Authors: Matt Kostura, MD (Staff Physician, Emergency Services Institute of the Cleveland Clinic Foundation, Assistant Professor of Emergency Medicine, and Assistant Program Director CWRU/Metrohealth Medical Center/Cleveland Clinic Emergency Medicine Residency Program), Courtney Smalley, MD (Staff Physician, Emergency Services Institute of the Cleveland Clinic Foundation, Associate Professor of Emergency Medicine, and Assistant Program Director CWRU/Metrohealth Medical Center/Cleveland Clinic Emergency Medicine Residency Program) // Reviewed by: Marina Boushra, MD (Staff Physician, Emergency Services Institute of the Cleveland Clinic Foundation); Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Case 1:
A 58-year-old male with a history of CAD, HTN, and a 40-pack-year smoking history presents to the emergency department (ED) for shortness of breath (SOB). His SOB has been progressive for one week but has acutely worsened over the last day. The patient has associated chest tightness, wheezing, and worsening of chronic leg swelling. He was treated two months ago for bronchitis. HE tried using some nebulized albuterol at home but his symptoms persisted, prompting the ED visit. The patient is vaccinated against COVID and he was infected with COVID one year ago.
Vital signs on arrival to the ED are HR 120 bpm, BP 76/42 mm Hg, RR 30 per minute, O2 87% on room air, T 37.0 C (98.6F). On exam, he has moderate respiratory distress with diminished breath sounds bilaterally and bilateral pitting edema to the lower extremities. ECG is negative for STEMI and a stat portable CXR is negative for pneumonia, pneumothorax, or pulmonary edema. While the differential diagnosis in this patient is broad, careful consideration in the next steps of resuscitation and management in order to “do no harm” is necessary.
Case 2:
A 47-year-old female with a history of pulmonary arterial hypertension (PAH) presents with a medication problem. She woke up this evening with an alarm from her treprostinil pump. She states that her continuous infusion of the medication stopped working about 2 hours prior to arrival and she is concerned that the central line is not working. She tried flushing her PICC line but it does not flush or draw back. She denies any symptoms currently but presents to the emergency department at 3 am because her pulmonologist told her that she can “get sick” if she does not take her medication.
Treprostinil is not a typical medication that is stocked in the ED pyxis and may not be available in small hospitals or community settings. Furthermore, the PICC team is not available in the middle of the night to troubleshoot her central line.
Clinical Relevance
Both of the above cases demonstrate patients with a history and presentation that is concerning for an acute right heart failure (RHF) exacerbation. Early recognition of RHF and its underlying cause is a key component to the successful management of these patients in the ED. The presentation of RHF may be complex, and the treatment and resuscitation of a patient with acute RHF differ from some of the other diagnoses that mimic this disease process. This focused post will highlight the pearls and pitfalls of the ED management of RHF patients. A more detailed review from which this post was based can be found here.83
What is Right Heart Failure?
Right heart failure is defined as impaired right ventricular (RV) contractility due to myocardial dysfunction, elevated pressures, or volume overload.1,83 RHF can result from many underlying conditions, some of which are listed in Table 1 below. 8,83

The true prevalence of RHF is challenging to estimate as it depends on how RHF is defined. Current literature suggests that RHF is observed in 3-9% of all acute heart failure admissions.4-7 While RHF is rare compared to left heart failure (LHF), the presence of RHF contributes to patient morbidity and mortality. Overall mortality from RHF is estimated to be between 6% to 14%.4,5,83
RV Physiology
Understanding the basic physiology of the RV can aid the clinician in understanding and treating a patient with acute RHF. About 75% of RV contraction occurs via longitudinal contraction, a bellows-like inward movement mechanism of the RV free wall that pulls the tricuspid annulus towards the cardiac apex.14,15,83 In patients with normal physiology, the RV pushes against a highly compliant, low-resistance pulmonary vascular system, and therefore generating RV output requires only about one-fifth the amount of energy needed to generate LV output.16 Table 2 compares the physiology of the RV to the LV.
Table 2. Left and Right Ventricle Physiology. RV= right ventricle, LV = left ventricle, EF = ejection fraction, PVR = pulmonary vascular resistance, SVR = systemic vascular resistance 83

RV systolic function is highly sensitive to changes in RV afterload.17 An acute RHF exacerbation often occurs due to an abrupt increase in RV afterload or a decrease in myocardial function, rather than an acute change in volume status or preload.1,17 In an acute RHF exacerbation, the RV initially compensates by stretching, but this abrupt change in preload can worsen RV hemodynamics, causing patient decompensation.1,25-27
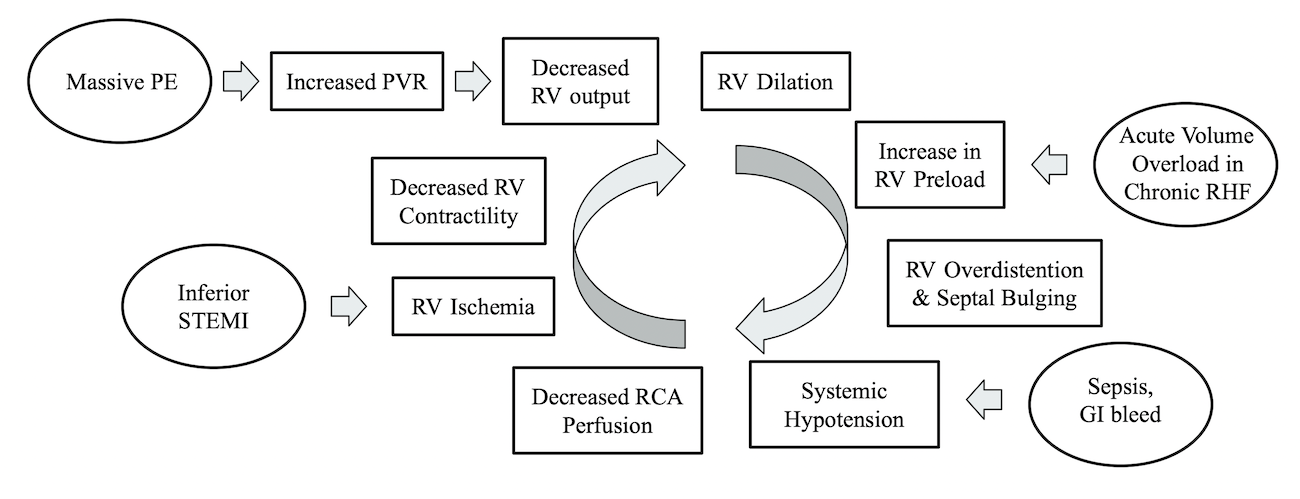
Figure 1 outlines the cyclic physiology of a right heart failure exacerbation, noting examples of underlying causes of RHF and entry points into the cycle.83 One key to understanding this cycle is that RV overdistention can lead to bulging of the interventricular septum into the LV and ultimately systemic hypotension (known as ventricular interdependence).17,18 RV overdistention can be due to a maladaptive physiologic response to an acute increase in RV afterload or pulmonary vascular resistance (PVR), or it can be due to gradual volume overload in a patient with chronic RHF.17,18 Systemic hypotension in a patient with RHF leads to worsening right coronary artery (RCA) perfusion of the RV, promoting more RV ischemia, and continuing the cycle of decompensation.27,28
Figure 1. Cyclic physiology of right heart failure. Ovals represent examples of underlying causes leading to right heart failure. PVR = pulmonary vascular resistance, RV = right ventricle, RHF = Right heart failure, PE = Pulmonary Embolism, STEMI = ST-elevation myocardial infarction, RCA = right coronary artery83
Pulmonary Hypertension
One of the common pathologic causes of chronic RHF is increased RV strain over time due to pulmonary hypertension (PH).20,29,83 PH has been classically defined as mean pulmonary artery pressure greater than 25 mm Hg as measured by right heart catheterization.30,83 While the gold standard of RV dynamic measurements is cardiac magnetic resonance imaging (MRI), an RV pressure greater than 35 mmHg on echocardiogram strongly suggests PH.31,32
PH is caused by a number of etiologies, which are divided into five World Health Organization (WHO) sub-categories.30,33
- Group 1: Pulmonary Arterial Hypertension – Rare, causes include underlying genetic conditions, infectious diseases such as HIV or schistosomiasis, toxins, or idiopathic
- Group 2: Chronic Left Heart Disease – Most common cause of PH
- Group 3: Chronic Lung Conditions – Second most common cause of PH
- Group 4: Sequela of Thromboemboli
- Group 5: Multifactorial or unknown mechanisms
RHF is the leading cause of death in patients with PAH.20,34 A patient with PH can be “tipped” into the cycle of acute RHF by a number of underlying mechanisms.
ED Presentation and Evaluation
The most common complaint in patients with PH is dyspnea.35,83 Depending on the severity of RHF, the patient may also present with chest pain, fatigue, peripheral edema, or lightheadedness.35.83 Syncope and pre-syncope in a patient with PH or RHF are concerning and warrant further evaluation for dysrhythmia, valvular pathology, and elevated RV pressures.25,83
The following labs and imaging studies can aid the clinician in the initial workup of a patient with RHF. If the patient has underlying PH or chronic RHF, trending labs may be useful.40
- CBC
- CMP
- Cardiac markers including troponin and brain natriuretic peptide (BNP)
- Chest X-ray (CXR)
- ECG
- Echocardiogram
There are no specific findings on ECG to diagnose RHF or PH. Common ECG findings in patients with PH include the following:41,42, 83
- Right axis deviation
- Right bundle branch block
- Normal sinus rhythm
- ST depression or T wave inversions in V1 and the inferior leads
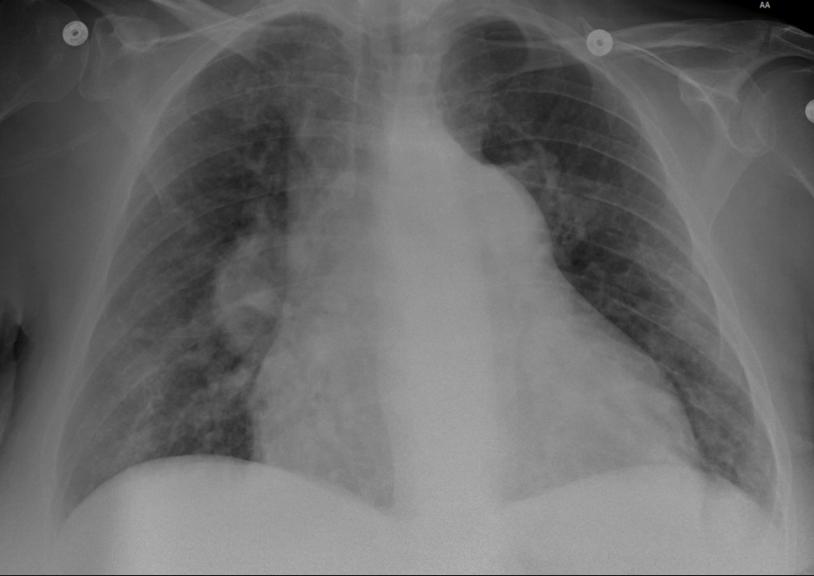
Imaging studies such as CXR may aid in the diagnosis of RHF. CXR findings in a patient with chronic RHF include the following and are demonstrated in Figure 2:45,46
- RV enlargement
- Globular cardiac silhouette with loss of the retrocardiac space
- Enlarged right atrium with rightward displacement of the cardiac silhouette beyond the spine
Figure 2. CXR in a patient with chronic right heart failure due to pulmonary arterial hypertension.
POCUS in RHF
Point of care cardiac ultrasound (POCUS) is a valuable tool in a patient with suspected RHF, not only to look for signs of acute RHF but also to identify other causes of the patient’s symptoms that may mimic RHF. POCUS assessments particular to RHF include an assessment of the following:48
- RV free-wall thickness
- Inferior vena cava (IVC) size and respirophasic variability
- RV to LV ratio
- Tricuspid annular plane of systolic exertion (TAPSE)
- Interventricular wall flattening
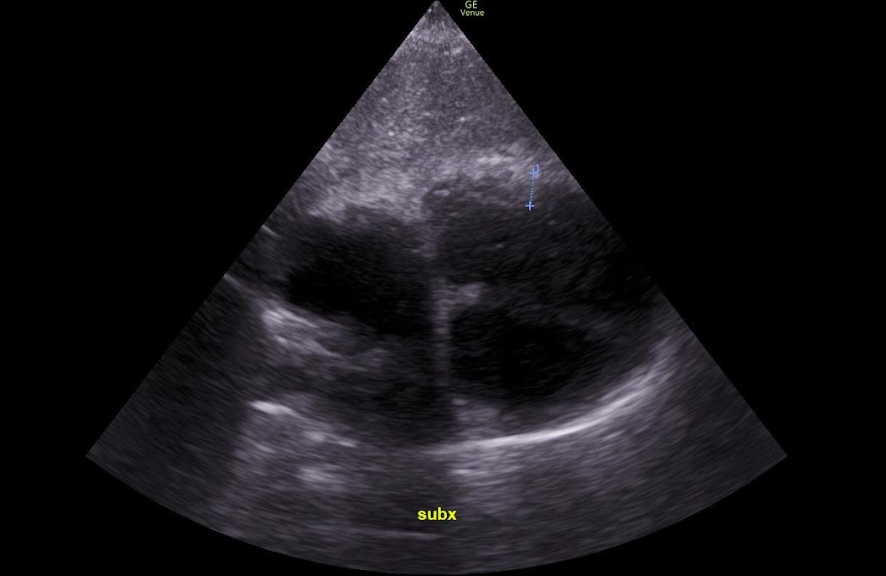
A normal RV wall is less than 5mm and is ideally measured in the subxiphoid view such as demonstrated in Figure 3.49 A thickened free wall indicates chronic RV failure which can be due to a number of underlying causes.49
Figure 3. Thickened RV free-wall measured in a subxiphoid view in a patient with chronic RHF.83
An IVC diameter greater than 2.1 cm and less than 50% collapse with patient sniff suggests high right atrial pressures.49 In acute RHF, this may indicate excess volume or an acute change in RV afterload, but interpretation should be clinically correlated with the patient’s history and physical examination.44,83 IVC measurements are more difficult to interpret clinically in a patient with chronic PH.83 Video 1 demonstrates a dilated IVC with minimal respiratory variation in a patient who is volume overloaded.83
Video 1. POCUS with dilated IVC and minimal respirophasic variation.83
The overall RV size and the ratio of the RV to the LV can be measured in an apical 4-chamber cardiac view at the base of the heart in end-diastole. A normal RV to LV ratio is 0.6:1.0 .48,52 An RV to LV ratio of 1:1 or an RV basal diameter greater than 41 mm is concerning for RV dilation.48,49 Video 2 demonstrates a dilated RV in a patient with chronic RHF.83
Video 2. Dilated RV on apical 4 chamber view in a patient with chronic RHF.83
TAPSE measurement gives an assessment of RV systolic function due to the bellows-like motion of the RV contraction.48,49 TAPSE is measured by placing the M mode cursor over the lateral portion of the tricuspid annulus in an apical 4-chamber view.49 Normal measurement from peak to valley of the tricuspid motion in M-mode is greater than 17 mm.49,53 Figure 5 demonstrates a normal TAPSE measurement. Limitations of TAPSE measurement include decreased accuracy in patients with regional differences in RV function, inability to distinguish between acute and chronic RHF, and the numerical value can be affected by the angle of the M-mode cursor over the tricuspid annulus.49,50
Figure 4. The blue lines in the M-mode image demonstrate a normal TAPSE measurement, which in this case was 23 mm.83

Finally, the parasternal short-axis view can be used to assess for interventricular flattening or RV bulging. Interventricular flattening is also known as the “D-sign”, as the LV takes on a D shape, rather than the circular shape in normal physiology.49 In extreme build-up of RV volume or pressure, septal dyskinesia may be present, in which the RV bulges into the LV, thus compromising the patient’s hemodynamics.49 Video 3 shows a patient with acute on chronic RHF with volume overload and interventricular flattening on the parasternal short axis view.83
Video 3. Parasternal short axis view in a patient with acute on chronic RHF who is volume overloaded. Note the “D” shape to the RV and LV.83
ED Management of RHF
RHF can present acutely with signs of cardiogenic shock or more insidiously.20,25,83 One of the tenets of management of an acute RHF exacerbation is to find, treat, and reverse the underlying cause. The underlying causes of an RHF exacerbation can include the following:
- STEMI
- Massive Pulmonary Embolism
- Arrhythmia
- Medication non-compliance in a patient with chronic RHF
- Sepsis
- GI bleeding
- Acute respiratory illness / COPD exacerbation
While searching for the underlying cause of RHF, it is important to manage the patient’s “ABCs” (airway, breathing, and circulation). Placing a hypoxic RHF patient on supplemental oxygen is helpful for resuscitation.75 More advanced airway adjuncts such as high flow nasal cannula (HFNC) or non-invasive positive pressure ventilation (NIPPV) may be needed to improve oxygenation. If possible, one should avoid intubating a patient with RHF, as positive pressure ventilation.75 Patients with acute dysrhythmia such as atrial fibrillation benefit from rapid electrical cardioversion, as loss of atrial kick can further impair RV cardiac output.24,55,83 If the ECG is concerning for an acute RV myocardial infarction, emergent coronary reperfusion is indicated, however nitrates or diuretics should be avoided, as the decrease in preload can result in patient decompensation.44
Optimizing hemodynamics such as preload, afterload, and contractility is important in RHF in order to prevent further decompensation.20,32
Preload
While a failing RV is preload dependent, hypotension does not necessarily mean the patient is hypovolemic, and an accurate assessment of volume status is necessary.20,44 Patient history, physical exam, and POCUS findings should be synthesized to help a clinician decide if the patient needs fluids, diuresis, or nothing (indicating the patient is euvolemic).44 If the patient appears intravascularly depleted, small boluses of isotonic fluids (250 ml boluses) and frequent patient reassessment are recommended to avois the risk of causing RV overdistention, i.32,44
Afterload
The afterload of the RV is dependent on the pulmonary vascular resistance (PVR).17 Areas of the lung that are hypoxic and acidotic will lead to pulmonary vasoconstriction, increasing PVR, and thus increasing RV afterload. So optimizing oxygenation such as with HFNC or improving respiratory acidosis with nebulized beta-agonists can improve RV afterload.32,55 However, intubation increases intrathoracic pressure which decreases RV preload and worsens RV hemodynamics.55,75 Thus intubation should be avoided if possible.55,75 NIPPV may be an acceptable alternative in some patients with persistent hypoxia but even NIPPV can also affect preload so this should be carefully monitored.20,55,75
Though evidence in RHF is limited, other medications that have the potential to reduce RV afterload are listed below.
- Inhaled nitric oxide – causes pulmonary vasodilation which can improve V/Q mismatch 60
- Diuretics – hypervolemia increases afterload 59
- IV pulmonary artery vasodilators (IV epoprostenol or IV treprostinil)
- These infusions are reserved for patients with chronic PAH (Group 1 PH) and are not well studied in the acute RHF setting.63
- Withdrawal from IV pulmonary artery vasodilators can precipitate a pulmonary hypertension crisis and acute RHF, so if a chronic infusion stops, restart medication administration as soon as possible via a peripheral or central IV line.25,65
- Inhaled epoprostenol – may not benefit all patients, but could be considered for acute RHF in consultation with an intensivist or pulmonology.77
Contractility
Either dobutamine or milrinone can be used in a patient with acute RHF to increase contractility and lower PVR.67,68 The lowest effective dose is recommended to decrease the risk of dysrhythmias or systemic hypotension, which can occur with either of these medications.72
If systemic hypotension occurs due to any cause in a patient with RHF, one should quickly start IV vasopressors.32 If the patient’s systolic blood pressure drops below RV pressures, right heart hemodynamics can quickly worsen and the patient may decompensate.20,27-28 IV vasopressors to consider in an RHF patient with hypotension are listed below.
- Norepinephrine – First line 72
- Vasopressin – Second line 73
- Phenylephrine- NOT recommended as it worsens PVR 74
Crashing Patient
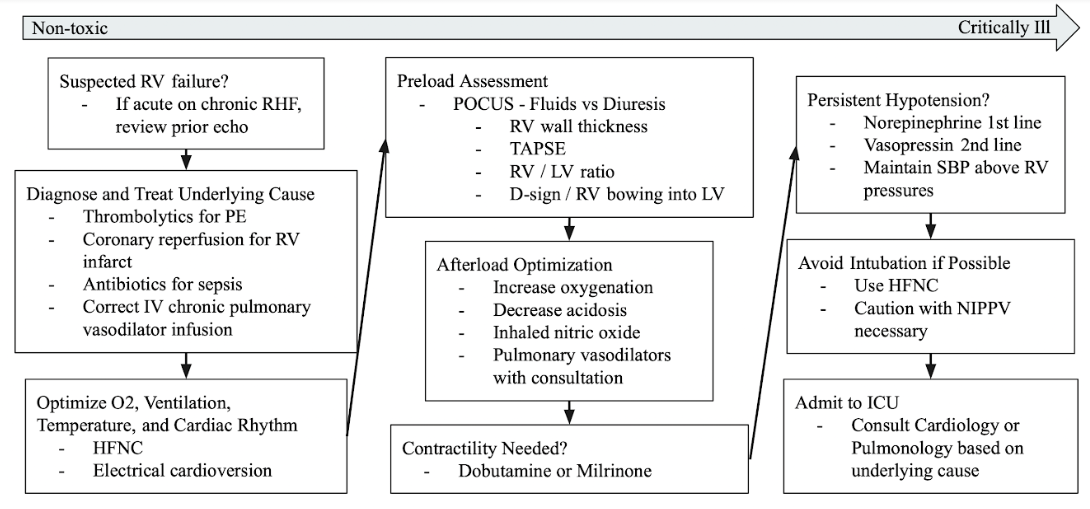
In an ideal situation, one should recognize RHF early and treat the patient in a stepwise fashion as described here and summarized in Figure 6.83 However some patients may present critically ill and require emergent intubation. If intubation is required, it is recommended to be performed by the most experienced provider with a vasopressor infusion running during intubation or quickly available at the bedside.78 The risk of intubation and mechanical ventilation is that the increase in intrathoracic pressure worsens preload and RV hemodynamics putting the patient at risk for cardiac arrest.55,75 Therefore, if the patient is mechanically ventilated the following settings are recommended in order to limit the effects of positive pressure ventilation on the right heart.
- Low Tidal Volume 78
- Low PEEP 78
- Keep Plateau pressure < 30 mmHg 25
- Avoid hypoxia and hypercapnia (leads to increased PVR) 78,81
Keeping all of these goals in balance while preventing the patient from decompensating can be challenging, so consider early consultation with a pulmonary intensivist.
While the literature on extracorporeal membrane oxygenation (ECMO) in acute RHF is limited, it can be considered as a bridge while reversible causes are treated (such as a thrombectomy for a PE),or as a bridge to RV assist device implantation.82 Mechanical RV assist devices (RVADs) are under study, but use is currently limited to end-stage disease or as a bridge to transplantation in patients with PH.20,83
Most patients presenting with acute RHF will require admission to the ICU, depending on the severity of the disease and its underlying cause.
Figure 6. Summary of key management points in a patient presenting with acute RHF.83
Case Resolutions
Case 1: COPD exacerbation or PE are highest on the differential diagnosis at this point. Nebulized beta-agonists are started and the patient is placed on HFNC with improvement in his oxygenation to 92%. POCUS assessment is notable for a thin RV free wall, positive “D sign” on parasternal long axis view, a dilated IVC, and a TAPSE of 12 mm. On chart review, the prior echocardiogram was notable for a normal LV ejection fraction, but moderately elevated RV systolic pressures. There is concern for an acute PE, but given the patient’s current hypotension and POCUS findings, there is also a concern for acute RHF. An IV infusion of norepinephrine is started to improve the patient’s BP to 90s/60s. Dobutamine is also started to augment RV contractility prior to the patient going to the CT scanner. CT angiogram of the chest is notable for acute PEs in the left and right pulmonary arteries. A PE resuscitation team is consulted to decide on IV thrombolytics vs a thrombectomy and the patient is admitted to the medical ICU in critical but improved condition.
Case 2: Recalling the short half-life of treprostinil of 2-4 hours, it is important to mobilize the ED resuscitation team quickly to establish a good functioning peripheral IV. Rather than waiting on the central pharmacy for a medication that the hospital may not carry, consider working with the patient to attach the treprostinil pump to the peripheral IV and begin the infusion. The pump appears to be functioning well and the medication is successfully restarted. It is imperative to ensure that she has an adequate supply of treprostinil with her for the next day. The patient is then admitted to the hospital overnight so that the PICC team can replace her central line in the morning.
Pitfalls and Pearls
- Keep RHF on the differential diagnosis in patients with underlying pathology that affects the right heart and lungs.
- Treat the underlying cause of an acute RHF exacerbation while optimizing preload, afterload, and contractility.
- POCUS, along with patient history and physical exam, is key to assessing patient volume status.
- Dobutamine or milrinone can improve the contractility of the RV. Phenylephrine should be avoided when possible due to increase in PVR.
- Avoid systemic hypotension and be quick to use norepinephrine and/or vasopressin if the patient decompensates.
- Avoid intubation when possible, utilizing HFNC or NIPPV first, as mechanical ventilation worsens RV hemodynamics.
References
- Thandavarayan R, Chitturi K, Guha A. Pathophysiology of Acute and Chronic Right Heart Failure. Cardiol Clin. 2020;38(2):149-160. doi:10.1016/j.ccl.2020.01.009
- Hunt S, Baker D, Chin M, et al. ACC/AHA Guidelines for the Evaluation and Management of Chronic Heart Failure in the Adult: Executive Summary A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1995 Guidelines for the Evaluation and Management of Heart Failure). Circulation. 2001;104(24):2996-3007. doi:10.1161/hc4901.102568
- Storrow AB, Jenkins CA, Self WH, et al. The burden of acute heart failure on U.S. emergency departments. JACC Heart Fail. 2014;2:269–77. doi:10.1016/j.jchf.2014.01.006
- Logeart D, Isnard R, Resche-Rigon M, et al. Current aspects of the spectrum of acute heart failure syndromes in a real-life setting: the OFICA study. Eur J Heart Fail. 2013;15(4):465–76. doi:10.1093/eurjhf/hfs189
- Maggioni AP, Dahlstroem U, Filippatos G, et al. EURObservational Research programme: the heart failure pilot survey (ESC-HF Pilot). Eur J Heart Fail. 2010;12(10):1076–84. doi:10.1093/eurjhf/hfq154
- Chioncel O, Vinereanu D, Datcu M, et al.. The Romanian Acute Heart Failure Syndromes (RO-AHFS) registry. Am Heart J. 2011;162:142–153. doi:10.1016/j.ahj.2011.03.033
- Nieminen MS, Brutsaert D, Dickstein K, et al. EuroHeart Failure Survey II (EHFS II): a survey on hospitalized acute heart failure patients: description of population. Eur Heart J. 2006;27:2725–2736. doi:10.1093/eurheartj/ehl193
- Ashraf H, Rosenthal J. Right Heart Failure. Cardiol Clin. 2020;38(2):175-183. doi:10.1016/j.ccl.2020.01.008
- Gorter T, van Veldhuisen D, Bauersachs J et al. Right heart dysfunction and failure in heart failure with preserved ejection fraction: mechanisms and management. Position statement on behalf of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2017;20(1):16-37. doi:10.1002/ejhf.1029
- Gulati A, Ismail TF, Jabbour A, et al. The prevalence and prognostic significance of right ventricular systolic dysfunction in nonischemic dilated cardiomyopathy. Circulation. 2013;128(15):1623–33. doi: 10.1161/CIRCULATIONAHA.113.002518
- Andersen HR, Falk E, Nielsen D. Right ventricular infarction: frequency, size and topography in coronary heart disease: a prospective study comprising 107 consecutive autopsies from a coronary care unit. J Am Coll Cardiol. 1987;10(6):1223–32. doi: 10.1016/s0735-1097(87)80122-5
- Jacobs A, Leopold J, Bates E et al. Cardiogenic shock caused by right ventricular infarction. J Am Coll Cardiol. 2003;41(8):1273-1279. doi:10.1016/s0735-1097(03)00120-7
- Coutance G, Cauderlier E, Ehtisham J, et al. The prognostic value of markers of right ventricular dysfunction in pulmonary embolism: a meta-analysis. Crit Care. 2011;15:R103. doi:10.1186/cc10119
- Haddad F, Couture P, Tousignant C, Denault AY. The right ventricle in cardiac surgery, a perioperative perspective: I. Anatomy, physiology, and assessment. Anesth Analg. 2009;108:407–421. doi:10.1213/ane.0b013e31818f8623
- Brown SB, Raina A, Katz D, et al. Longitudinal shortening accounts for the majority of right ventricular contraction and improves after pulmonary vasodilator therapy in normal subjects and patients with pulmonary arterial hypertension. Chest. 2011;140(1):27–33. doi: 10.1378/chest.10-1136
- Friedberg MK, Redington AN. Right versus left ventricular failure: differences, similarities, and interactions. Circulation. 2014;129:1033–1044. doi: 10.1161/CIRCULATIONAHA.113.001375.
- Sheehan F, Redington A. The right ventricle: anatomy, physiology and clinical imaging. Heart. 2008;94:1510–1515. doi: 10.1136/hrt.2007.132779.
- Santamore WP, Dell’Italia LJ. Ventricular interdependence: significant left ventricular contributions to right ventricular systolic function. Prog Cardiovasc Dis. 1998;40:289–308. doi:10.1016/s0033-0620(98)80049-2
- Guazzi M, Naeije R. Pulmonary hypertension in heart failure: pathophysiology, pathobiology, and emerging clinical perspectives. J Am Coll Cardiol. 2017;69:1718–1734. doi: 10.1016/j.jacc.2017.01.051.
- Cassady S, Ramani G. Right Heart Failure in Pulmonary Hypertension. Cardiol Clin. 2020;38(2):243-255. doi:10.1016/j.ccl.2020.02.001
- Ryan JJ, Huston J, Kutty S, et al. Right ventricular adaptation and failure in pulmonary arterial hypertension. Can J Cardiol. 2015;31(4):391–406. doi:10.1016/j.cjca.2015.01.023
- Rana B, Robinson S, Francis R, et al. Tricuspid regurgitation and the right ventricle: risk stratification and timing of intervention. Echo Res Pract. 2019;6(1):R25–39. doi:10.1530/ERP-18-0051
- Damman K, van Deursen VM, Navis G, et al. Increased central venous pressure is associated with impaired renal function and mortality in a broad spectrum of patients with cardiovascular disease. J Am Coll Cardiol. 2009;53(7):582–8. doi:10.1016/j.jacc.2008.08.080
- Tongers J, Schwerdtfeger B, Klein G, et al. Incidence and clinical relevance of supraventricular tachyarrhythmias in pulmonary hypertension. Am Heart J. 2007;153(1):127–32. doi:10.1016/j.ahj.2006.09.008
- Greenwood J, Spangler R. Management of Crashing Patients with Pulmonary Hypertension. Emerg Med Clin North Am. 2015;33(3):623-643. doi:10.1016/j.emc.2015.04.012
- Dell’Italia LJ. The right ventricle: anatomy, physiology, and clinical importance. Curr Probl Cardiol. 1991;16:653–720. doi:10.1016/0146-2806(91)90009-y
- Van Wolferen SA, Marcus JT, Westerhof N, et al. Right coronary artery flow impairment in patients with pulmonary hypertension. Eur Heart J. 2008;29:120–7. doi:10.1093/eurheartj/ehm567
- Minai OA, Yared JP, Kaw R, et al. Perioperative risk and management in patients with pulmonary hypertension. Chest. 2013;144:329-340. doi:10.1378/chest.12-1752
- Konstam M, Kiernan M, Bernstein D et al. Evaluation and Management of Right-Sided Heart Failure: A Scientific Statement From the American Heart Association. Circulation. 2018;137(20). doi:10.1161/cir.0000000000000560
- Galiè N, Humbert M, Vachiery J et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J. 2015;37(1):67-119. doi:10.1093/eurheartj/ehv317
- Surkova E, Muraru D, Iliceto S, et al. The use of multimodality cardiovascular imaging to assess right ventricular size and function. Int J Cardiol. 2016; 214:54–69. doi:10.1016/j.ijcard.2016.03.074
- Wilcox S, Kabrhel C, Channick R. Pulmonary Hypertension and Right Ventricular Failure in Emergency Medicine. Ann Emerg Med. 2015;66(6):619-628. doi:10.1016/j.annemergmed.2015.07.525
- Maron BA, Choudhary G, Khan UA, et al. Clinical profile and underdiagnosis of pulmonary hypertension in US veteran patients. Circ Heart Fail. 2013;6:906-912. doi:10.1161/CIRCHEARTFAILURE.112.000091
- Campo A, Mathai SC, Le Pavec J, et al. Outcomes of hospitalisation for right heart failure in pulmonary arterial hypertension. Eur Respir J. 2011;38(2):359–67. doi:10.1183/09031936.00148310
- Ling Y, Johnson MK, Kiely DG, et al. Changing demographics, epidemiology, and survival of incident pulmonary arterial hypertension: results from the Pulmonary Hypertension Registry of the United Kingdom and Ireland. Am J Respir Crit Care Med. 2012;186:790–6. doi:10.1164/rccm.201203-0383OC
- Kruger S, Graf J, Merx NW, et al. Brain natriuretic peptide predicts right heart failure in patients with acute pulmonary embolism. Am Heart J. 2004;147:60–5. doi:10.1016/s0002-8703(03)00528-3
- Benza RL, Miller DP, Gomberg-Maitland M, et al. Predicting survival in pulmonary arterial hypertension: insights from the Registry to Evaluate Early and Long-term Pulmonary Arterial Hypertension Disease Management (REVEAL). Circulation. 2010;122:164–72. doi:10.1161/CIRCULATIONAHA.109.898122
- Chen AA, Wood MJ, Krauser DG, et al. NT-proBNP levels, echocardiographic findings, and outcomes in breathless patients: results from the ProBNP Investigation of Dyspnoea in the Emergency Department (PRIDE) echocardiographic substudy. Eur Heart J. 2006;27:839-845. doi:10.1093/eurheartj/ehi811
- Shah SJ, Thenappan T, Rich S, et al. Association of serum creatinine with abnormal hemodynamics and mortality in pulmonary arterial hypertension. Circulation. 2008;117(19):2475–83. doi:10.1161/CIRCULATIONAHA.107.719500
- Samsky MD, Patel CB, DeWald TA, et al. Cardiohepatic interactions in heart failure: an overview and clinical implications. J Am Coll Cardiol. 2013;61:2397–2405. doi:10.1016/j.jacc.2013.03.042.
- McGoon M, Gutterman D, Steen V, et al. Screening, early detection, and diagnosis of pulmonary arterial hypertension: ACCP Evidence-Based Clinical Practice Guideline. Chest. 2004;126:14S–34S. doi:10.1378/chest.126.1_suppl.14S
- Bossone E, Paciocco G, Iarussi D, et al. The prognostic role of the ECG in primary pulmonary hypertension. Chest. 2002;121:513–8. doi:10.1378/chest.121.2.513
- Bowers TR, O’Neill WW, Grines C, et al.. Effect of reperfusion on biventricular function and survival after right ventricular infarction. N Engl J Med. 1998;338:933–940. doi: 10.1056/NEJM199804023381401
- Harjola V, Mebazaa A, Čelutkienė J et al. Contemporary management of acute right ventricular failure: a statement from the Heart Failure Association and the Working Group on Pulmonary Circulation and Right Ventricular Function of the European Society of Cardiology. Eur J Heart Fail. 2016;18(3):226-241. doi:10.1002/ejhf.478
- Lupi E, Dumont C, Tejada VM, et al. A radiologic index of pulmonary arterial hypertension. Chest. 1975;68:28–31. doi:10.1378/chest.68.1.28
- Matthay RA, Schwarz MI, Ellis JH Jr, et al. Pulmonary artery hypertension in chronic obstructive pulmonary disease: determination by chest radiography. Invest Radiol. 1981;16:95–100. doi:10.1097/00004424-198103000-00003
- Tan RT, Kuzo R, Goodman LR, et al. Utility of CT scan evaluation for predicting pulmonary hypertension in patients with parenchymal lung disease. Medical College of Wisconsin Lung Transplant Group. Chest. 1998;113:1250–6. doi:10.1378/chest.113.5.1250
- Schneider M, Binder T. Echocardiographic evaluation of the right heart. Wien Klin Wochenschr. 2018;130(13-14):413-420. doi:10.1007/s00508-018-1330-3
- Rudski LG, Lai WW, Afilalo J, Hua L, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685–713. doi:10.1016/j.echo.2010.05.010
- Fields J, Davis J, Girson L et al. Transthoracic Echocardiography for Diagnosing Pulmonary Embolism: A Systematic Review and Meta-Analysis. Journal of the American Society of Echocardiography. 2017;30(7):714-723.e4. doi:10.1016/j.echo.2017.03.004
- Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1–39. doi:10.1016/j.echo.2014.10.003
- Peterson D, Arntfield RT. Critical care ultrasonography. Emerg Med Clin North Am. 2014;32:907-926. doi:10.1016/j.emc.2014.07.011
- Tamborini G, Pepi M, Galli CA, et al. Feasibility and accuracy of a routine echocardiographic assessment of right ventricular function. Int J Cardiol. 2007;115:86-9. doi:10.1016/j.ijcard.2006.01.017
- Konstantinides SV, Torbicki A, Agnelli G, et al. 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35:3033–3069. doi:10.1093/eurheartj/ehu283
- Hoeper MM, Granton J. Intensive care unit management of patients with severe pulmonary hypertension and right heart failure. Am Respir Crit Care Med. 2011;184:1114-1124. doi:10.1164/rccm.201104-0662CI
- Ellison DH. Diuretic therapy and resistance in congestive heart failure. Cardiology. 2001;96:132–143. doi:10.1159/000047397
- Felker GM, Lee KL, Bull DA, et al. NHLBI Heart Failure Clinical Research Network. Diuretic strategies in patients with acute decompensated heart failure. N Engl J Med. 2011;364:797–805. doi:10.1056/NEJMoa1005419.
- Boerrigter G, Burnett JC Jr. Cardiorenal syndrome in decompensated heart failure: prognostic and therapeutic implications. Curr Heart Fail Rep. 2004;1:113–120. doi:10.1007/s11897-004-0020-9
- Marenzi G, Lauri G, Grazi M, et al. Circulatory response to fluid overload removal by extracorporeal ultrafiltration in refractory congestive heart failure. J Am Coll Cardiol. 2001;38:963–968. doi:10.1016/s0735-1097(01)01479-6
- Ghadimi K, Rajagopal S. Nasally Inhaled Nitric Oxide for Sudden Right-Sided Heart Failure in the Intensive Care Unit: NO Time Like the Present. J Cardiothorac Vasc Anesth. 2019;33(3):648-650. doi:10.1053/j.jvca.2018.10.008
- Pepke-Zaba J, Higenbottam TW, Dinh-Xuan AT, et al. Inhaled nitric oxide as a cause of selective pulmonary vasodilatation in pulmonary hypertension. Lancet. 1991;338(8776):1173–4. doi:10.1016/0140-6736(91)92033-x
- Monzo L, Reichenbach A, Al-Hiti H et al. Acute Unloading Effects of Sildenafil Enhance Right Ventricular–Pulmonary Artery Coupling in Heart Failure. J Card Fail. 2021;27(2):224-232. doi:10.1016/j.cardfail.2020.11.007
- Agarwal R, Gomberg-Maitland M. Current therapeutics and practical management strategies for pulmonary arterial hypertension. Am Heart J. 2011;162:201-213. doi:10.1016/j.ahj.2011.05.012
- Creagh-Brown BC, Griffiths MJ, Evans TW. Bench-to-bedside review: inhaled nitric oxide therapy in adults. Crit Care. 2009;13(3):221. doi:10.1186/cc7734
- Rubenfire M, McLaughlin VV, Roblee A, et al. Transition from epoprostenol to treprostinil in pulmonary arterial hypertension: a controlled trial. Chest. 2007;132:757–63. doi:10.1378/chest.06-2118
- Anderson JR, Nawarskas JJ. Pharmacotherapeutic management of pulmonary arterial hypertension. Cardiol Rev. 2010;18:148–62. doi:10.1097/CRD.0b013e3181d4e921
- Scott M, Winters M. Congestive Heart Failure. Emerg Med Clin North Am. 2015;33(3):553-562. doi:10.1016/j.emc.2015.04.006
- Mebazaa A, Nieminen M, Packer M et al. Levosimendan vs Dobutamine for Patients With Acute Decompensated Heart Failure. JAMA. 2007;297(17):1883. doi:10.1001/jama.297.17.1883
- Yamani M, Haji S, Starling R et al. Comparison of dobutamine-based and milrinone-based therapy for advanced decompensated congestive heart failure: Hemodynamic efficacy, clinical outcome, and economic impact. Am Heart J. 2001;142(6):998-1002. doi:10.1067/mhj.2001.119610
- Eichhorn E, Konstam M, Weiland D et al. Differential effects of milrinone and dobutamine on right ventricular preload, afterload and systolic performance in congestive heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol. 1987;60(16):1329-1333. doi:10.1016/0002-9149(87)90616-3
- Aranda J, Schofield R, Pauly D et al. Comparison of dobutamine versus milrinone therapy in hospitalized patients awaiting cardiac transplantation: A prospective, randomized trial. Am Heart J. 2003;145(2):324-329. doi:10.1067/mhj.2003.50
- Price LC, Wort SJ, Finney SJ, et al. Pulmonary vascular and right ventricular dysfunction in adult critical care: current and emerging options for management: a systematic literature review. Crit Care. 2010;14:R169. doi:10.1186/cc9264
- Currigan DA, Hughes RJ, Wright CE, et al. Vasoconstrictor responses to vasopressor agents in human pulmonary and radial arteries: an in vitro study. Anesthesiology. 2014;121:930-936. doi:10.1097/ALN.0000000000000430
- Rich S, Gubin S, Hart K. The effects of phenylephrine on right ventricular performance in patients with pulmonary hypertension. Chest. 1990;98:1102-1106. doi:10.1378/chest.98.5.1102
- Myles PS, Hall JL, Berry CB, et al. Primary pulmonary hypertension: prolonged cardiac arrest and successful resuscitation following induction of anesthesia for heart–lung transplantation. J Cardiothorac Vasc Anesth. 1994;8:678–681. doi:10.1016/1053-0770(94)90203-8
- Helviz Y, Einav S. A systematic review of the high-flow nasal cannula for adult patients. Crit Care. 2018;22(1):71. doi:10.1186/s13054-018-1990-4
- Mosier J, Joshi R, Hypes C, Pacheco G, Valenzuela T, Sakles J. The Physiologically Difficult Airway. Western Journal of Emergency Medicine. 2015;16(7):1109-1117. doi:10.5811/westjem.2015.8.27467
- Lentz S, Grossman A, Koyfman A, et al. High-Risk Airway Management in the Emergency Department. Part I: Diseases and Approaches. J Emerg Med. 2020;59(1):84-95. doi:10.1016/j.jemermed.2020.05.008
- Johannes J, Berlin D, Patel P et al. A Technique of Awake Bronchoscopic Endotracheal Intubation for Respiratory Failure in Patients With Right Heart Failure and Pulmonary Hypertension. Crit Care Med. 2017;45(9):e980-e984. doi:10.1097/ccm.0000000000002586
- Kuhn B, Bradley L, Dempsey T, Puro A, Adams J. Management of Mechanical Ventilation in Decompensated Heart Failure. J Cardiovasc Dev Dis. 2016;3(4):33. doi:10.3390/jcdd3040033
- Viitanen A, Salmenpera M, Heinonen J. Right ventricular response to hypercarbia after cardiac surgery. Anesthesiology. 1990;73:393–400. doi:10.1097/00000542-199009000-00005
- Grant C, Richards J, Frakes M, Cohen J, Wilcox S. ECMO and Right Ventricular Failure: Review of the Literature. J Intensive Care Med. 2020;36(3):352-360. doi:10.1177/0885066619900503
- Kostura M, Smalley C, Koyfman A, Long B. Right heart failure: A narrative review for emergency clinicians. Am J Emerg Med. 2022;58:106-113. doi:10.1016/j.ajem.2022.05.030









3 thoughts on “Right Heart Failure in the ED: Approach to Diagnosis and Management”
Very interesting topic
It would be awesome to have your opinion about these aspects below…
Since I’ve never seen a pulmonary vasodilators stocked in the EDs I’ve worked, can nebulized nitroglycerine have some utility? I’m surely thinking about the PE patient, but also the copd patient with signs of RHF rather than copd exacerbation.
Is norepi really the pressor of choice or can it worsen pulmonary vascular resistance??..Someone suggests to consider other pressors for this reason
Thank you by an italian ED doc
Pingback: Quiz 169, November 25th, 2022 – The FOAMed Quiz
Buongiorno. Thanks for reading.
Pulmonary vasodilators like epoprostenol or treprostinil are primarily reserved for patients with pulmonary arterial hypertension (Group 1 PH) who are on chronic infusions of these medications. If their infusion is interrupted they will crash quickly. So if you work in a community where these patients live, it’s important to have quick access to these medications. Outside of patients with Group 1 PH / pulmonary arterial hypertension, IV prostaglandins have not been well studied. So they are not recommended at this point for patients with a PE or COPD. I did not come across any high level evidence for nebulized nitroglycerin. If you have access to inhaled Nitric Oxide this may be helpful in your crashing PE patient, but discuss with the intensivist. The benefit of inhaled NO, is that it helps improve V/Q mismatch which might be seen in a pulmonary embolism.
Norepinephrine is first line because it has the least chance of worsening pulmonary vascular resistance (especially at low doses), in comparison to other vasopressors such as phenylephrine. However, hypotension makes everything worse in RHF, so if all you have access to is epinephrine you could give it a try.
I hope this helps.
Cheers,
Matt Kostura