Authors: Joshua J. White, DO (EM Resident Physician, Christus Spohn/Texas A&M, Corpus Christi, TX); J.D. Cambron, DO (EM Attending Physician, Pella Regional Health Center, Pella, IA); and Craig Pedersen, DO ( EM Attending Physician, Christus Spohn/Texas A&M, Corpus Christi, TX // Reviewed by: Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit); Alexander Y. Sheng, MD, MHPE (@TheShenger)
Cases
#1: A 62-year-old male presents to the emergency department (ED) from a company barbeque with coughing, dyspnea and painful swallowing after eating a piece of fish. The patient complains of “something stuck in his throat.” There is a mild inspiratory stridor present and the patient appears to be in mild distress. X-ray of soft tissue neck appears to demonstrate a radiopaque foreign body within the patient’s vallecula (Figure 1).

(Case Courtesy of Dr. Cole Seaton, Corpus Christi, TX)
#2: After successful retrieval of the previously mentioned foreign body, your next patient arrives at the ED. A 66-year-old male with a past medical history of dementia and Parkinson’s disease arrives from a nursing home after an episode of choking and is currently in severe respiratory distress.
#3: In the next room a 6-month-old healthy female presents from home with stridor and ongoing cough. Mother states that she left the child in a room with her older sibling and when she returned the child had developed the above symptoms. Mother notes that the older sibling had been playing with collector coins and likes to share with the younger sibling. The child is currently tachypneic. Initial two view chest x-ray demonstrates a circular metallic density over the thoracic inlet lying within the sagittal plane.
Questions
1) How should we evaluate and work up suspected foreign bodies?
2) When should foreign bodies be removed in the ED vs. managed in the OR?
3) What equipment do you need to manage an airway with a foreign body?
Introduction
Foreign body aspiration is a common complaint when presenting to the ED. In the United States from 2001-2009 an average of 12,435 children/year with ages ranging from 0-14 years presented to the ED with this complaint (1). Aspiration of a foreign body is the 3rd most common cause of death due to unintentional injury in children less than 1 year old in the United States(2). Although children account for most of foreign body aspiration cases, adults make up to 25% of these incidents (3). Developmentally delayed individuals are at a higher risk to aspirate foreign bodies. Those with impaired swallowing, chronic sedative, alcohol use and the elderly are at increased risk (3). Of aspirated foreign bodies approximately 20% affect the upper airway which includes the nasopharynx, oropharynx, laryngopharynx and also the trachea according to some sources. The remainder are lodged in mainstem or lobar bronchus(4,5). Children are more likely to have upper airway foreign bodies due to relative anatomical narrowing of the tracheobronchial tree(6,7).
Presentation
Upper airway foreign body aspiration has an heterogenous presentation depending on a variety of factors. These factors include the age of the patient, degree of airway obstruction, location of foreign body and how long the foreign body has been present. As mentioned previously, children are more likely to have upper airway foreign bodies and they are more likely to have a foreign body obstruct their airway. Aspirated objects that cause complete airway obstruction are much more rare and typically present as respiratory distress with signs of choking, stridor and drooling that requires immediate intervention and is more easily diagnosed(8). Conversely, distal airway foreign bodies are more likely to present with more subtle signs such as the classic diagnostic triad of wheezing, coughing, and decreased breath sounds. Although this triad is a classic presentation, a review of upper airway foreign bodies by Wiseman et al. noted that this triad was present in less than half the cases reviewed, and incomplete triad presentation is more common(9).
Diagnosis
If the patient’s clinical status allows it, then imaging is indicated to confirm a suspected diagnosis of an upper airway foreign body. Initial recommended imaging includes chest x-ray PA and lateral inspiratory-expiratory films(3,10). This may identify radiopaque foreign bodies and might identify air trapping further localizing the suspected foreign body. However, in up to 25-50% of airway foreign bodies, x-rays may be normal in appearance(11). In patients who are stable and cooperative, using CT to diagnose foreign body aspiration has shown to be beneficial to avoid unnecessary bronchoscopies(12,13). It also decreases the likelihood of delays in diagnosis and can help triage patients to determine need for transfer to another hospital. Gordon et al. demonstrated success in using ultralow-dose CT with a tin filter to diagnose foreign bodies to minimize radiation exposure (14). If the patient is too unstable for CT, then direct or video laryngoscopy can be initiated next in an effort to locate and remove foreign body(15). 5 mL of 4% nebulized lidocaine can be administered to cooperative patients to attenuate the gag-reflex to enable laryngoscopy on awake patients(16). Otherwise, procedural sedation is recommended prior to laryngoscopy to ensure optimal chance of success. Once the diagnosis is confirmed through direct visualization, removal can be attempted in the ED.


Management

Hemodynamically stable algorithm
Management of upper airway foreign bodies varies depending on the stability of the patient. Like every patient in the ED, a patient with a suspected foreign body should be assessed starting with vital signs, the primary survey and a brief history and physical. In patients who are hemodynamically stable and protecting their airway, recommendations for management includes the following:
1. Obtain diagnostic imaging starting with CXR AP/Lateral.
- If the foreign body is identified, usually further imaging is not indicated.
- If foreign body is not identified, CT should be considered to avoid unnecessary bronchoscopies, and to further localize foreign body.
2. If no foreign body is identified, suggested management depends on level of suspicion of foreign body.
- If there is high level of suspicion, bronchoscopy is indicated as it remains the Gold Standard for diagnosis even though sensitivity of CT approaches 100%.
- If there is low suspicion, other diagnosis should be considered, but follow up is suggested as many presentations are subtle including a single non-specific symptom as cough.
- An episode of choking followed by coughing is the most common presentation for an airway foreign body aspiration in children(19). If an episode of choking is elicited while obtaining history, suspicion of an aspirated foreign body should be heightened, and bronchoscopy should be considered.
3. If foreign body is identified in the lower airway, consult for bronchoscopy is recommended.
- Performing bronchoscopy in the emergency department is not recommended if the patient is stable. Early consultations to medical specialists to perform bronchoscopy is recommended where a more controlled environment in the operating room (OR) is able to be performed.
4. If foreign body is identified in the upper airway, attempt removal with laryngoscopy.
- If foreign body is identified above the glottis, then laryngoscopy may be successful in removing foreign body. If it cannot be removed, consultation for bronchoscopy is suggested.
- 5 mL of 4% nebulized lidocaine can be administered to cooperative patients to attenuate the gag-reflex to enable laryngoscopy on awake patients. If patient is unable to tolerate awake laryngoscopy, use sedation to ensure comfort. Ketamine can be used as sedation; however, it induces hypersalivation making foreign body retrieval more difficult at times. You may want to suggest giving Glycopyrrolate (0.1-0.2mg IV) or Atropine (0.5mg IV) to aid in inhibition of salivation and secretions during procedure. Both of these are given 20-30 minutes prior to procedure and would only apply to hemodynamically stable algorithm.
- During initial laryngoscopy, forceps should be available to remove foreign bodies if visualized. In some cases, even suction is enough to remove the foreign body. Useful instruments for foreign body retrieval include Magill, Sponge stick or Alligator forceps. (Figures 5-7).

- While preparing for the procedure, you might have to get the Magill forceps from the OBGYN tray, and alligator forceps from the ENT tray. Additional tools can be obtained from the OR if time permits.
- One study performed by Higgins et. Al. compared Magill (Figure 6) and sponge stick forceps (figure 7) and found sponge stick forceps to be more favorable in foreign body retrieval during laryngoscopy(20).
- Another study performed by Je et Al. compared the use of Glidescope vs Macintosh blade in the removal of foreign bodies and found use of Macintosh blade led to easier and quicker retrieval of foreign bodies with fewer attempts(21). Some newer generation glidescopes and Carl Storz C-mac blades use standard geometry mimicking direct laryngoscopy. This makes foreign body retrieval easier and if necessary, these blades can be used for direct laryngoscopy if the camera becomes contaminated.
5. If foreign body removal with laryngoscopy is successful, consider discharge if there were no complications and if patient has no other complaints.
- After successful removal, confirm removal via laryngoscopy or imaging as indicated if there is suspicion for more foreign bodies.
Hemodynamically unstable algorithm
As with routine emergency care, initial airway management is critical as patients can present with hypoxia due to airway obstruction.
1. If patient is or becomes unconscious, CPR should be initiated in an attempt to clear the patient’s airway.
2. If patient is conscious and in respiratory distress, or if the patient is already unconscious, inspect the patient’s airway with laryngoscopy.
- If you are able to visualize the foreign body above the glottis, attempt removal with suction or available forceps.
3. If removal is successful, reassess the patient for respiratory distress or any hemodynamic instability.
- If not stable, obtain a definitive airway. Consider using a larger endotracheal tube (8-0 is preferable) to enable future bronchoscopy.
- If foreign body relieved distress, and patient is back to baseline, consider observation and for further evaluation given initial critical presentation.
4. If retrieval of the foreign body is unsuccessful, intubate around foreign body or if able force foreign body down one of the mainstem bronchi in order to maintain an airway (figure 8).
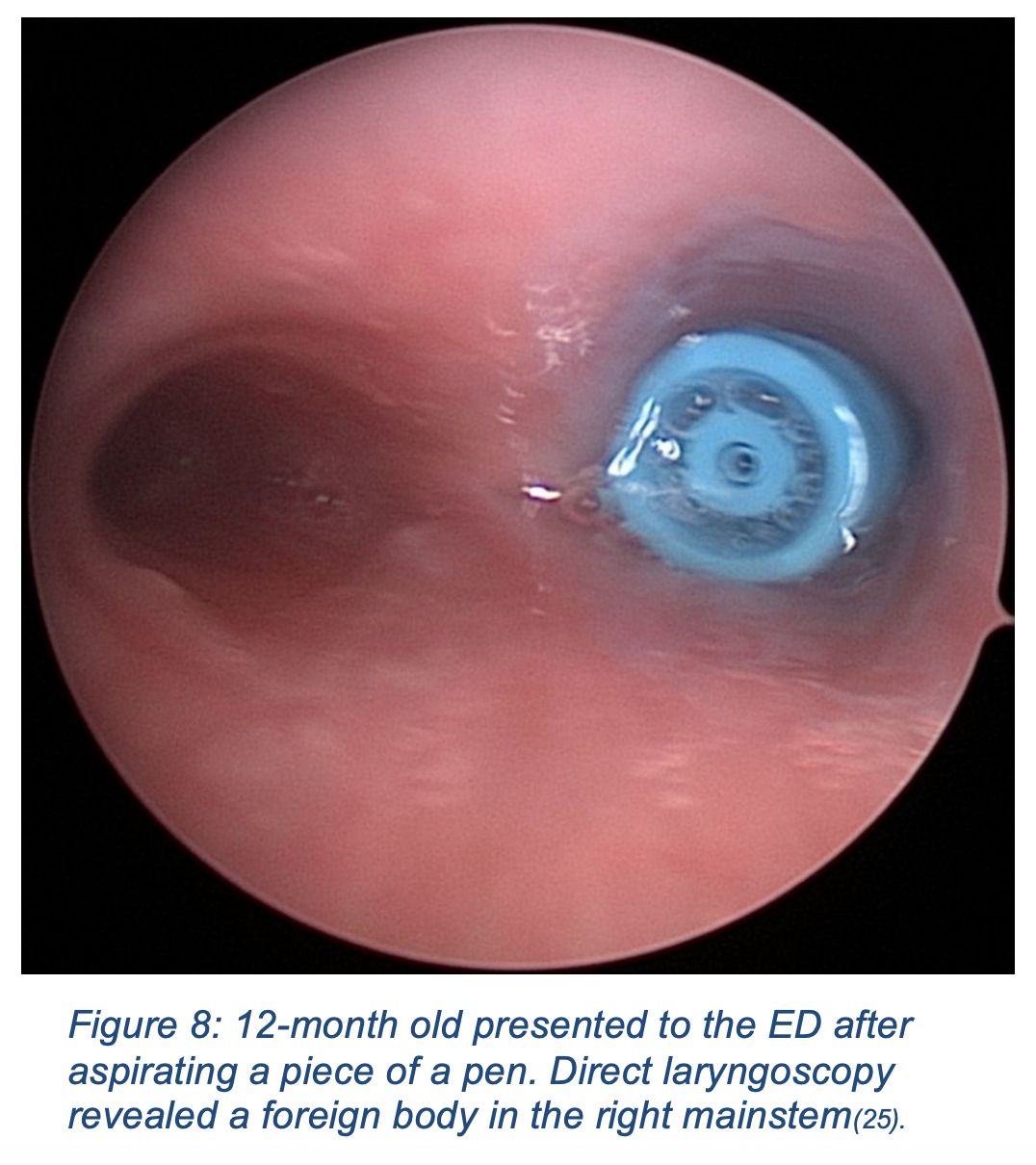
- If the foreign body cannot be removed in the setting of respiratory compromise, definitive airway management is indicated. Intubation around the foreign body or forcing the foreign body into one of the mainstem bronchi should be attempted(10,25).
- Although supraglottic devices for airway management are usually a reasonable option, it should be avoided in the hypoxic patient with a suspected foreign body. This is due to the possibility of a foreign body obstructing the airway distal to the supraglottic device which would provide no benefit and lead to probable harm for the patient. Direct or video laryngoscopy with subsequent endotracheal intubation is the preferred management for patients who are hypoxic with suspected foreign body aspiration or who have complete airway obstruction.
5. If you are able to obtain a definitive airway, next consult for bronchoscopy to remove foreign body.
6. If unable to intubate patient, perform a cricothyrotomy if foreign body is above the patient’s glottis. If it is below the glottis, cricothyrotomy has no benefit and ENT should be consulted emergently.
Disposition
There is a paucity of literature specifying recommendations regarding patient disposition and discretion is deferred to the emergency medicine provider and specialty consultation’s clinical judgment. If the patient is stable and the foreign body is successfully removed, it is reasonable to discharge the patient after a short period of observation. In a patient that was in distress, or experienced hemodynamic instability prior to successful removal, admission to the hospital for further observation is a reasonable disposition. Even patients’ that have negative imaging may be considered for admission and bronchoscopy if suspicion is high. This especially applies to children as there can be delays in diagnosis and a complete history may be difficult to obtain.
Case Conclusions
1. CT confirms a metallic object traversing the patient’s supraglottic airway with partial embedment into the vallecula. After receiving ketamine, the patient undergoes evaluation with Glidescope video laryngoscopy, and the foreign body is retrieved via Alligator forceps (Figure 9). After foreign body removal, the patient was discharged home with no complications.

2. Hypoxia was present with pulse oximetry of 75% and very little air movement to lungs bilaterally. Patient was given a dose of Ketamine and a Brussel sprout foreign body was removed from the upper airway via Magill forceps. The patient’s clinical presentation improved post removal, and the patient was admitted to the hospital for observation given his initial critical presentation.
3. Foreign body was identified below the patient’s glottis and pediatric Pulmonology was consulted who successfully removed a button battery from the patient’s trachea via rigid bronchoscopy in the OR with no complications. The patient was observed in the hospital for 24 hours and subsequently discharged.
References / Further Reading
- Chapin MM, Rochette LM, Annest JL, Haileyesus T, Conner KA, Smith GA. Nonfatal choking on food among children 14 years or younger in the United States, 2001-2009. Pediatrics. 2013 Aug;132(2):275-81.
- WISQARS leading causes of death reports. Cdc.gov. Accessed October 20, 2020. https://webapp.cdc.gov/sasweb/ncipc/leadcaus10.html
- Hewlett JC, Rickman OB, Lentz RJ, Prakash UB, Maldonado F. Foreign body aspiration in adult airways: therapeutic approach. J Thorac Dis. 2017;9(9):3398-3409.
- Lucia D. Respiratory Distress. Current Diagnosis & Treatment: Emergency Medicine. 2017;8e.
- Tintinalli JE, Stapczynski JS, John O, Cline DM, Yealy DM, Meckler GD. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 8th ed. McGraw-Hill Professional; 2015.
- Cramer N, Jabbour N, Tavarez MM, Taylor RS. Foreign Body Aspiration. In: StatPearls. StatPearls Publishing; 2020.
- Salih AM, Alfaki M, Alam-Elhuda DM. Airway foreign bodies: A critical review for a common pediatric emergency. World J Emerg Med. 2016;7(1):5-12.
- Rose D, Dubensky L. Airway foreign bodies. In: StatPearls. StatPearls Publishing; 2020.
- Wiseman NE. The diagnosis of foreign body aspiration in childhood. J Pediatr Surg. 1984 Oct;19(5):531-5.
- Wormley M. Foreign-Body Aspiration. Emra.org. Accessed on 10/7/2020. https://www.emra.org/emresident/article/foreign-body-aspiration-a-pediatric-airway-emergency/ Accessed on 10/7/2020.
- Hsiang-Jer Tseng TN. Hanna WS, Majid Aized FK, Linnau KF. Imaging Foreign Bodies: Ingested, Aspirated, and Inserted. Annals of Emergency Medicine. 2015. 66(6):570-82
- Gibbons, AT. et al. Avoiding unnecessary bronchoscopy in children with suspected foreign body aspiration using computed tomography. Journal of Pediatric Surgery. 2020. 55(1):176-81
- Gordon L, Nowik P, Mobini Kesheh S, Lidegran M, Diaz S. Diagnosis of foreign body aspiration with ultralow-dose CT using a tin filter: a comparison study. Emerg Radiol. 2020 Aug;27(4):399-404.
- Sakaida H, Chiyonobu K, Ishinaga H, Takeuchi K. Use of a Rigid Curved Laryngoscope for Removal of a Fish Bone in the Hypopharynx. Case Rep Otolaryngol. 1155/2016/9689521;2016(9689521). doi:10.
- Nickson C. Awake Intubation. Litfl.com. Published January 1, 2019. Accessed on 10/16/2020. https://litfl.com/awake-intubation
- Patel MS. Airway foreign body in child. Radiopaedia.org. Accessed October 10, 2020. https://radiopaedia.org/cases/airway-foreign-body-in-child-1.
- Steel D. Airway Foreign Body. Radiopaedia.org. Accessed on 10/10/2020. https://radiopaedia.org/images/26465123?case_id=49402
- Even L, Heno N, Talmon Y, Samet E, Zonis Z, Kugelman A. Diagnostic evaluation of foreign body aspiration in children: a prospective study. J Pediatr Surg. 2005 Jul;40(7):1122-7.
- Higgins GL 3rd, Burton JH, Carter WP, Floor AE. Comparison of extraction devices for the removal of supraglottic foreign bodies. Prehosp Emerg Care. 2003 Jul-Sep;7(3):316-21.
- Je SM, Kim MJ, Chung SP, Chung HS. Comparison of GlideScope(®) versus Macintosh laryngoscope for the removal of a hypopharyngeal foreign body: a randomized cross-over cadaver study. Resuscitation. 2012 Oct;83(10):1277-80.
- Image of Nasal forceps. Anthonyproducts.com. Accessed on 10/20/20. https://www.anthonyproducts.com/store/nasal-forceps-3
- Image of Magill forceps. Litfl.com. Accessed on 10/20/20. https://litfl.com/wp-content/uploads/2019/01/Magill-forceps.jpeg
- Image of Sponge stick forceps. Surgicaltools.com. Accessed on 10/20/20. https://www.surgicaltools.com/3909/foerster-ballenger-sponge-forceps-18cm-curved
- Chaffin PL, Grischkan JM, Malhotra PS, Jatana KR. Endoscopic management of pediatric airway and esophageal foreign bodies. In: Endoscopy – Innovative Uses and Emerging Technologies. InTech; 2015.








