Author: Sarah Brubaker, MD (EM Resident Physician, San Antonio, TX) // Edited by: Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit); and Tim Montrief (@EMinMiami)
Case
A 45-year-old woman presents to the emergency department with the chief complaint of “fever.” She has noted an intermittent fever for the last 2 weeks, with a maximum temperature of 103°F. She denies other symptoms. She was recently started on phenytoin for a newly-diagnosed seizure disorder, but she denies other medical history and she takes no other medications. Upon presentation, her vital signs are BP 118/72, HR 77, RR 14, SpO2 100%, T 102.2°F. Her exam is normal. Because this fever has been intermittent for several weeks, you think to yourself, “How should I approach this patient? Since her fever has lasted for 2 weeks without other symptoms, could there be a non-infectious cause? What pathologies cause non-infectious fever?”
When a patient presents to the emergency department with a chief complaint of fever, most providers initially presume an infective etiology. This is a reasonable assumption, as the majority of fevers are caused by infection [1, 2]. However, this assumption is flawed for several reasons. First, the presence or absence of fever is not reliably sensitive or specific in detecting the presence of an infection. In a study of pediatric patients, fever (temperature >100.4°F ) was only 67% sensitive and 45% specific in detecting serious bacterial infection [3]. In addition, there are myriad non-infectious causes of fever that can be life-threatening if not identified and treated quickly. Therefore, it is important to keep a broad differential when evaluating a febrile patient and investigate further if there is not an apparent infection.
This article will begin with a basic review of the pathophysiology of fever, which will lay the groundwork for understanding the various causes of non-infectious fever. We will then discuss the most common etiologies, with the goal of creating a practical differential diagnosis for non-infectious fever.
Pathophysiology
The definition of fever has not been universally established, but many providers define a fever as any temperature greater than 38°C (100.4°F) [2]. Temperature is regulated by the hypothalamus, which has a “regulatory set point between 36.5-37.5°C (98-100°F)”[4]. Various insults to the body can cause the hypothalamus to increase the regulatory set point. For example, in infectious processes, various pyrogens (e.g. viruses and bacteria) lead to the release of cytokines, which up-regulate prostaglandins, activating the hypothalamus to increase its temperature set-point [2, 4]. Cytokines can also be released in response to non-infectious inflammatory states, such as neoplastic and autoimmune processes, which can result in a non-infectious fever. A non-infectious fever can also be due to malfunction of the hypothalamus itself (“central fever”) as a result of stroke, trauma, or other intracranial processes [5].
Hyperpyrexia, defined as a temperature greater than 41°C (105.8°F) [2], is an independent predictor of high mortality. In addition, it is more likely to represent non-infectious causes compared to a traditional fever[6]. Therefore, the presence of hyperpyrexia should increase suspicion for non-infectious causes of fever.
Causes of non-infectious fever
The research is sparse regarding the prevalence of different etiologies of acute fever. However, there is robust research regarding fever of unknown origin (FUO), defined as fever greater than 101°F on more than 3 occasions for 3 weeks or longer in an immunocompetent patient without diagnosis despite prior workup [6, 7]. Several prospective studies have evaluated causes of FUO [6-10]. In 2012, a meta-analysis of these studies found that most FUO are caused by infection (14-53%), followed by non-infectious inflammatory disease (2-36%), malignancy (8-19%), miscellaneous (including thyroiditis, drug fever, pulmonary embolism) (0-18%), and unknown (7-42%) [11]. In a prospective review of 290 patients, investigators found non-infectious inflammatory diseases to be the most common cause of FUO (35%), followed by infection (30%) and malignancy (15%) [10]. The patients in these studies were in an inpatient setting for evaluation of FUO and had already received an outpatient workup, so there are several caveats to generalizing this data, especially in the setting of emergency medicine. However, the results highlight the prevalence of non-infectious fever and the importance of knowing its potential causes. Although it is not all-inclusive, Table 1 lists the most important potential etiologies of non-infectious fever.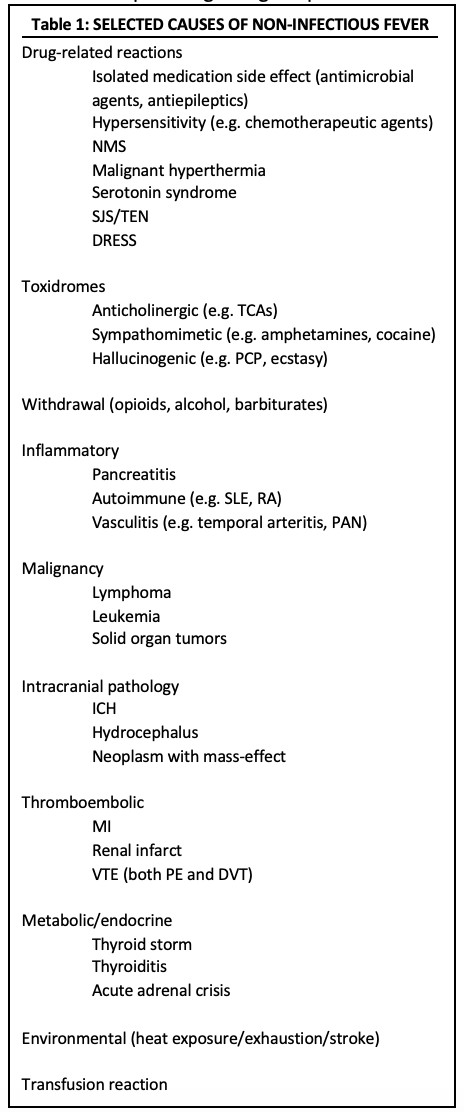
Drug and toxin-related
Medications can lead to temperature changes (both hypo- and hyperthermia), especially in chronically ill patients with polypharmacy [1]. This can occur as a result of hypersensitivity, adverse effects at therapeutic levels, overdose, and withdrawal. For example, several chemotherapeutic agents are well known to cause a hypersensitivity reaction (most commonly the taxanes, which includes paclitaxel and docetaxel [12]), resulting in the release of pyrogens that leads to an isolated fever [13]. This reaction has also been described after administration of several antiepileptic agents, either as part of drug reaction with eosinophilia and systemic symptoms (DRESS) or as an isolated hypersensitivity reaction. The most common offending antiepileptic medications are carbamazepine, lamotrigine, and phenytoin [14-17]. Some medications result in increased metabolism (e.g. thyroxine) or altered temperature control (e.g. antihistamines, dopaminergic medications such as carbidopa), and therefore hyperthermia may be present in both therapeutic and supratherapeutic doses. Antimicrobial agents (most commonly beta-lactams and sulfonamides), procainamide, and intravenous potassium chloride are examples of common agents that may result in fever [1], although these are only a few examples of the numerous medications that can have this effect. The fever may occur immediately after administration, but it can also manifest several days after ingestion, and persist for up to a week after removal of the offending agent [11].
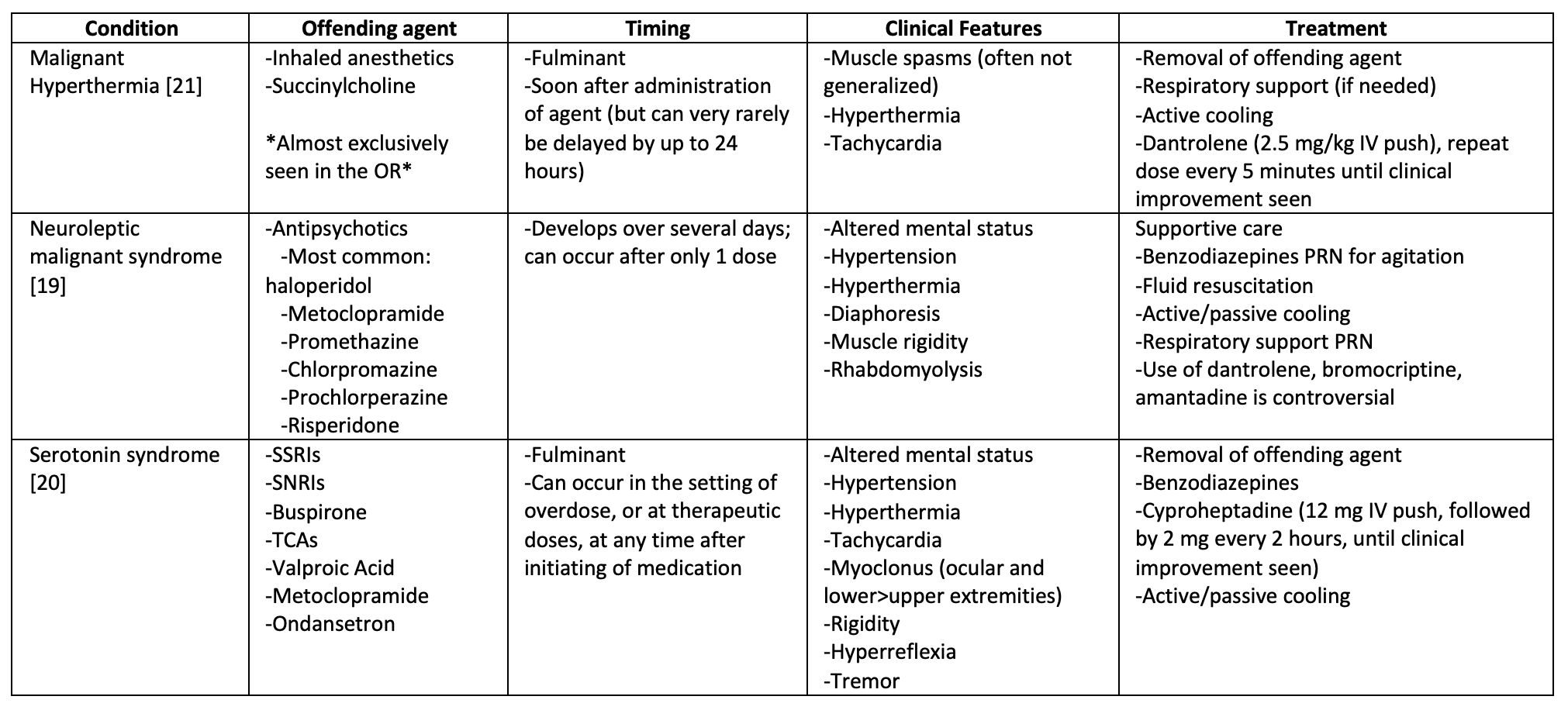
Most drug-related fevers are benign. However, three drug-based syndromes associated with hyperthermia confer high morbidity and mortality: malignant hyperthermia, neuroleptic malignant syndrome (NMS), and serotonin syndrome. You should maintain high suspicion for these syndromes in any patient with hyperpyrexia. All three are characterized by autonomic instability and muscular rigidity, but there are important distinguishing features and treatments, which are described in Table 2. When you are trying to distinguish between NMS and serotonin syndrome, remember that although both cause rigidity, NMS is characterized by “lead-pipe rigidity” (muscular stiffness that is consistently present, even with passive range of motion), while serotonin syndrome is characterized by lower extremity clonus and tremors. In addition, serotonin syndrome is usually more fulminant than NMS, with symptoms developing over several hours (compared to several days for NMS) [18-20].
Overdose and withdrawal syndromes often manifest with fever. For example, the anticholinergic toxidrome (e.g. diphenhydramine or TCA overdose) is characterized by fever, tachycardia, altered mental status, anhidrosis, flushing, and urinary retention. The sympathomimetic toxidrome (e.g. cocaine ingestion, amphetamine overdose) is characterized by fever, tachycardia, altered mental status, and diaphoresis. Several hallucinogens (e.g. PCP, ketamine, or ecstasy) contain sympathomimetic components, in addition to serotonergic effects; therefore, the hallucinogenic toxidrome often involves hyperthermia in addition to behavioral changes (euphoria and/or agitation), hypertension, tachycardia, and seizures. Fever is also common in withdrawal syndromes. Benzodiazepine, barbiturate alcohol, and opioid withdrawal can lead to substantial hyperthermia, often in addition to tachycardia, diaphoresis, and agitation [1]. All of these syndromes are associated with morbidity and mortality if not appropriately recognized and treated.
Non-infectious inflammatory diseases
Non-infectious inflammatory diseases (NIID) are responsible for up to 35% of FUO [10, 22]. NIID can further be divided into autoimmune disease (e.g. rheumatoid arthritis, Sjogren syndrome, systemic lupus erythematosus, polymyalgia rheumatica), vasculitis (e.g. temporal arteritis, polyarteritis nodosa), and granulomatous disorders (e.g. sarcoidosis). If you suspect a first-time diagnosis of these conditions, you may choose to initiate a workup (including ANA, rheumatoid factor, ESR, CRP)[2], but often these conditions can be further evaluated in an outpatient setting.
In addition, in patients with known NIID, it is important to note that although flares may present with fever, patients with chronic inflammatory conditions are often immunocompromised, and clinicians should assess for and consider infection before assuming a non-infectious fever [23]. This often includes a diligent search for a source of infection, in addition to CRP, ESR, and sometimes procalcitonin [24]. However, the use of these tests is controversial. Emerging literature suggests high procalcitonin may be a specific indicator of bacterial infection [25], while ESR and CRP likely lack the specificity to reliably distinguish between inflammatory and infectious disease processes [26]. However, use of procalcitonin in the ED for exclusion of infection requires further study.
Malignancy
In studies concerning FUO, hematologic cancers were the most common neoplastic cause of fever [9, 10], predominantly lymphoma (both Hodgkin’s and non-Hodgkin’s). Solid tumors can cause fever as well, with lung cancer being the most common. You may suspect a neoplastic etiology if the patient reports recurrent fever, night sweats, and gradual weight loss (“B symptoms”) [27].
Intracranial pathology
Thermoregulatory abnormalities are well-known entities in patients with intracranial pathology; up to 70% of patients in the neurologic intensive care unit become febrile during their hospitalization [5]. However, less than half of these fevers are caused by infection. There are several proposed mechanisms for central fever, but most of the pathophysiology ultimately results from an insult to the hypothalamus. For example, hydrocephalus or large intracranial neoplasms can place physical pressure on the hypothalamus; blood acts as an irritant, and its presence in the basal cisterns can lead to increased body temperature. Patients with ischemic or hemorrhagic damage to the hypothalamus may experience primary dysfunction [28, 29].
Fever is common in patients with aneurysmal subarachnoid hemorrhage (SAH). In one prospective cohort study of 194 patients with SAH, 43% of patients developed a fever within the first 4 days of admission. Of these, 34% were infectious (as demonstrated by positive blood, urine, CSF, or sputum culture) and 9% were noninfectious. The study found intraventricular blood to be an independent risk factor for the development of fever [29]. However, non-infectious fever was rare, and the authors stressed the importance of evaluating for infectious causes before assuming a non-infectious cause. Central fever should only be considered AFTER infection and other non-infectious causes of fever have been excluded, such as drug administration or withdrawal, venous thromboembolism, and blood transfusion reactions [5].
Thromboembolic
Fevers may be a part of the symptomatology of thromboembolic diseases (e.g. myocardial infarction, deep venous thrombosis (DVT), and pulmonary embolism (PE)). The exact cause is unknown, but they likely lead to generalized inflammation and cytokine release, increasing the hypothalamic set point. Fevers are generally low-grade (<38.3C) and last for one day or less [30]. Nonetheless, fever may be present in up to 9% of patients with DVT [31]. In a large, multicenter, prospective analysis of 14,480 patients admitted with acute DVT, 4.9% of patients had fever upon presentation. These patients had increased mortality (5.8% vs. 2.9%) compared to those without a fever [32]. According to the same study, “this worse outcome persisted after multivariate adjustment, and was mostly due to an increased incidence of fatal PE or infection.”
Fever is present in up to 50% of patients with PE [33, 34]. The PIOPED study (a retrospective chart-review of 311 patients hospitalized for newly diagnosed pulmonary embolism) found that fever (>37.5 C) was present in 50% of patients with acute PE; the majority of fevers were caused by alternate causes (e.g. infection, malignancy), but 14% of PEs were associated with fever without any other identifiable cause [33]. Although it has not been well-studied, the literature does not reliably indicate worsened outcomes with febrile PEs [30, 34, 35]. However, in a retrospective study of 241 patients admitted for acute PE, “patients in PE with fever group were more likely to require intensive care admission (69.5% vs 35.7%), had a longer hospital length of stay (19.80 vs 12.20 days) and higher requirement of mechanical ventilation (30.5% vs 6.6%) compared with those without fever. PE with fever group were more likely to have massive and submassive PE (55.9% vs 36.8%) and had higher incidence of deep vein thrombosis (33.3% vs 17.4%) compared with PE without fever” [36].
Because high fever (>39C) is rare in PE [30], and because concomitant infection and/or malignancy is common, it is important to look for alternate sources in febrile patients with PEs, especially if the fever is >39. For example, it is important to consider sources for septic emboli, such as right-sided infective endocarditis, infected central venous catheter, or septic internal jugular thrombophlebitis (Lemierre’s syndrome).
Endocrine/Metabolic
Unlike most of the conditions described above, which reset the hypothalamic set-point, endocrine disorders lead to fever because they increase metabolic demand [37]. The two most important endocrinopathies that may cause fever are thyroid storm and adrenal insufficiency.
Thyrotoxicosis is the constellation of symptoms caused by the overproduction (or over-ingestion) of thyroid hormones. It is characterized by fever, heat intolerance, sweating, tremor, palpitations, nervousness, fatigue, weight loss, diarrhea, tachycardia, hypertension (with wide pulse-pressure), lid retraction, hyperreflexia, and increased cardiac output. Thyroid storm can be considered end-stage thyrotoxicosis; in addition to the symptoms above, patients may experience hyperpyrexia, delirium, and high-output cardiac failure. Mortality is 20-30%, and patients with thyroid storm require aggressive treatment in the emergency department, followed by admission to a medical ICU [37]. The most common precipitating cause of thyroid storm is infection, so have a low threshold to empirically treat with antibiotics. Thyroid storm is complex condition that requires nuanced management; it is discussed in more detail here: http://www.emdocs.net/thyroid-storm-management/.
Adrenal insufficiency is the inability of the adrenal glands to produce glucocorticoids (e.g. cortisol) and aldosterone [37]. Glucocorticoid deficiency leads to hypotension and hypoglycemia; aldosterone deficiency leads to hyponatremia and hyperkalemia. These deficiencies lead to orthostatic hypotension, confusion, abdominal pain, nausea, vomiting, diarrhea, and fever. Because these symptoms are vague, this diagnosis is often overlooked. In extreme cases, patients can present with distributive shock. Therefore, it is important to consider adrenal insufficiency in patients with persistent hypotension despite adequate fluid resuscitation and initiation of vasopressors; these patients are likely glucocorticoid deficient and will improve with steroid administration (e.g. 100 mg IV hydrocortisone). In addition, these patients are often persistently hypoglycemic, so consider adding glucose to your fluids-of-choice during resuscitation.
Of note, because these patients have a blunted stress-response, they are often functionally immunocompromised [37]. Therefore, have a low threshold to administer empiric antibiotics. For an overview of acute adrenal insufficiency: http://www.emdocs.net/em3am-acute-adrenal-insufficiency/.
Conclusion
In addition to medication effects, toxicity, inflammatory processes, malignancy, intracranial pathology, thromboembolism, and metabolic derangements, there are several important sources of non-infectious fever not described above. Unfortunately, there are so many causes of non-infectious fever that a single article cannot reasonably describe each cause in depth. For example, fever may be present (generally as part of a larger clinical picture) in patients with environmental exposure (e.g. heat exhaustion, heat stroke), transplant rejection (both acute and chronic), and acute transfusion reaction. However, this article should provide as a sufficient starting-point for keeping a broad differential when considering non-infectious etiologies of fever.
For the patient who presented at the beginning of this article, a thorough investigation was performed to evaluate for infection, toxic ingestion, malignancy, autoimmune conditions, thromboembolic disease, intracranial pathology, thyrotoxicosis, adrenal insufficiency. After all of these processes were excluded, the only possible source of infection was the patient’s use of phenytoin, which is known to cause non-infectious fever. After follow-up with her neurologist, the patient switched her anti-epileptic from phenytoin to levetiracetam; her fever resolved within 1 week of cessation.
Summary
–Most fevers are caused by infection. However, in fever of unknown origin, up to 70% of fevers have non-infectious etiology [10].
-Some common medications that can cause fever: beta-lactam antibiotics, antiepileptics (phenytoin, carbamazepine), chemotherapeutic agents (paclitaxel, docetaxel), thyroxine.
–Toxidromes with fever: anticholinergic, sympathomimetic, hallucinogenic.
–Withdrawal syndromes with fever: alcohol, opioid, and barbiturate.
–NMS (most common offending agent: 1st generation antipsychotics) and serotonin syndrome are associated with high mortality; have high suspicion for these diagnoses in patients with hyperpyrexia (temperature greater than 41°C (105.8°F)).
-Workup for autoimmune disease can often be deferred to the outpatient setting; patients with known chronic inflammatory conditions are often immunocompromised, and infection must be ruled out before assuming a non-infectious fever.
-“B symptoms” (fever, night sweats, weight loss) may indicate the presence of a neoplastic process; hematologic cancers (both lymphoma and leukemia) are more likely to cause fever than solid cancers.
-Although infectious causes must be excluded first, non-infectious fevers are common in patients with intracranial pathology (hemorrhage, ischemia, hydrocephalus).
–Thyroid storm and adrenal insufficiency are two metabolic conditions that can lead to fever. They have very high morbidity and mortality when they are not promptly recognized. They often co-occur with infective processes, so have a low threshold to administer antibiotics.
-Other possible causes: environmental exposure (e.g. heat exhaustion, heat stroke), as well as thromboembolism (e.g. myocardial infarction, deep venous thrombosis, pulmonary embolism).
-In the correct setting, fever can also be caused by transplant rejection (both acute and chronic) as well as transfusion reaction.
References/Further Reading
- O’Grady, N.P., et al., Guidelines for evaluation of new fever in critically ill adult patients: 2008 update from the American College of Critical Care Medicine and the Infectious Diseases Society of America. Critical care medicine, 2008. 36(4): p. 1330-1349.
- Blum, F.C., Fever in the adult patient. Rosen’s emergency medicine: concepts and clinical practice, 2006: p. 134-138.
- De, S., et al., Lack of accuracy of body temperature for detecting serious bacterial infection in febrile episodes. The Pediatric infectious disease journal, 2015. 34(9): p. 940-944.
- Anochie, I.P., Mechanisms of fever in humans. International Journal of Microbiology and Immunology Research, 2013. 2(5): p. 037-043.
- Hocker, S.E., et al., Indicators of central fever in the neurologic intensive care unit. JAMA neurology, 2013. 70(12): p. 1499-1504.
- Bleeker-Rovers, C.P., et al., A prospective multicenter study on fever of unknown origin: the yield of a structured diagnostic protocol. Medicine, 2007. 86(1): p. 26-38.
- Knockaert, D., S. Vanderschueren, and D. Blockmans, Fever of unknown origin in adults: 40 years on. Journal of internal medicine, 2003. 253(3): p. 263-275.
- Efstathiou, S.P., et al., Fever of unknown origin: discrimination between infectious and non-infectious causes. European journal of internal medicine, 2010. 21(2): p. 137-143.
- Ergönül, Ö., et al., Revised definition of ‘fever of unknown origin’: limitations and opportunities. Journal of infection, 2005. 50(1): p. 1-5.
- Vanderschueren, S., et al., From prolonged febrile illness to fever of unknown origin: the challenge continues. Archives of internal medicine, 2003. 163(9): p. 1033-1041.
- Hayakawa, K., B. Ramasamy, and P.H. Chandrasekar, Fever of unknown origin: an evidence-based review. The American journal of the medical sciences, 2012. 344(4): p. 307-316.
- Baldo, B.A. and M. Pagani, Adverse events to nontargeted and targeted chemotherapeutic agents: emphasis on hypersensitivity responses. Immunology and Allergy Clinics, 2014. 34(3): p. 565-596.
- Niven, D.J. and K.B. Laupland, Pyrexia: aetiology in the ICU. Critical Care, 2016. 20(1): p. 247.
- Shear, N.H. and S.P. Spielberg, Anticonvulsant hypersensitivity syndrome. In vitro assessment of risk. The Journal of clinical investigation, 1988. 82(6): p. 1826-1832.
- Bakker, C.V., V.N. Hegt, and M.C. Van Praag, Lamotrigine hypersensitivity syndrome and spiking fever. Indian journal of dermatology, 2012. 57(6): p. 504.
- Mansur, A.T., Ş. Pekcan Yaşar, and F. Göktay, Anticonvulsant hypersensitivity syndrome: clinical and laboratory features. International journal of dermatology, 2008. 47(11): p. 1184-1189.
- Kano, Y. and T. Shiohara, The variable clinical picture of drug-induced hypersensitivity syndrome/drug rash with eosinophilia and systemic symptoms in relation to the eliciting drug. Immunology and allergy clinics of North America, 2009. 29(3): p. 481-501.
- Hiraga, A. and S. Kuwabara, Neuroleptic malignant syndrome and serotonin syndrome in general hospital settings: Clinical features, frequency and prognosis. Journal of the Neurological Sciences, 2017. 381: p. 606.
- Bottoni, T.N., Neuroleptic malignant syndrome: a brief review. Hospital Physician, 2002. 38(3): p. 58-63.
- Boyer, E.W. and M. Shannon, The serotonin syndrome. New England Journal of Medicine, 2005. 352(11): p. 1112-1120.
- Rosenberg, H., et al., Malignant hyperthermia: a review. Orphanet journal of rare diseases, 2015. 10(1): p. 93.
- Mulders-Manders, C., A. Simon, and C. Bleeker-Rovers, Rheumatologic diseases as the cause of fever of unknown origin. Best Practice & Research Clinical Rheumatology, 2016. 30(5): p. 789-801.
- Cuchacovich, R. and A. Gedalia, Pathophysiology and clinical spectrum of infections in systemic lupus erythematosus. Rheumatic Disease Clinics, 2009. 35(1): p. 75-93.
- Kim, H.-A., et al., C-reactive protein is a more sensitive and specific marker for diagnosing bacterial infections in systemic lupus erythematosus compared to S100A8/A9 and procalcitonin. The Journal of rheumatology, 2012: p. jrheum. 111044.
- Shaikh, M.M., L.E. Hermans, and J.M. Van Laar, Is serum procalcitonin measurement a useful addition to a rheumatologist’s repertoire? A review of its diagnostic role in systemic inflammatory diseases and joint infections. Rheumatology, 2014. 54(2): p. 231-240.
- Markanday, A. Acute phase reactants in infections: evidence-based review and a guide for clinicians. in Open forum infectious diseases. 2015. Oxford University Press.
- Diakos, C.I., et al., Cancer-related inflammation and treatment effectiveness. The Lancet Oncology, 2014. 15(11): p. e493-e503.
- Gijn, J.v., et al., Acute hydrocephalus after aneurysmal subarachnoid hemorrhage. Journal of neurosurgery, 1985. 63(3): p. 355-362.
- Dorhout Mees, S.M., et al., Fever after aneurysmal subarachnoid hemorrhage: relation with extent of hydrocephalus and amount of extravasated blood. Stroke, 2008. 39(7): p. 2141-2143.
- Nucifora, G., et al., Pulmonary embolism and fever: when should right-sided infective endocarditis be considered? Circulation, 2007. 115(6): p. e173-e176.
- Kazmers, A., H. Groehn, and C. Meeker, Do patients with acute deep vein thrombosis have fever? The American surgeon, 2000. 66(6): p. 598.
- Barba, R., et al., Fever and deep venous thrombosis. Findings from the RIETE registry. Journal of thrombosis and thrombolysis, 2011. 32(3): p. 288-292.
- Stein, P.D., et al., Fever in acute pulmonary embolism. Chest, 2000. 117(1): p. 39-42.
- Calvo-Romero, J.M., et al., Low-grade and high-grade fever at presentation of acute pulmonary embolism. Blood coagulation & fibrinolysis, 2004. 15(4): p. 331-333.
- Kokturk, N., et al., Fever in pulmonary embolism. Blood coagulation & fibrinolysis, 2005. 16(5): p. 341-347.
- Saad, M., et al., Fever is associated with higher morbidity and clot burden in patients with acute pulmonary embolism. BMJ open respiratory research, 2018. 5(1): p. e000327.
- Tenner, A.G. and K.M. Halvorson, Endocrine causes of dangerous fever. Emergency medicine clinics of North America, 2013. 31(4): p. 969.









6 thoughts on “Nuances to the Management of Febrile Patients: Non-Infectious Causes of Fever”
Pingback: Länkar v13-14 | Internmedicin
Pingback: Fever checks can't catch all Covid-19 cases. Smell tests might help
Pingback: Fever checks can’t catch all Covid-19 cases. Smell tests might help - Harmony
Pingback: Fever checks are a flawed way to flag Covid-19 cases; smell tests might help | Awesome Investors
Pingback: Fever checks are a flawed way to flag Covid-19 cases. Experts say smell tests might help – Salman Chughtai’s Laboratories
Pingback: OOR VUmc Regionaal onderwijs SEG 27 augustus 2020 – SPOEDZ Spoedeisende Geneeskunde Dijklander Ziekenhuis