Originally published on Ultrasound G.E.L. on 6/19/17 – Visit HERE to listen to accompanying PODCAST! Reposted with permission.
Follow Dr. Michael Prats, MD (@PratsEM), Dr. Creagh Bougler, MD (@CreaghB), and Dr. Jacob Avila, MD (@UltrasoundMD) from Ultrasound G.E.L. team!
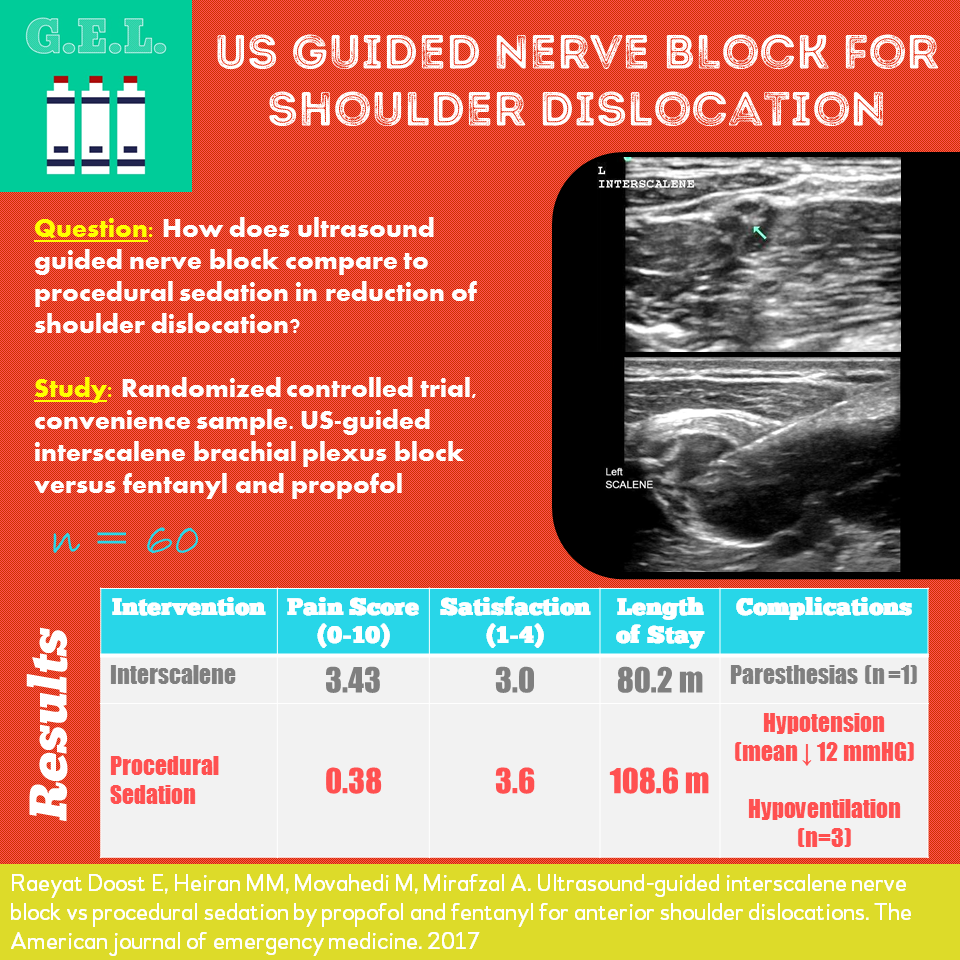
Ultrasound-guided interscalene nerve block vs procedural sedation by propofol and fentanyl for anterior shoulder dislocations
Am J Emerg Med April 2017 (Epub) – Pubmed Link
Take Home Points
1. US guided interscalene block led to decreased length of stay compared to procedural sedation for shoulder dislocation reduction (80.2 vs 108.6 minutes).
2. US guided interscalene block led to worse pain and satisfaction scores.
3. Both groups had few significant side effects.
Background
Shoulder dislocations are super duper common. There are several options for facilitating a potentially painful reduction including intraarticular anesthesia, relaxation maneuvers, and regional anesthesia BUT it seems that most people go to procedural sedation for this purpose. Depending on the agents used, this poses the potential risk of airway compromise, aspiration, apnea from oversedation, and hypotension. An alternative is to use an interscalene brachial plexus nerve block to numb the shoulder and allow for painless reduction. The use of ultrasound makes this even safer. In this study, they compare using an ultrasound guided interscalene nerve block to using procedural sedation and analgesia looking at pain and length of stay, as well as other secondary outcomes.
We previously covered an article looking at ultrasound for diagnosing shoulder dislocation, reduction, and associated fractures – check that out here
Questions
Does performing an ultrasound guided interscalene nerve block for shoulder dislocation reduce length of stay compared to procedural sedation?
Is there a difference in pain?
Is there a difference in # of reduction attempts, # of techniques, complications, or patient satisfaction?
Population
Level 2 trauma center in large city in Iran
Inclusion
- Isolated anterior shoulder dislocation during 11 months of enrollment (1/30/16 – 12/29/16) diagnosed on xray while the researchers were working
- Adults ≥ 18 yo
Exclusion
- Any contraindications to the study medications
- Medical conditions that made either group not feasible
- Neurovascular compromise related to dislocation
- Concomitant fracture
- Patient refusal to participate
Design
Randomized control trial
Convenience sample
Randomization blocks of 6 patients
Primary Outcomes:
- Length of stay (from beginning of procedure to discharge)
- Pain score during reduction
Secondary Outcomes:
- Total number of attempts at reduction
- Number of techniques used for reduction
- Occurrence of complications
- Patient satisfaction
Intervention
Both groups
- full upper extremity neuro exams
- Xray obtained
- No analgesics given before intervention
- Randomized to intervention or control
Interscalene brachial plexus block (ISBPB) (Intervention)
- see “Scan” below
Procedural sedation and Analgesia (PSA)(Control)
- 2 microgram/kg fentanyl AND 1 mg/kg of propofol
- Titrated to sedation
Reduction Attempts were standardized:
- First Liedelmeyer technique (external rotation in adduction), one attempt by resident, if failed then one attempt by attending
- If that failed, then Milch maneuver, one attempt by resident, if failed then one attempt by attending
- If that also failed, finally attempted traction-countertraction maneuver, one attempt by resident, if failed then one attempt by attending
All complications were recorded, including:
- respiratory depression
- hypotension
- systemic effects of lidocaine
- hypersensitivity
- sensori-motor deficits
Who did the scans?
Two board certified EM attending physicians
2 day training course AND 1 year experience with ISBPB with 1 weekly nerve block in this period
The Scan
High frequency linear probe

15-25 mL of 1% lidocaine and 0.1 mg epinephrine
Check out this great video on how to do an interscalene nerve block
Results
60 patients enrolled, 30 intervention, 30 control
- 96.7% men (58/60)
- Mean age 28.7 yo
- 83% were recurrent, 17% were first time
Primary Outcomes
Mean ER lengths of stay (measured from time of ISBPB or PSA to discharge)
PSA: 108.6 minutes
ISBPB: 80.2 minutes
Pain (scale 0-10)
PSA: 0.38
ISBPB: 3.43
Secondary Outcomes
Satisfaction (scale 1-4)
PSA: 3.6
ISBPB: 3.0
Number of Attempts *No statistically significant difference
PSA: 1.2
ISBPB: 1.4
Number of Techniques *No statistically significant difference
PSA: 1.13
ISBPB: 1.16
Neurovascular Complications:
PSA: 0
ISBPB: 0
Other Complications/Side Effects:
PSA: drop in SBP of 12 mm Hg mean, 3 pts with hypoventilation (transient)
ISBPB: 1 pt with body numbness and tongue paresthesia, attributed to systemic toxicity (did not last more than 1 hour)
Limitations
Not blinded (for obvious reasons)
Convenience sample – missed 83 patients because investigators were not present
Physicians had fairly good experience with ultrasound guided nerve blocks (1 per week for 1 year)
Took place in Iran – external validity questionable as there may be cultural and systems differences in factors affecting length of stay, pain, and satisfaction.
Fairly limited sample size – with only 30 patients in each group, it is hard to compare the incidence of rare serious side effects
Pain score presumably assessed after the procedure. Given that the PSA control group was a) sedated and b) given an agent with amnestic properties (propofol), it is not really a fair comparison to the awake procedure of a nerve block. On the other hand, if you are considering from a patient-centered standpoint, if that is the pain they remember, perhaps that is what is important.
Take Home Points
1. US guided interscalene block led to decreased length of stay compared to procedural sedation for shoulder dislocation reduction (80.2 vs 108.6 minutes).
2. US guided interscalene block led to worse pain and satisfaction scores.
3. Both groups had few significant side effects.
Our score
Cite this post as
Michael Prats, MD. Ultrasound Guided Nerve Block for Shoulder Dislocations. Ultrasound G.E.L. Podcast Blog. Published on June 19, 2017. Accessed on September 04, 2020. Available at https://www.ultrasoundgel.org/22.