Authors: Brit Long, MD (@long_brit, EM Attending Physician, SAUSHEC) and Kristen Kann, MD (EM Attending Physician, SAUSHEC) // Edited by: Alex Koyfman, MD (@EMHighAK, EM Attending Physician, UT Southwestern Medical Center / Parkland Memorial Hospital)
A 44-year-old male presents to the ED with wheezing and respiratory distress. His vital signs include BP 200/120, HR 132 bpm, RR 28, T 97 F, and SpO2 88% on room air. He is diaphoretic, and exam demonstrates wheezes throughout all lung fields. He has a history of asthma, though he has never been admitted for asthma. You give him a continuous nebulizer treatment for one hour, with IV steroids. After the hour, he does not improve. Are there other conditions that could account for his symptoms?
Background
Asthma accounts for 1.8 million ED visits and 439,000 admissions annually in the U.S.1 The disease affects 1 in 11 children and 1 in 12 adults in the U.S.1 Asthma lacks a clear definition, despite it being a common disease. The Global Initiative for Asthma defines it as “a heterogeneous disease, usually characterized by chronic airway inflammation. It is defined by the history of respiratory symptoms such as wheeze, shortness of breath, chest tightness, and cough that vary over time and in intensity, together with variable expiratory airflow limitation.”2
An asthma exacerbation often presents with wheezing and prolonged expiration. Patients with severe respiratory distress may present in a tripod position, leaning forward. The most dangerous lung sound is the absences of air movement, which is due to severe bronchoconstriction or patient exhaustion.
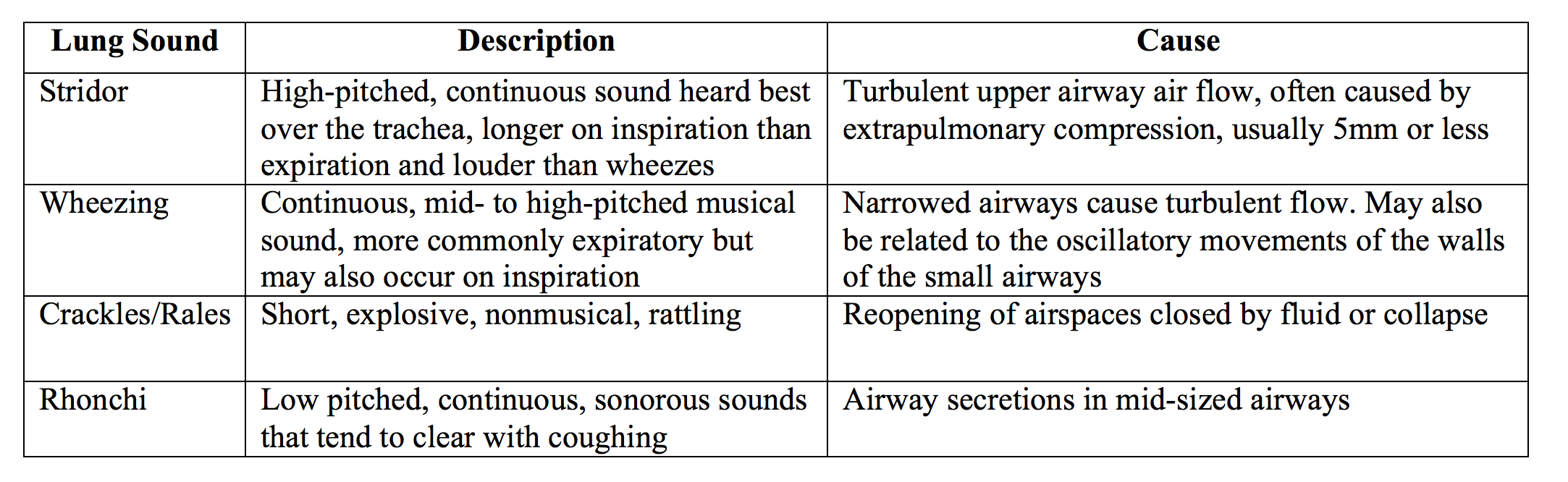
There are many mimics of asthma, especially conditions that present with wheezing. Some patients may present with no wheezing. In one study, 92% of patients with asthma report obstructive feelings like wheezing.3 Over 75% of COPD patients and nearly 30% of patients with cardiac pathology experience similar symptoms.3 Airways narrow through swelling, compression, and intrinsic compression, and this narrowing with turbulent air flow can result in wheezing. Emergency physicians should be aware of conditions that can result in similar symptoms. Lung findings on exam are explained below.
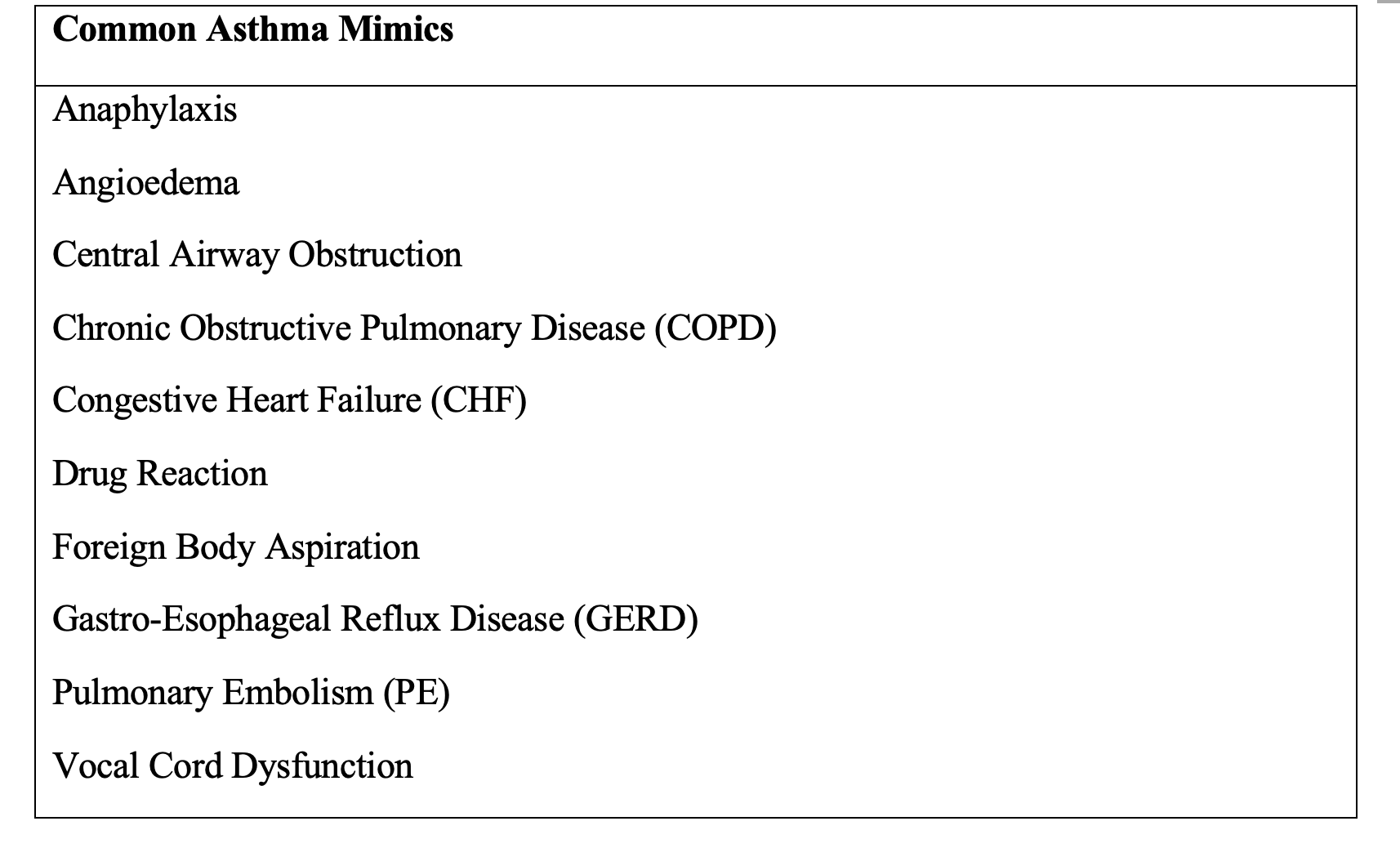
Asthma Mimics
Anaphylaxis: This condition presents with similar pathophysiology as asthma with hyperactive immune response and bronchoconstriction. It accounts for close to 1% of ED visits, though onset of symptoms is more acute than in asthma with history of exposure to an allergen. Anaphylaxis involves two organ systems or a known allergic exposure with low blood pressure. Exam usually reveals urticaria (10-20% will not have rash), and nausea, vomiting, or diarrhea may also be observed. Treatment requires immediate resuscitation with epinephrine, steroids, intravenous (IV) fluids, and histamine antagonists. Any concern for anaphylaxis warrants intramuscular epinephrine.4
COPD: COPD classically has been thought to be irreversible and associated with tobacco use. Like asthma, it is an obstructive airway disease. The CHAIN study described Asthma-COPD Overlap Syndrome (ACOS or ACO). In this study, 15% of patients with COPD have features of asthma, while 15% of patients with asthma have COPD.5,6 Official diagnosis is often done by pulmonologist, though asthma is usually diagnosed in young adulthood and COPD usually after age 40 with history of bronchodilator responsiveness, though these are not completely reliable.5 Initial treatment of COPD is similar to asthma, though long term medication management differs (such as Long Acting Beta Agonists (LABA) in COPD improving mortality). In asthma, LABA use may increase mortality if used without inhaled steroids.7
Heart Failure: Heart failure may result in wheezing with lung fluid accumulation. Some patients may not be diagnosed with heart failure upon initial presentation, and patients may present acutely with respiratory distress or with chronic worsening orthopnea and dyspnea (the most common presentation). Flash pulmonary edema (the acute version) can be due to ischemia, acute valvular pathology, cardiomyopathy, and other conditions. Exam may reveal rales, S3 heart sound, elevated JVP, and edema. Patients may have a history of dyspnea with exertion or with lying flat. Acute exacerbation with pulmonary edema requires venodilators and positive pressure ventilation (CPAP or BiPAP). However, treatment should be tailored to the patient. Diuretics can be used after venodilation.8 The underlying etiology should be treated as well.
PE: PE is not always an easy diagnosis, though emergency physicians evaluate patients with potential PE on a regular basis. Close to 1 in 10 patients with PE may have wheezing on exam.9 This may be due to vasoactive mediators released in response to the embolus.10 The key is to evaluate for PE risk factors in the history. If patients do not improve with standard asthma medications, PE should also be considered. Evaluation includes risk stratification such as Wells criteria, with D-dimer and CT pulmonary as needed. Significant PE requires anticoagulation.11
Foreign body aspiration: A small object in the bronchioles from aspiration can result in focal lung finds, and worse, respiratory distress. Patients with greatest risk for this include children, older adults, and those mentally disabled. Patients may present with acute cough or wheezing. The classic history is lack of preceding upper respiratory symptoms or prior wheezing.12 Choking followed by cough is present in 75% of pediatric patients with foreign body aspiration. Chest x-ray can help, erect and lateral, which may show hyperinflation. Bronchoscopy is required if concern for aspiration, even with negative chest x-ray.13
Angioedema: “Angioedema” refers to localized swelling in locations with loose connective tissue, including the face, oropharynx, bowel wall, extremities, and genitalia. There are many causes. Primary pathology includes mast cell-mediated and bradykinin-mediated. Mast-cell mediated angioedema can have other signs of allergic reaction such as urticaria. Bradykinin-induced angioedema is not associated with urticaria and pruritis, as it is not allergic. This form is the cause in ACE-inhibitor-induced angioedema and Hereditary Angioedema (HAE).14 Angioedema associated with systemic findings such as upper airway swelling, wheezing, abdominal pain, nausea, and vomiting should be managed as anaphylaxis until proven otherwise and treated with epinephrine, antihistamines, and corticosteroids. Rapid airway protection with intubation may be required, and a difficult airway should be assumed with adjuncts available.
Drug Related Wheezing: This is most commonly associated with aspirin. Aspirin Exacerbated Respiratory Disease, or Samter’s Triad, consists of asthma, nasal polyps, and sensitivity to aspirin or other NSAIDs.15 Non-selective beta-blockers can precipitate wheezing in patients with underlying disease (such as asthma).16 ACE-inhibitors, while commonly causing dry cough, may result in bronchospasm and wheezing.17 Many drugs can cause asthma symptoms, or worsen asthma in patients with known disease. The risks and benefits of continuing aspirin or an NSAID must be strongly considered, or an alternative can be used.
Central Airway Obstruction: Obstruction in the trachea and main stem bronchi include bronchogenic carcinomas, tracheal strictures, sarcoidosis, and goiter. Though these usually do not present acutely, patients may notice other symptoms including weight loss. If the obstruction is fixed, wheezing will likely be constant and fixed. Asthmatic wheezing usually occurs after exposure to allergen or upper respiratory infection. Wheezing due to fixed obstruction may be localized on exam.18 Further evaluation and testing relies on the history and exam. Risk factors for cancer, symptoms consistent with hyperthyroidism, or a history of intubation should be obtained. Chest CT will most likely identify the obstruction, though the patient must be able to lie supine. Further consultation is required if diagnosed, with bronchoscopy as well.19
Vocal Cord Dysfunction: Paradoxical, involuntary closure of the vocal cords during inspiration, (or edema of the vocal cords) may result in wheezing and acute respiratory distress. Wheezing in this condition is usually inspiratory or inspiratory and expiratory (asthmatic wheezing is mostly expiratory). This is due to forced expiration stenting open the cords and decreasing the obstruction. Patients often present soon after exposure to a stressor, inhaled irritants, or exercise. Risk factors include prior intubation or neck surgery (leading to possible damage to the recurrent laryngeal nerve). Diagnosis is often confirmed through laryngoscopy. Treatment of vocal cord dysfunction includes several maneuvers. Panting, which can abduct the vocal cords through activation of the posterior cricoarytenoids,20 breathing through a straw, patient jaw thrust while breathing, nose to mouth breathing,21 administration of a helium-oxygen mixture such as heliox,22 or continuous positive airway pressure (CPAP) can be used. The condition is often self-limited and usually does not require other invasive interventions.
Approach
The approach for asthma and asthma mimics is to first assess for life threats, provide emergent interventions, and then obtain history and focused exam. Rapid treatment with bronchodilator and corticosteroids is required.23-25 Non-Invasive Positive Pressure Ventilation (NIPPV) should be considered. This modality decreases mortality in COPD and CHF, though in asthma more literature is needed.24,25
Once treatment and initial stabilization have been completed, focused history and exam should be conducted to evaluate for mimics. As discussed, there are many causes of wheezing, and these conditions must be considered to prevent anchoring bias. Red flags for other conditions include absence of asthma history, prior history of mild asthma, or poor response to therapy.23 Most patients with asthma improve with treatment, as suggested in a retrospective study of over 13,000 patients.26-28
Patients who do not improve with asthma treatment including anticholinergic/beta-agonist nebulizer treatment, corticosteroids, magnesium, and further resuscitation measures require more evaluation such as ECG, imaging (x-ray, CT, or US), and laboratory studies. These measures may allow physicians to diagnose and treat another underlying disease.
Case Conclusion:
With poor response to asthma management, the emergency physician reassesses the patient and conducts a focused US of the lungs and heart. The US reveals diffuse B lines and poor ejection fraction. The BNP returns at 2,000, though the ECG and troponin are unactionable. Chest x-ray shows interstitial edema. The physician orders nitroglycerin 100 mcg/min IV infusion, and the patient is placed on NIPV and admitted.
Key Points:
– All that wheezes is not asthma.
– Asthma exacerbation often presents with wheezing and prolonged expiration, though respiratory distress may occur.
– Asthma is a common condition managed in the ED, but there are many mimics.
– A history of no asthma, or mild asthma, should raise concern that the current presentation may be due to some other condition.
– Mimics include anaphylaxis, heart failure, COPD, foreign body aspiration, vocal cord dysfunction, drug related wheezing, central airway obstruction, angioedema, or PE.
– Focused history and exam, with patient reassessment, are vital. Patients with no prior asthma, mild asthma, or little response to treatment require consideration of another cause.
References/Further Reading
- Asthma Fact Sheet. Centers for Disease Control and Prevention Web site. http://www.cdc.gov/asthma/impacts_nation/asthmafactsheet.pdf. Accessed 01 August, 2016
- 2015 Pocket Guide for Asthma Management. Global Initiative for Asthma Web site. http://ginasthma.org/wp-content/uploads/2016/01/GINA_Pocket_2015.pdf. Accessed 01 August, 2016.
- Elliott MW, Adams L, Cockcroft A, et al. The language of breathlessness. Use of verbal descriptors by patients with cardiopulmonary disease. Am Rev Respir Dis 1991; 144: 826 –32.
- Zilberstein J, McCurdy MT, Winters ME. Anaphylaxis. J Emerg Med. 2014; 47: 2 182-187.
- Cosio BG, Soriano JB, Lopez-Campos JL, et al. CHAIN Study. Defining the asthma-COPD overlap syndrome in a COPD cohort. Chest. 2016; 149; 45-52.
- Gibson PG, McDonald VM. Asthma-COPD overlap 2015: now we are six. Thorax. 2015; 70: 683-691.
- Nelson HS, Weiss ST, Bleeker ER, Yancey SW, Dorinsky PM. “The Salmeterol Multicenter Asthma Research Trial: a comparison of usual pharmacotherapy for asthma or usual pharmacotherapy plus salmeterol. Chest. 2006; 129(1): 15
- Mattu A, Martinez JP, Kelly BS. Modern Management of Cardiogenic Pulmonary Edema. Emerg Med Clin North Am, 23 (2005), pp.1105-1125
- Calvo-Romero JM, Pérez-Miranda M, Bureo-Dacal P. Wheezing in patients with acute pulmonary embolism with and without previous cardiopulmonary disease. Eur J Emerg Med 2003 Dec; 10(4): 288-9.
- W. J. Windebank, G. Boyd, and F. Moran. Pulmonary Thromboembolism Presenting as Asthma. Br Med J 1973 Jan 13; 1(5845): 90–94.
- Fesmire FM et al. Critical Issues in the Evaluation and Management of Adult Patients Presenting to the Emergency Department With Suspected Pulmonary Embolism. www.acep.org, accessed 08Sep2016.
- Wiseman NE. The Diagnosis of Foreign Body Aspiration in Childhood. J Pediatr Surg. 1984;19(5):531.
- Even L, Heno N, Talmon Y, Samet E, Zonis Z, Kugelman A. Diagnostic evaluation of foreign body aspiration in children: a prospective study. J Pediatr Surg 2005;40(7):1122.
- Wilkerson RG. Angioedema in the Emergency Department: An Evidence Based Review. Emergency Medicine Practice Nov 2012, vol 14 #11.
- Samter M and Beers RF Jr. Intolerance to Aspirin: Clinical Studies and Consideration of its Pathogenesis. Ann Intern Med. 1968;68(5):975
- Khosla S, Kunjummen B, Khaleel R, et al. Safety of therapeutic beta-blockade in patients with coexisting bronchospastic airway disease and coronary artery disease. Am J Ther 2003;10(1):48.
- Lunde H, Hedner T, Samuelsson O, Lötvall J, Andrén L, Lindholm L, Wiholm BE. Dyspnoea, asthma, and bronchospasm in relation to treatment with angiotensin converting enzyme inhibitors. BMJ 1994;308(6920):18.
- Ernst A, Feller-Kopman D, Becker HD, and Mehta AC. Central Airway Obstruction. Am J Respir Crit Care Med. 2004; 169(12):1278
- Stephens KE Jr, Wood DE. Bronchoscopic Management of Central Airway Obstruction. J Thorac Cardiovasc Surg. 2000;119(2):289.
- Pitchenik AE. Functional laryngeal obstruction relieved by panting. Chest 1991; 100(5): 1465.
- Denipah N, Dominguez CM, Kraai EP, Kraai TL, Leos P, Braude D, Acute Management of Paradoxical Vocal Fold Motion (Vocal Cord Dysfunction). Annals of Emergency Medicine In press as of 28 August, 2016. DOI: http://dx.doi.org/10.1016/j.annemergmed.2016.06.045.
- Weir M. Vocal cord dysfunction mimics asthma and may respond to heliox. Clin Pediatr (Phila) 2002; 41(1): 37.
- Rodrigo GJ, Rodrigo C, Hall JB. Acute Asthma in Adults: A Review. Chest. 2004;125(3):1081.
- Lim WJ, Mohammed Akram R, Carson KV, et al. Non-invasive positive pressure ventilation for treatment of respiratory failure due to severe acute exacerbations of asthma. Cochrane Database Syst Rev 2012;12:CD004360.
- Landry A, Foran M, and Koyfman A. Does noninvasive positive-pressure ventilation improve outcomes in severe asthma exacerbations? Annals of Emergency Med 2013 Vol62(6) pp 594-596.
- Chen W, Marra CA, Lynd LD, FitzGerald JM, Zafari Z, Sadatsafavi M. The natural history of severe asthma and influences of early risk factors: a population-based cohort study. Thorax 2016; 71: 3 267-275.
- Kelly WJ, Hudson I, Phelan PD, Pain MC, Olinsky SO. Childhood asthma in adult life: a further study at 28 years of age. Br Med J (Clin Res Ed) 1987; 294(6579): 1059
- Settipane GA, Greisner WA 3rd, Settipane RJ. Natural history of asthma: a 23-year follow-up of college students. Ann Allergy Asthma Immunol 2000; 84(5): 499.









3 thoughts on ““All that wheezes is not asthma” – an evaluation of asthma mimics”
Pingback: emDOCs.net – Emergency Medicine EducationGastroenteritis Mimics: What should the emergency physician consider? - emDOCs.net - Emergency Medicine Education
Pingback: SGEM#206: I’m Wheezy Like A Pre-Schooler – Prednisolone for Wheezy Children | The Skeptics Guide to Emergency Medicine
Pingback: November ’23 Asynchronous – Lakeland Health EM Blog