Written by: David Cisewski, MD (@PainProfiles – EM Resident Physician, Icahn School of Medicine at Mount Sinai) // Edited by: Manpreet Singh, MD (@MPrizzleER), Alex Koyfman, MD (@EMHighAK), and Brit Long, MD (@long_brit)
This edition of Pain Profiles looks at a new review from Annals of Emergency Medicine on regional anesthesia.
Feeling Blocked? Another Pain Management Tool in the Emergency Department.
Wilson C. Annals Emerg Med. 2018;72(2):120-126.

In the midst of the current opioid dilemma, a discerning eye has been placed on how, when, and why we are using certain analgesics – particularly opioids. This has left emergency medicine providers with the responsibility to recognize the individual, subjective nature of each patient’s pain and to treat the pain in a safe and efficacious manner specific to a pain syndrome. As Dr. Wilson’s review suggests, ultra-sound guided nerve blocks have proven to be a safe, easy-to-learn analgesic alternatives used to treat a variety of pain presentations. This article will highlight the essential points of this must-read review.
What are the major advantages to nerve blocks?
Nerve blocks are a simple-to-learn, non-opioid analgesic technique that can result in improve ‘door-to-analgesia’ time (Johnson, 2014). Additionally, nerve blocks have demonstrated a reduction in ED length of stay by over 50% (Stone, 2008).
In which population are nerve blocks particularly useful?
Geriatrics! Femoral nerve blocks have been shown to be as effective as opioids for femoral fractures without the adverse effects of opioids seen among the elderly such as sedation, respiratory depression, and inpatient delirium (Haines, 2012; Beaudoin, 2013; Newton-Brown, 2014).
Why use ultrasound? Can’t I just eye-ball it?
This isn’t baseball; a .300 batting average isn’t going to make patients very happy. Approximately one-third of nerve blocks fail by landmark alone. This compares to a >95% success rate by using trained US-guidance (Perlas, 2008; Redborg, 2009; Sohoni, 2016). Additionally, US-guidance can limit the risk of major adverse events such as pneumothorax, intramuscular injection, and local anesthesia systemic toxicity (LAST) caused by an intravascular injection (Barrington, 2013).
Is there any pain presentation in which nerve blocks might not be ideal?
Pain, pallor, paresthesia, poikilothermia, pulselessness, paralysis. In patients with concern for compartment syndrome, nerve blocks can mask the early signs of development.
It seems so straightforward… Are there any major risks associated with nerve blocks?
Of course – you’re injecting a needle into tissue which includes, muscle, nerves, and blood vessels. Nerve blocks include an increased risk of infection, hematoma, nerve damage, and local anesthetic toxicity if an excess amount is injected directly into the blood stream. Side effects of local anesthetic toxicity include confusion, anxiety, sense of impending doom, headache, drowsiness, dizzy/lightheadedness, tremors as well as hemodynamic collapse, widened PR, QRS prolongation and eventual ventricular tachycardia, ventricular fibrillation, hypotension, and asystole (Jeng, 2010; Hasan, 2017). Seizures are treated with benzodiazepines (Sekimoto, 2017). Though rare, patients may develop local anesthesia systemic toxicity (LAST) secondary to direct injection of anesthetics into the vasculature. LAST can also result in cardiac toxicity including PR prolongation, bradycardia, and progression to hypotension, ventricular tachycardia, ventricular fibrillation, and ultimately asystole if severe (for a great review of LAST, see REBEL EM, May 2017 – Local Anesthetic Systemic Toxicity (LAST) or LITFL – Local Anesthetic Toxicity).
Treatment for LAST includes hemodynamic resuscitation efforts and the antidote – 20% solution 1.5 cc/kg bolus IV fat emulsion (intralipid) infused over one minute (Neal 2012, Cao 2015).
Okay, I’m feeling blocked – what supplies do I need for nerve block?
Dr. Wilson offers the following checklist from her review paper that is a perfect example to use for nerve block prep.

Okay, I have my supplies – time to block!
Not so fast – like all procedures, nerve blocks need a systemized pre-procedural protocol to maximize safety. Dr. Wilson offers a simple-to-use protocol for nerve blocks that should be used for every nerve block procedure. Identify the area of pain and review potential exclusion criteria such as coagulopathy, anesthesia allergies, history of neurologic deficiency, and obviously patient refusal. Always make sure that consent is obtained from patient and that a full neurologic exam is completed prior to the block. If a fracture is present and/or orthopedic intervention is required, make sure orthopedics is on board prior to blocking to ensure it doesn’t change their management. Have patient of a cardiac monitor to assess for systemic toxicity and know where lipid emulsion is available should it be necessary.
Before beginning, you must mark the extremity, and confirm dose administered with two-person verification. (Example use calculation: 1% lidocaine = 1g/100ml = 10mg/ml; 7 mg/kg x 70 kg patient = 490 mg; 490mg @ 10mg/ml = 49 ml 1% lidocaine). Lastly, do not forget to perform and document a time out!

I finished a block, and the patient is pain free, but now what?
Don’t forget to repeat the neurologic exam and to write a procedure note including the amount of anesthesia used, location of block, time of administration, and any potential complications. Not only does this assist billing, it provides information to all other providers treating the patient after you (like the orthopods taking your 75-year-old hip fracture to surgery later!).
I did 5 femoral nerve blocks during intern year with expert attending Dr. N Block. Can I start doing these solo?
Though you may feel comfortable after a few blocks, consensus guidelines for anesthesia residents require a minimum of 20 total ultrasound guided nerve blocks to demonstrate competency. A great way to get these numbers up is to practice in a cadaver lab or do an elective anesthesia or orthopedic block during residency to get double-digit numbers on your block. Better yet, lobby for your residency program to include US-guided nerve blocks as part of the residency core curriculum!
What about those of us in the community or out of residency; are there any good learning resources?
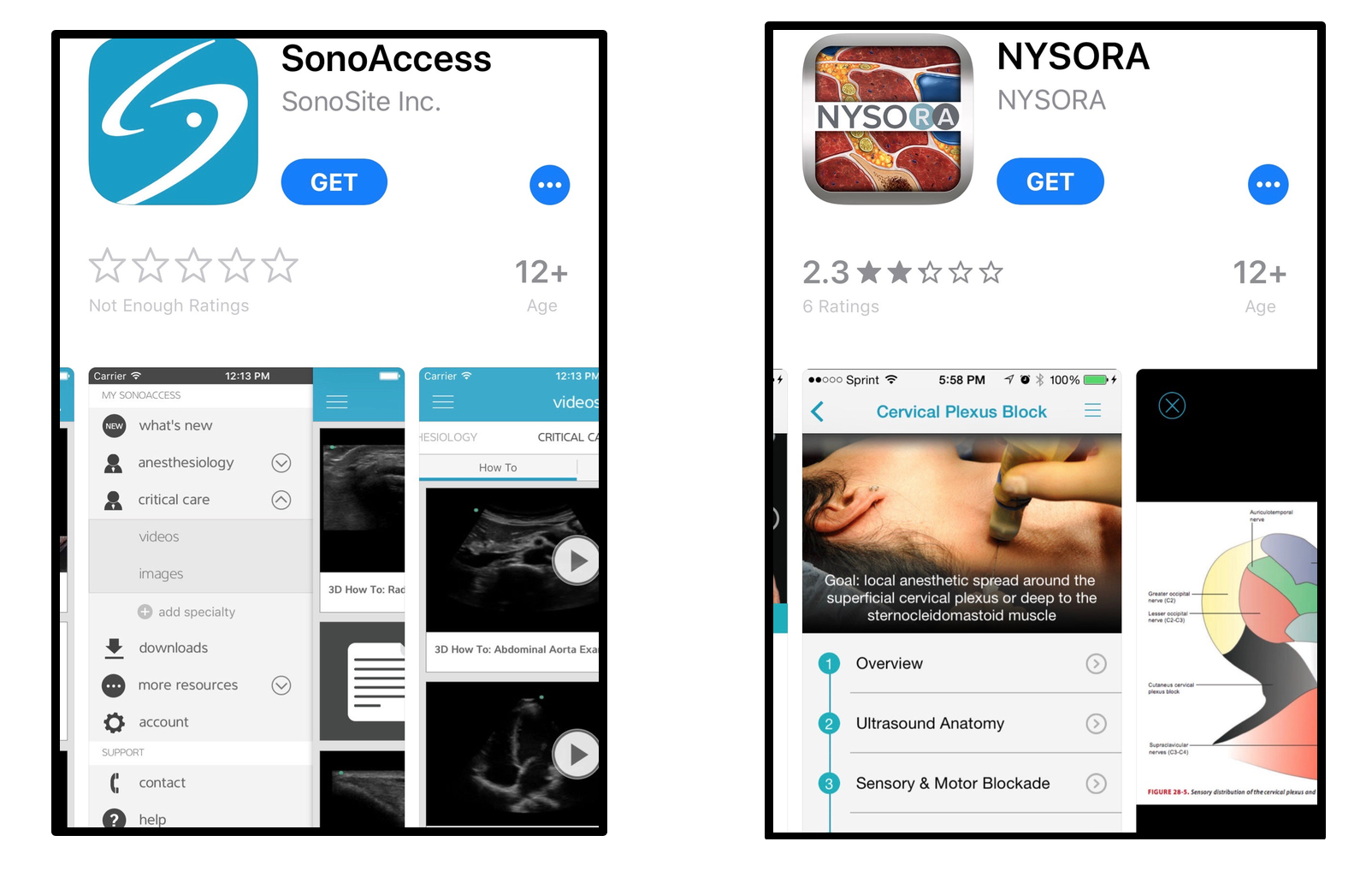
There are a number of free open-access websites you can use including Highland Ultrasound ED Block Guide, NYSORA (less ED-focused, but still useful), and 5-min Sono’s nerve block video tutorial, as well as a number of apps such as Nerve Block Star, Nerve Whiz, SonoAccess, NYSORA, andBlock GuRU Lite – $5.99). I personally love the Nerve Block Star app designed by Dr. Wilson herself. As opposed to other resources which are heavy in anesthesia-related content, Dr. Wilson’s app is tailored specifically to the emergency provider using tips and tricks she’s picked up through her time in the ED. Additionally, Nerve Block Star is centered around injury type as opposed to targeted nerve: “you have an ankle dislocation…. Ok, here’s the appropriate block and how to do it”. This is great for providers just starting out in the field who may not have mastered the anatomic nerve distribution.

Expert commentary from author Casey Wilson, MD:
“I hope this piece inspires more Emergency Physicians to consider incorporating regional anesthesia into their pain management algorithm. Oftentimes, I’m told this sounds too advanced or difficult, but I think most of us are surprised when we first start practicing this technique at how quick and simple it can really be. If you’ve ever done a dental block and seen the rapid satisfaction it can bring to your suffering patient, you’ll rapidly fall in love with the idea of using blocks elsewhere. Consider starting with the femoral nerve block in your elderly patients with hip fractures, from there, you’ll notice the fine motor skills can be applied to smaller nerves as well. This is something we can and should do for our patients, and I look forward to seeing more and more examples of how rock star EP’s are continuing to apply this skill in new ways.”
So there you have it. Ultrasound-guided nerve blocks are an easy, safe, effective non-opioid analgesic alternative that can be used by any emergency provider. Don’t forget to take a systematic approach to the patient to ensure no contraindications or potential complications. Never forget a before and after neurologic exam, and don’t forget to document! Happy blocking.
Additional Links:
Highland EM – My personal favorite site for all things related to US-guided ED Pain Management
Painandpsa – Ultrasound-Guided Regional Nerve Blocks in Emergency Medicine
5-min Sono– high-quality video tutorials:
- TAP Block
- Superficial Cervical Plexus Block
- Ulnar Block
- Median Block
- Radial Block
- Supraclavicular Block
- Interscalene Brachial Plexus Block
- Posterior Tibial Block
- Fascia Iliaca Block
- Popliteal Sciatic Block
NYSORA:
- Face and Head Blocks
- Supraclavicular Brachial Plexus Block
- Superficial Cervical Plexus Block
- Wrist Block
- Suprascapular nerve block
- Intercostal Nerve Block
Video Tutorial – Dorsal Penile Block
R.E.B.E.L. EM – Local Anesthetic Systemic Toxicity (LAST)
R.E.B.E.L. EM – Skin Anesthesia: Lidocaine vs Bupivacaine +/- Epinephrine









2 thoughts on “Pain Profiles: Feeling Blocked?”
Pingback: Nursing FOAMed Review #1 (Aug 1st - 9th) - Code Blue LLC
Pingback: LITFL Review 343 • LITFL