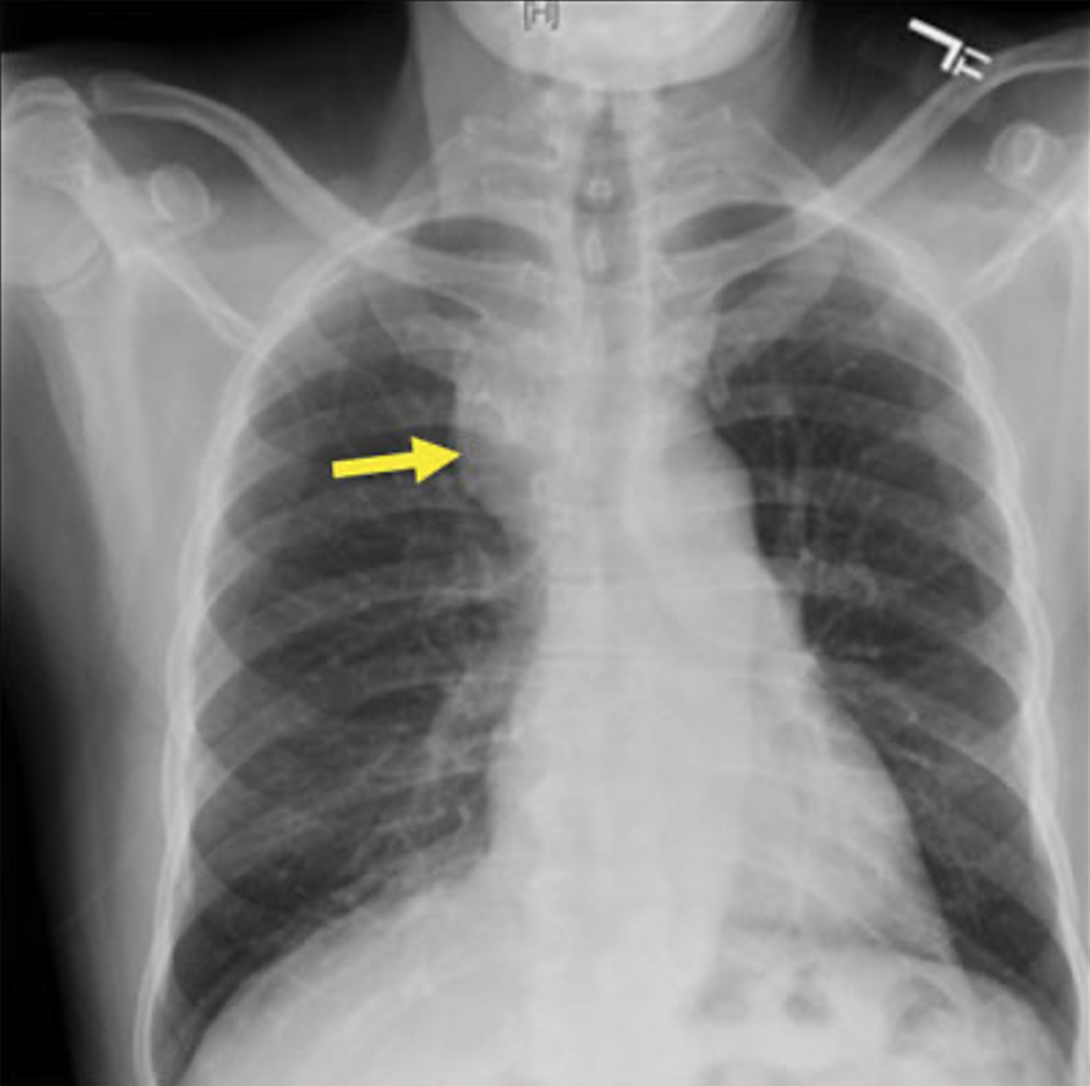 74/50. Lab and EKG are unremarkable except for sinus bradycardia. Chest x-ray shows a very wide mediastinum [image is illustrative only]. A non-contrast CT scan is interpreted by a telemetry service as showing a RUL mediastinal mass “likely due to cancer, no vascular abnormality.” The patient is admitted as “Chest Pain – Acute” for further evaluation and possible biopsy of the undefined RUL mass. No differential diagnosis is recorded, nor is there any mention of possible thoracic aortic aneurysm. He is given 40 mg low molecular weight heparin (LMWH) for DVT prophylaxis. The next morning an in-hospital radiologist over-reads the CT scan as a “leaking aortic aneurysm with mediastinal hematoma.” The patient is transferred to a higher level of care, is taken to the OR for an endovascular repair, but dies in surgery. The family consults an attorney, and a lawsuit is filed against the ED physician, virtual radiologist, hospitalist, and others.
74/50. Lab and EKG are unremarkable except for sinus bradycardia. Chest x-ray shows a very wide mediastinum [image is illustrative only]. A non-contrast CT scan is interpreted by a telemetry service as showing a RUL mediastinal mass “likely due to cancer, no vascular abnormality.” The patient is admitted as “Chest Pain – Acute” for further evaluation and possible biopsy of the undefined RUL mass. No differential diagnosis is recorded, nor is there any mention of possible thoracic aortic aneurysm. He is given 40 mg low molecular weight heparin (LMWH) for DVT prophylaxis. The next morning an in-hospital radiologist over-reads the CT scan as a “leaking aortic aneurysm with mediastinal hematoma.” The patient is transferred to a higher level of care, is taken to the OR for an endovascular repair, but dies in surgery. The family consults an attorney, and a lawsuit is filed against the ED physician, virtual radiologist, hospitalist, and others.
Plaintiff:
- RE the first radiologist: You misread my CT scan.
- RE the ED physician: You saw the wide mediastinum on the CXR and apparently thought of thoracic aortic aneurysm but didn’t question the radiologist’s CT report.
- RE subsequent caregivers: You relied on the radiologist’s report and the ED physician’s “diagnosis” despite the fact that the history sounded nothing like a malignancy. You all delayed care that could have saved my life,= and complicated it by giving me LMWH.
Defense:
- Only the nightshift radiologist is responsible. We would have transferred you earlier if he had read the CT scan correctly.
- Your LAD was already fully occluded, your RCA was 60-70% occluded, and your circumflex artery was diffusely narrowed. You would not have survived the surgery anyway.
Result:
- Pre-trial settlement for undisclosed amount apportioned in undisclosed percentages amongst the various defendants.
Takeaways:
- Missed aortic dissection is one of the top causes of medical malpractice lawsuits. Always consider it in chest pain patients.
- The chest x-ray showed a textbook image of a widened mediastinum consistent with a thoracic aortic dissection.
- When we order a study to evaluate for a specific condition, the radiologist deserves some useful information. Why this study? What am I concerned about? Sudden onset of 9/10 chest pain should lead a radiologist to think differently.
- Failure of the EP to recognize the discordance between the patient’s history and the CT report should lead to a conversation with the radiologist.
- If uncertain, challenge the reading. Because we have clinical context, we occasionally find things on the images we order that radiologists miss – or conversely over-read. Each of us will cause a radiologist to amend or correct a report at some point in our careers (Feels good, doesn’t it?).
- Document conversations with consultants.
- When we eliminate a diagnosis from our differential, explain why. It then becomes a judgment call, not negligence.
- This case is an example of “Authority Bias,” deferring to or declining to disagree with an “expert.”
- In summary, remember that YOU are sometimes the expert. You have the patient, the history, the exam – the whole package. A distant consultant may only be looking at data. Give them some help.
References:
- Aortic dissection. emDocs.net. http://www.emdocs.net/aortic-dissection-why-do-we-miss-it-how-to-improve/
- Carotid artery dissection. Zohrabian D. Medscape eMedicine. Updated Feb. 19, 2019. medscape.com/article/757906-overview
- Aortic dissection. Mancini MC. Medscape eMedicine. Updated Jul 24, 2020. medscape.com/article/2062452-overview








