Authors: Gurpreet Kaur, DO (@KaurGurpreetDO, EM Resident Physician, University of Kentucky, Lexington, KY), Linda Katirji, MD (@LKatirji, EM Attending Physician, University of Kentucky, Lexington, KY) // Reviewed by: Alexander Y. Sheng, MD, MHPE (@TheShenger); Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Case 1
A 38-year-old male with no past medical history presented to the emergency department (ED) with a puncture wound from a construction site. The patient stated that he was walking around the construction site with tennis shoes when he felt severe pain in his right foot. The patient pulled a rusty nail from the sole of the foot.
Case 2
A 50-year-old female with past medical history of hypertension, hyperlipidemia, insulin-dependent diabetes, and peripheral neuropathy presented to the ED with swelling and redness of her left foot. The patient stated that she noticed the swelling 4 days ago and it has progressed. The foot is now painful and red. The patient denied any trauma to the area, numbness or weakness in the leg, or any fever and chills. The patient did not recall stepping on anything, although she admits that sensation in her feet are absent at baseline due to her peripheral neuropathy. Physical exam was remarkable for moderate swelling of her left foot up to the ankle with redness and tenderness, especially on the plantar surface where a small, subtle puncture wound was visible and associated with fluctuance.
Background
Puncture wounds are penetrating injuries caused by a pointed object. Puncture wounds with or without a retained foreign body are a common presentation to the ED.1 Plantar puncture wounds account for the majority of these injuries. Nails are the most frequently seen objects in puncture wounds, but other items such as needles, glass, wood, plastic, and metal are common causes as well. Puncture wounds are associated with complications such as soft tissue infections, deep abscess, reactive inflammation, pyogenic granuloma, epidermal inclusion cyst. Depending location of the initial injury and surrounding anatomical structures, other potential complications include osteomyelitis (if penetration of cartilage, periosteum, and bone), septic arthritis (if penetration of joint capsule), tendon laceration/dysfunction, and nerve injury. Approximately 10% of these injuries result in infections and 1-2% of those will develop osteomyelitis.1,2
Risk factors associated with infection include characteristics of the wound such as timing, location of puncture, depth, characteristic of the penetrating object, contamination, and retained foreign body or foreign body sensation.1,2,3 Elderly, immunocompromised, and patients with peripheral vascular disease and diabetes are at higher risk for infections associated with puncture wounds.4 Diabetes mellitus is one of the most significant risk factors associated with infections. Patients with diabetes are more likely to have serious infections such as osteomyelitis and most likely to require hospitalization and surgical interventions following a puncture wound.2
The inciting organism for infection differs by mechanism of injury. Most soft tissue infections associated with puncture wounds are caused by Staphylococcus and Streptococcal species. These gram-positive bacteria usually colonize the skin and typically cause cellulitis and abscess formation. Pseudomonas is the most common cause of osteomyelitis. Pseudomonas is common when puncture injury occurs through the rubber sole of athletic shoes. Puncture wounds occurring in bodies of water may involve Pseudomonas, Aeromonas hydrophila, Vibrio species, and Mycobacterium marinum. Eikenella is part of the normal oropharyngeal flora and is implicated in infection involving toothpick injuries.1,2,4,5
Evaluation
Clinically, most puncture wounds initially appear benign, in the form of a small entry point with irregular skin margins and local ecchymosis.6 Delayed presentation can present with local edema, erythema, wound drainage, lymphadenopathy.6 Taking a thorough history is imperative. Timing of the injury is critical. A wound more than 6 hours old has a high-risk profile for infection and those after 48 hours have a greater risk of secondary complications.
History should also include the type of footwear at the time of injury. Puncture wounds through a rubber sole have increased risk of pseudomonas infections, possibly due to the moist conditions in the shoe which provide a suitable environment for the growth of the organism.1,2,3 Description of the object and injury will provide the examiner valuable information regarding injury depth. Deeper penetrations are at increased risk for more serious injury, damage to surrounding tissue, and infection. Sharp objects can break off and be retained as foreign bodies. Immunization history is pertinent to update tetanus prophylaxis if needed. Obtaining a thorough past medical history is especially relevant as delayed presentation among diabetic patients has been reported to have increased incidence of osteomyelitis compared with nondiabetic patients.1,2,3
Physical Exam
Evaluation of a patient with puncture wound includes the examination of the entry site, assessing the skin appearance, inspecting, and palpating for retained foreign bodies. Inspection should include looking for any signs of infections such as local erythema, edema, drainage.1,2,3 Pain with passive movement, crepitus, and purulence may indicate a deeper infection, abscess, or serious infection. Record the location, extent of soft tissue involvement and proximity to any neurovascular structures, tendons, or joint capsules is critical.7
Evaluation of the sensation and motor function allows delineating possible damage to nerves or tendons.1,2,3 In case of delayed presentation, a puncture site may have already healed over. Take patients who complain of foreign body sensation seriously as patient perception has modest (31% positive, 89% negative) predictive value for foreign body retention.8
Imaging
Detection of any retained foreign bodies is important as stated earlier since they can lead to serious infection and inflammatory complications. Thirty-eight percent of retained foreign bodies are missed on initial examination.5 X-ray radiographs with multiple views of the injury site are recommended for all puncture wounds except in the case of knife wounds.2,3 X-ray will allow for the identification of radiopaque retained foreign bodies, fractures, and bony changes associated with infections in the region.

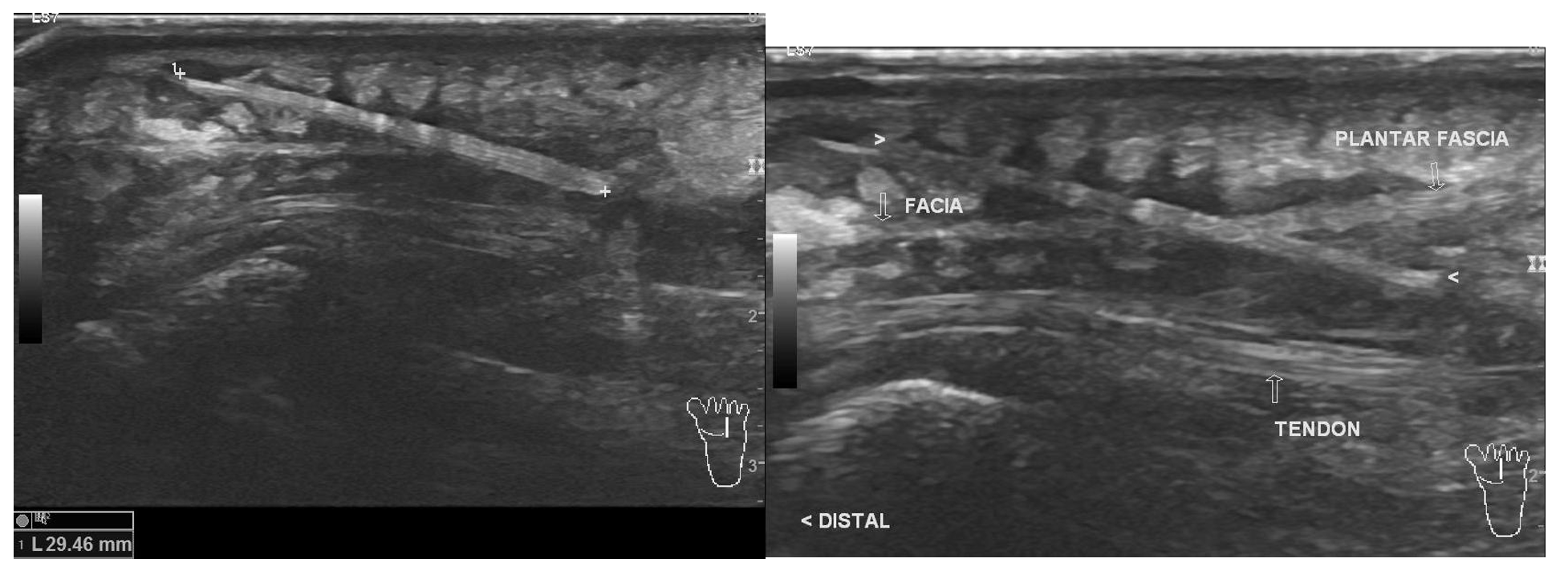
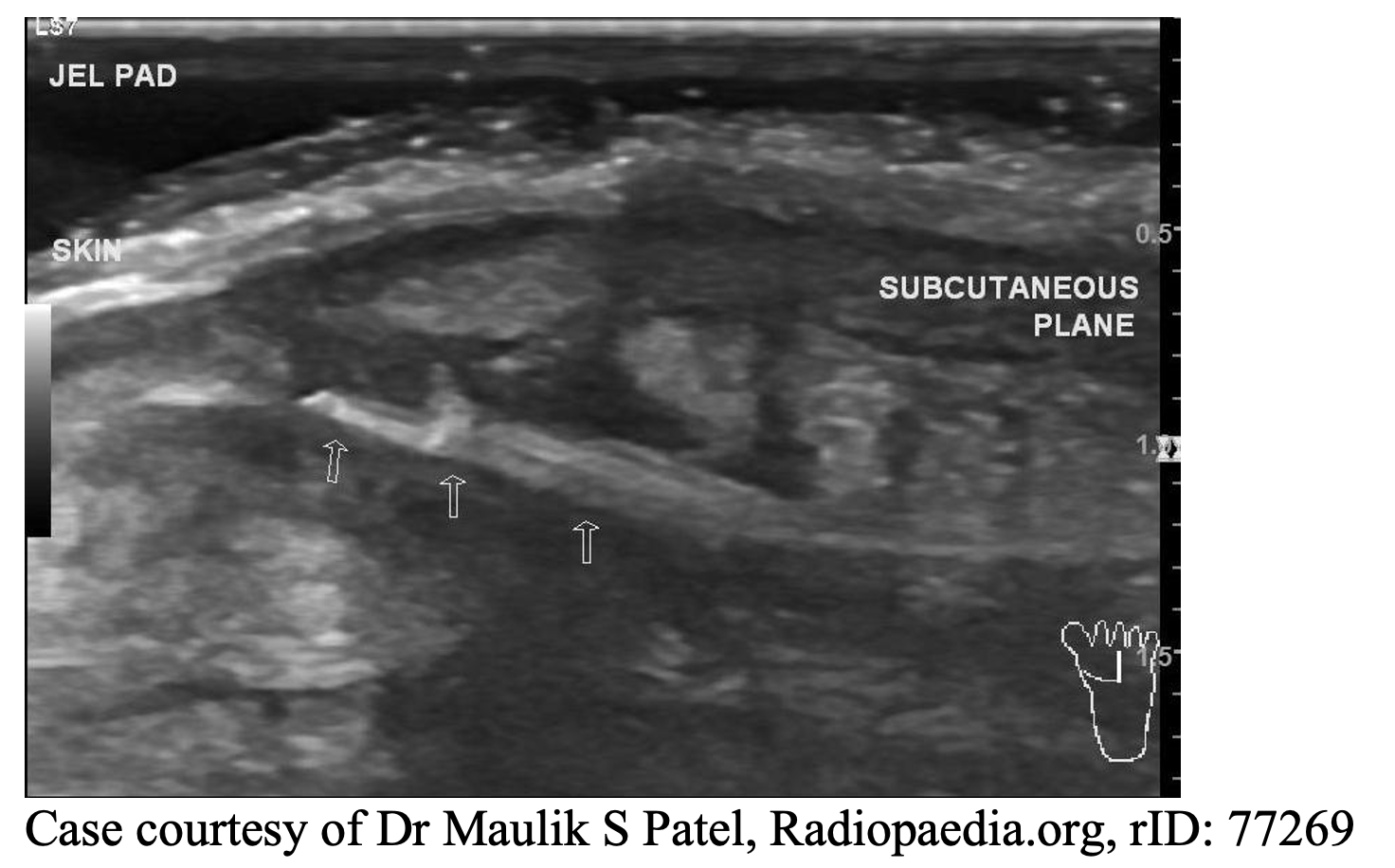
Ultrasound is another reliable tool used to detect associated abscesses and retained foreign bodies, especially organic nonradiopaque ones that are missed on x-ray and aid in their drainage/removable. Ultrasound has shown to have a sensitivity of 87% and specificity of 97% in detecting 2.5mm long wooden foreign bodies and sensitivity of 93% and specificity of 97% in 5mm long wooden foreign bodies. Similar sensitivity and specificity have been shown in the detection of glass, plastic foreign bodies.2,5 A prior Emdocs article on the topic provides valuable information on how to perform an ultrasound of soft tissue to visualize a retained foreign body.9
Advanced imaging can be considered in cases when suspected retained foreign body is not visualized on plain radiographs and ultrasound. Computed tomography and magnetic resonance imaging is also indicated when there is concern for deep-space infection, persistent pain, and treatment failure.3
Management
The majority of puncture wounds have a benign course. Almost all serious complications are associated with retained foreign body. One must have a high index of suspicious for identification and removal of retained foreign bodies.2,3Patients who present within 6 hours of an injury with a superficial puncture wound with no evidence of foreign body retention can be managed conservatively.3 Wound can be irrigated using copious amounts of normal saline solution with a 20 -mL syringe. High – pressure wound irrigation can cause tissue damage and push foreign bodies deeper therefore should be avoided. Aggressive surgical debridement, including excision of wound edges, probing the wound, and coring are generally not indicated.10 Patient can be discharged with instructions for dressing changes and strict return precautions for any signs of infection. The use of prophylactic antibiotics in the management of puncture wounds is controversial, especially for plantar puncture wounds.3,5 Antibiotics prophylaxis is recommended for use in highly contaminated, presentation greater than 6hrs, and at-risk patients (those with diabetes or immunosuppression).2
When indicated, first-generation oral cephalosporin, anti-staphylococcal penicillin, fluoroquinolone, or macrolide are recommended. Prophylaxis coverage for methicillin-resistant Staphylococcus aureus is not necessary for soft tissue infections caused by puncture wounds1 For wounds through soles of shoes, antibiotics with antipseudomonal activity, oral fluoroquinolone such as ciprofloxacin are needed.1,2,3 For deeper contaminated wounds and delayed presentation in high-risk patients, broad-spectrum oral antibiotics are recommended such as amoxicillin/clavulanic acid, trimethoprim/sulfamethoxazole, or clindamycin with ciprofloxacin.2 For patients requiring surgical debridement, parenteral antibiotics such as cefazolin, ampicillin/sulbactam, piperacillin/tazobactam, clindamycin, ciprofloxacin, and cefepime are recommended for initial broad-spectrum coverage.3
If a foreign body is suspected, attempts to remove it should be made. Many superficial objects such as needles, nail, splinters, gravel can be removed in the ED with the aid of ultrasound. Orthopedic consult should be obtained for any intra-articular foreign bodies given the increased risk for septic arthritis associated with these foreign bodies.11
Patients may present with localized abscess associated with a retained foreign body. A tender, warm, fluctuant mass can be palpated, and ultrasound can be used to aid incision and drainage.3 Deep soft tissue infection may require surgical exploration with drainage, excision of necrosis tissue and irrigation of infected areas. These patients will also require broad-spectrum parenteral antibiotics.1,2
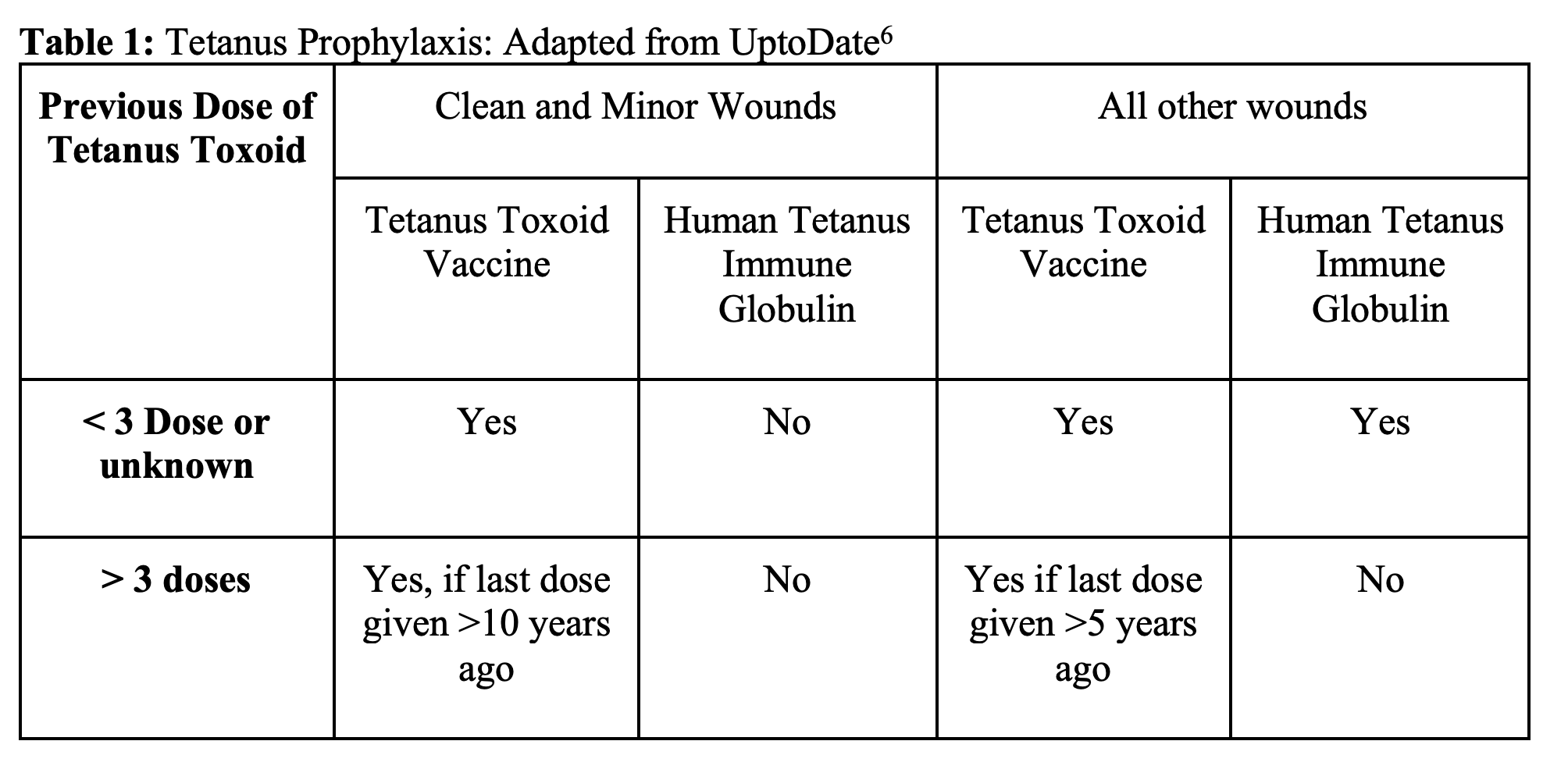
A patient’s tetanus immunization status always needs to be considered when treating these injuries since puncture wounds are susceptible to Clostridium found in but not limited to soil and feces.1,2
Case Conclusions
Case 1: Plain imaging was negative for any retained foreign bodies. Patients puncture wound was irrigated with 1L of normal saline. Dressing was applied and patient was discharged home with Cefalexin and Ciprofloxacin.
Case 2: Plain imaging was negative for any retained foreign bodies, there was significant soft tissue edema. Point of Care Ultrasound showed a fluid collection with significant cobblestoning. Incision and Drainage was performed. Patient was started on ampicillin/sulbactam and admitted to the hospital for further observation.
Pearls
- Despite their benign initial appearance, puncture wounds should be taken seriously due to risk of infection and potential sequela such as osteomyelitis and deep soft tissue infections.
- Consideration of retained foreign bodies and thorough examination and imaging (ultrasound and/or plain films) are the keys to decreasing complications.
- Staphylococcus and Streptococcal species are the most common causes of infection. Pseudomonas is an important consideration in plantar puncture wounds and the most common cause of osteomyelitis.
- The majority of puncture wounds without retained foreign bodies will have a benign course. Prophylactic antibiotics, high-pressure irrigation, and debridement are unnecessary in most cases. Educate patients re: signs and symptoms to return for.
References / Further Reading:
- Haverstock DPM, B., 2012. Puncture Wound of the Foot. Clinics in Podiatric Medicine and Surgery, 29(2), pp.311-322.
- Racz, R., Ramanujam, C. and Zgonis, T., 2020. Puncture Wound of the Foot. Clinics in Podiatric Medicine and Surgery, 27(4), pp.523-534.
- Quinn J. Puncture Wounds and Bites. In: Tintinalli JE, Ma O, Yealy DM, Meckler GD, Stapczynski J, Cline DM, Thomas SH. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 9e. McGraw-Hill; Accessed July 26, 2020. https://accessemergencymedicine-mhmedical-com.ezproxy.uky.edu/content.aspx?bookid=2353§ionid=218708499
- Belin, R. and Carrington, S., 2012. Management of Pedal Puncture Wounds. Clinics in Podiatric Medicine and Surgery, 29(3), pp.451-458.
- Boyse, T., Fessell, D., Jacobson, J., Lin, J., van Holsbeeck, M. and Hayes, C., 2001. US of Soft-Tissue Foreign Bodies and Associated Complications with Surgical Correlation. RadioGraphics, 21(5), pp.1251-1256.
- Baddour, MD, FIDSA, FAHA, L. and Brown, MD, FACEP, L., 2020. UpToDate. [online] Uptodate.com. Available at: <https://www.uptodate.com/contents/infectious-complications-of-puncture-wounds> [Accessed 1 July 2020].
- Chachad S, Kamat D. Management of Plantar Puncture Wounds in Children. Clin Pediatr (Phila). 2004;43(3):213-216. doi:10.1177/000992280404300301
- Steele M, Tran L, Watson W, Muelleman R. Retained glass foreign bodies in wounds: Predictive value of wound characteristics, patient perception, and wound exploration. Am J Emerg Med. 1998;16(7):627-630. doi:10.1016/s0735-6757(98)90161-9
- Alerhand, S., 2020. Ultrasound for Retained Radiolucent Foreign Body in Soft Tissue – Emdocs.Net – Emergency Medicine Education. [online] emDOCs.net – Emergency Medicine Education. Available at: <http://www.emdocs.net/ultrasound-for-retained-radiolucent-foreign-body-in-soft-tissue/> [Accessed 4 July 2020].
- Baldwin G, Colbourne M. Puncture Wounds. Pediatr Rev. 1999;20(1):21-23. doi:10.1542/pir.20-1-21
- Mulhall K, Sheehan E, Kearns S. Diagnosis and Management of an Intra-articular Foreign Body in the Foot. Ir Med J. 2020;95(9):277-278.
- Harrison, M., 2002. Antibiotics after puncture wounds to the foot. Emergency Medicine Journal, 19(1), pp.49-a-49.
- Case courtesy of Dr Hani Salam, <a href=”https://radiopaedia.org/”>Radiopaedia.org</a>. From the case <a href=”https://radiopaedia.org/cases/9114″>rID: 9114</a>
- Case courtesy of Dr Maulik S Patel, <a href=”https://radiopaedia.org/”>Radiopaedia.org</a>. From the case <a href=”https://radiopaedia.org/cases/77269″>rID: 77269</a>








