Authors: Stephanie Bartikoski (Medical Student, Uniformed Services University of the Health Sciences), Wells Weymouth (EM Resident, San Antonio, TX), and C.J. Winckler (Deputy Medical Director, San Antonio Fire Department EMS) // Edited by: Alex Koyfman, MD (@EMHighAK) and Brit Long, MD (@long_brit)

Figure 1. Whole Blood use in San Antonio, Texas.
Case
An ambulance is transporting a 27-year-old male who has been the victim of a stabbing. The radio operator tells you there is a penetrating wound to the left upper abdomen. Vitals show tachycardia with a heart rate of 130. Blood pressure is 105/60 during transport, but upon arrival it drops to 88/50. Hemothorax is noted on chest X-ray, and FAST is positive for fluid in the RUQ and LUQ windows. You anticipate the need for massive transfusion given a likely vascular injury. What blood products do you reach for?
Introduction
In the trauma setting, the most common cause of death within the first hour upon arrival to a trauma center is massive hemorrhage.1 The mortality of patients that need massive transfusion is greater than 50%, and up to 10% of these deaths are considered potentially survivable.2 Modern combat history has taught us much of what we know about the treatment of trauma and the tenets of resuscitation. The use of blood products, in addition to crystalloid solutions for traumatic injuries has deep roots in the last century of conflict. The military blood program primarily used whole blood (WB) from the 1940s until the 1960s, reaching its peak during the Vietnam War, when more than 1 million units of cold-stored WB was transfused by the military.3 Following this, there was a growing interest in the civilian sector to conserve blood as a vital resource and target specific component deficiencies, which resulted in WB being used more sparingly, and the subsequent rise of component therapy in the 1970s and 1980s.
Component therapy enabled increased storage times and offered a more tailored approach to resuscitation with decreased risk of infection. By 1990, trauma resuscitation nearly exclusively used component therapy. Management of trauma patients was centered on correcting of the lethal triad of acidosis, hypothermia, and coagulopathy by mitigating ischemia, rewarming, and administering large volume crystalloid fluids. Over the last decade, this approach has demonstrated significant improvement in mortality, most notably when blood products were administered rather than crystalloid solution.4
The concept of an Acute Coagulopathy of Trauma – Shock (ACoTS) was first described by Brohi et al. in the mid-2000s, which was discovered to be an independent marker of morbidity and mortality.5 This physiologic state caused many to begin to reconsider methods of fluid resuscitation. A large retrospective cohort study of patients wounded during Operation Iraqi Freedom and Operation Enduring Freedom showed that there was a significant survival benefit when a 1:1:1 ratio of RBCs, platelets, and fresh frozen plasma was transfused rather than the traditional large volumes of packed RBCs.6
Medical innovation and, in this case re-invention, was spurred by recent conflicts as the capabilities of state militaries extended from large scale urban battles to numerous, dispersed forward operating bases. Given the forward deployed nature of conflict and the demand to maintain a readily available blood supply where component therapy is logistically difficult, recent strategy has shifted back towards the use of fresh and stored whole blood (FWB and SWB).7 First pioneered by the Swedish and Norwegian militaries and later developed and implemented in the 75th Ranger Regiment, the Tactical Damage Control Resuscitation protocol for FWB collection and transfusion became the standard in the United States military.8 This military medicine advancement has permeated into the civilian sector with growing evidence that even partial use of WB can offer a survival advantage.9 This development has led some to endorse WB as the ideal resuscitation product in massive hemorrhage.10
What is Whole Blood?
It is important to distinguish between fresh whole blood (FWB) and stored whole blood (SWB). FWB, commonly known as a “walking blood bank”, is usable at room temperature for 24 hours or it can be refrigerated within 8 hours of collection, which is then considered stored whole blood (SWB).11 SWB can be stored at 1-6°C for twenty-one days in the anticoagulant citrate phosphate dextrose, or for thirty-five days in citrate phosphate dextrose adenine (CPDA-1).12,13 Whole blood is FDA approved for administration when appropriately collected in anticoagulants, then stored and tested for transfusion associated diseases.14 FWB is not approved by the FDA in the civilian setting because it does not undergo disease screening prior to administration (although many would argue this is unnecessary given military members are pre-screened for blood-borne disease), leaving SWB as the only solution to be used outside of the military. However, SWB has been shown to provide the same hemostatic effect as FWB at least in the short term.15
What are the Advantages of Whole Blood?
Despite an optimally balanced component therapy ratio of 1:1:1, the resulting blood mixture is diluted to a hematocrit of 29%, a platelet count of about 90,000/μL, and coagulation factors that are only 62% as concentrated when compared to WB.16 This is mostly due to the necessary anticoagulant agents and additive solution. WB also inherently contains platelets, which are challenging to store as a separated component due to a short shelf life, among other issues. While the transfusion of component therapy may lead to thrombocytopenia, one study in the Vietnam War revealed that up to six liters of WB can be transfused without diluting platelets below normal counts.17 Another study showed that one unit of stored FWB had the same hemostatic effect of eight to ten units of platelets.18 WB provides the most physiologic fluid replacement, and assuages concerns regarding the volume of anticoagulant infused during resuscitation.19,20
And are there Disadvantages to Whole Blood?
SWB and FWB performance and safety do not differ significantly when compared to component therapy, but they are associated with unique disadvantages.21 FWB may confer increased risk of transfusion-transmitted disease (TTD) such as HIV, hepatitis B/C, and syphilis. FWB also carries an increased risk of clerical errors causing major mismatch when ABO-identical WB is given due to its immediate collection and storage.20,22 In contrast, SWB collected in licensed blood centers must be tested to the same extent as component therapy and therefore offers the same level of TTD safety. As previously discussed, SWB may be the blood product of choice in civilian practice. The main disadvantage of SWB is that it may be more likely to cause plasma-associated transfusion reactions like transfusion-related lung injury (TRALI) due to the presence of antibodies to human leukocyte antigen HLA or leukocytes in the donor’s plasma.23 Recently approved leukoreduction filters provide a possible solution for this issue and can be used for FWB. Another disadvantage of using SWB is that although current studies are underway, there is not enough existing evidence from randomized controlled trials.24
Administration and Practical Solutions
Before the civilian sector begins regular use of WB, particular concerns must be addressed.
- Platelet (PLT) efficacy following cold storage
- Risk of hemolytic transfusion reactions
- Logistical challenges specific to WB
- Hypocalcemia exacerbated by transfusion of blood products
Current practice under American Association of Blood Banks (AABB) standards is to store PLTs at 22-24º C, or room temperature (RT). Storage for longer periods of time may increase risk of bacterial contamination. In addition, efficacy of PLTs stored at RT decreases over time due to the process called “platelet storage lesion”. As a result, the FDA does not allow PLTs to be stored for more than five days and they must be tested for bacteria.25,26 However, recent data suggest that PLTs may be able to maintain function for up to twenty-one days when placed in cold storage, and that these PLTs may have superior acute hemostatic function compared to PLTs stored at RT.27-30 While it has not yet been demonstrated in human trials, it can be postulated that SWB is a simpler alternative to current practice of PLT transfusion.31
A major concern with SWB is the risk of hemolytic reactions caused by preformed immunoglobulin M (IgM) type anti-A and anti-B if group O WB is given to non-group O patients. Each unit of SWB can include 300mL of plasma which is enough to cause clinically relevant direct intravascular hemolysis of the donor RBCs if the levels of antibody present are high enough. Currently, transfusion is considered to be at minimal risk of ABO-incompatible hemolysis if anti-A and anti-B titers show IgM <100 and IG <400.32,33 Civilian risk of hemolytic reactions secondary to plasma incompatible transfusions using titered donors is about 1:120,000, which is less than currently occur with 1:1:1 massive transfusion protocols.34 Therefore, early resuscitation with low-titer group O whole blood (LTOWB) can be considered safe to administer within the correct context.
Several groups have now created guidelines to ensure LTOWB is properly collected and administered. The Ranger O Low Titer (ROLO) program sought to mitigate risks by testing donors in the pre-deployment setting for low IgM anti-A and anti-B titers (<128). Donors with low titers were labeled as ‘universal donors’ and were able to provide blood for collection and ‘buddy transfusions’ during the care of a patient with traumatic hemorrhagic shock.8 Civilian guidelines created by the University of Pittsburgh Medical Center state donors must be male, O positive, and have anti-A and anti-B titers <50 using an immediate spin saline tube method.35 Following these advances, LTOWB administration was recently approved by the AABB following the recommendation from The Trauma Hemostasis and Oxygen Research (THOR)-ABBB joint working group.36,37 The standard’s 31st edition states that the definition of “low titer” is decided locally by individual transfusion services, and the transfusion service must have a policy specifying which patients may receive whole blood, the maximum amount of whole blood per patient, and provide instructions on monitoring for adverse events following transfusion.15 It adds that the previous AABB mandate, which required issued WB to be ABO-identical to the recipient, needs to be adapted in order to accommodate giving group O WB to recipients during trauma resuscitation since the need for rapid administration typically does not allow time for traditional type and crossmatch.38 An alternative solution is that WB units could be recognized as equivalent to RBC units, allowing the release of group O WB for trauma resuscitation in patients without a known ABO group.
When considering isoimmunization and Rh type, hemolytic disease of the fetus and newborn in women of childbearing age is of concern.39 This is potentially mitigated by the administration of anti-D immune globulin (RhIg) and a well-described immunosuppression in trauma patients.40 Women of childbearing age who are given Rh positive pRBCs or LTOWB should be considered for RhIg as well as obstetric and pathology consultation within 24 hours.41
What are some challenges?
There are major logistical challenges in the institution of a WB program in civilian practice. Hospitals must first develop a collection program and standardize an operating procedure for titer testing. Any new intervention is likely to be impeded by unexpected obstacles. For example, a pilot study at Memorial Hermann in Texas experienced added delay in treatment while awaiting WB randomization, unintentionally resulting in trauma faculty often excluding more unstable patients who may have gained the most benefit from WB from the study.42 Navarrete, et al. discussed this result in a letter to the editor, and voiced support for the initial transfusion of plasma to prevent challenges created by supplying WB to emergency departments.42,43 Despite the logistical simplification of administering plasma in place of WB, there was no significant benefit, and WB still holds the most potential to re-modernize trauma resuscitation.44
While the advantages of WB over component therapy have only been shown to be significant in pre-hospital practice and austere environments, this could be because of the small number of trials involving WB in the civilian sector.9,45-47 To date, the only randomized controlled trial (RCT) addressing WB in the civilian population is a single-center randomized study done in 2013.42 The lack of robust data should only further encourage research into LTOWB, particularly in the pre-hospital setting with its recent use in advanced emergency medical services (EMS).
Emergency Services District 48 and Cypress Creek in Texas were first to carry WB and have infused more than 100 units with their protocol.48 The South Texas Blood and Tissue Center (STBTC), UT Health Office of the Medical Director San Antonio, San Antonio Military Medical Center, US Army Institute for Surgical Research, and Southwest Texas Regional Advisory Council for Trauma (STRAC) collaborated to initiate LTOWB administration in all phases of their trauma system to serve a population of over 1.5 million in the greater San Antonio metro area.41 As part of this process, the San Antonio Fire Department (SAFD) EMS became equipped with LTOWB in 2018.
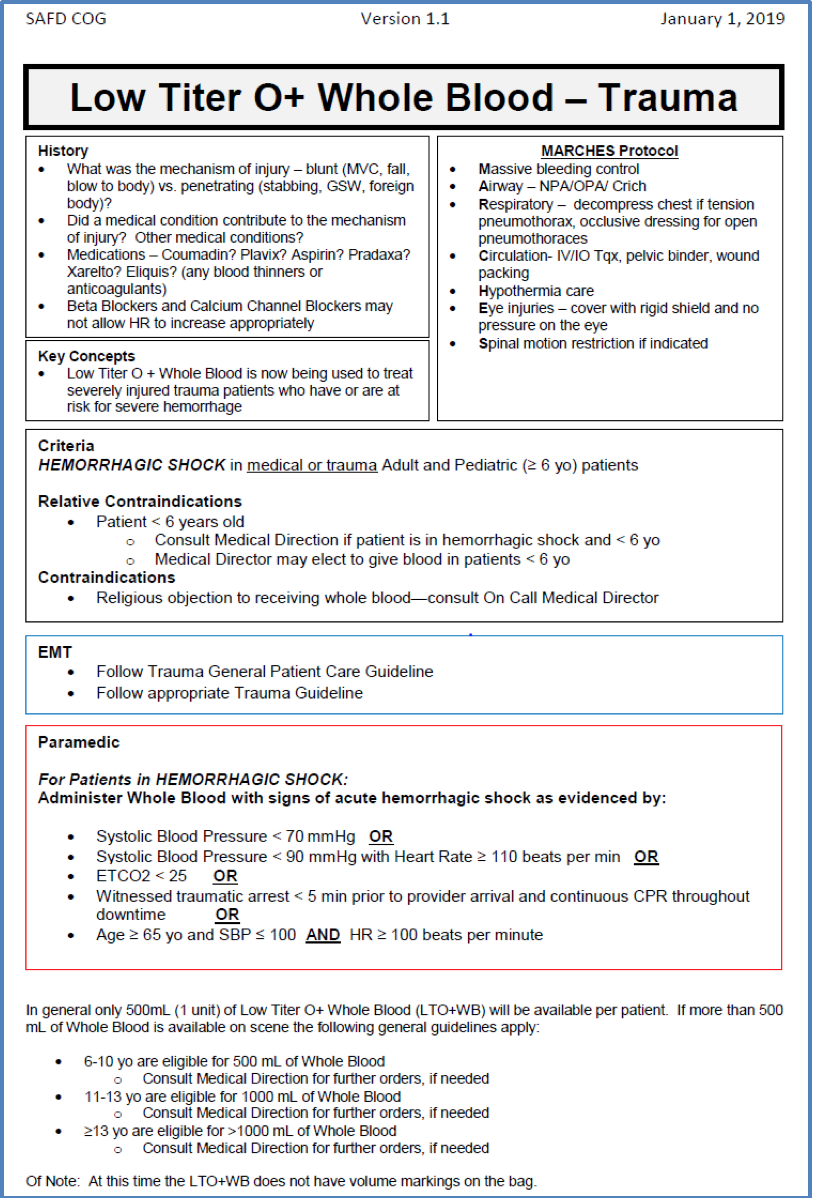
Figure 2. Low-titer group O whole blood (LTOWB) prehospital treatment parameters in San Antonio, Texas.
The current guidelines created by the previously mentioned programs are focused on critical illness transfusion triggers (Figure 2) which include heart rate, blood pressure, and end-tidal carbon dioxide (ET CO2) parameters. These were developed based off of trials demonstrating the need for massive transfusion was associated with initial pre-hospital shock index (SI) values of 1.0 and 1.2.49,50 Data also show that low ET CO2 correlates with standard indicators for shock and is predictive of the need for operative intervention.51,52 Although there is some research describing blood products improving the chance of achieving return of spontaneous circulation in cardiac arrest, further studies are needed.53,54
One facet of the logistical challenge of WB transfusion is the scalability in the pre-hospital setting given WB’s limited shelf life. Regarding this issue, the San Antonio EMS system has fostered an important relationship with the Southwest Texas Blood Tissue Center (STBTC), which also performs infectious screening. SWB is collected at STBTC, stored in a pre-cooled patented temperature-controlled container, and then assigned to a transport vehicle. The cooled WB is then rotated through the helicopter EMS for two weeks where it is kept in a refrigerator, to ground EMS for two weeks at 1-9 degrees Celsius, and returned to a hospital for a week. This cycle ensures viability and availability of WB. This protocol improves efficiency of WB use in densely populated areas, but the short shelf life may be cost ineffective for small or rural hospitals that do not experience trauma as regularly, creating more blood waste. Future solutions include the possibility of transporting WB to mass casualty events where it may be most needed via EMS command vehicles, helicopter, or to local hospitals directly.
While component therapy has been preferred over WB for trauma in civilian medicine, it is these authors’ opinion that reconsidering the use of LTOWB is the next important arena of research in modern trauma resuscitation.55
What about pediatric patients?
There is not robust literature concerning massive transfusion in pediatrics, and more specifically WB transfusion. Transfusion guidelines in pediatrics mainly reflect expert opinion or extrapolated results from studies done in adults.50 The type of injury further complicates this issue since pediatric trauma is usually blunt, not penetrating.56 It is logical that the 1:1:1 component transfusion is sensible in this population but carries the risk of over-resuscitation due to weight-based dosages. WB may be preferable as it offers all components in one container, which is administered as a single weight-based dose or titrated based on continued blood loss.
Future Directions
Another consideration when utilizing massive transfusion protocols is the effect of blood products on electrolyte levels, specifically calcium. Hypocalcemia is a common metabolic derangement in already critically ill, acidotic and coagulopathic trauma patients. Ionized calcium concentration is important for both cardiovascular function and coagulation and is postulated to be a predictor of mortality in severely injured patients.57 This depletion of ionized calcium is exacerbated by the administration of blood products due the infusion of citrate, a chelating agent and anticoagulant added to blood bags for storage.
In a retrospective review of trauma patients who received blood products during transport by the UK Medical Emergency Response Team in Afghanistan, the incidence of hypocalcemia was 70%, which allows for correlation of expected ionized calcium levels per unit dose of WB transfusion. In this study, 10 milliliter (mL) of IV calcium chloride given with each unit of blood significantly decreased the risk of hypocalcemia on arrival to the military treatment facility.58 Another civilian study reported an incidence of hypocalcemia during massive transfusion to be 97% with the majority being classified as severe hypocalcemia (ionized calcium <0.90 mmol/L) which was further associated with significantly higher mortality.59 The Committee for Tactical Emergency Casualty Care (C-TECC) was formed to accelerate advancements from military medicine into the civilian sector, and worked with George Washington University to propose protocol for repletion of calcium during blood product transfusion. Similar to the treatment used in the UK Medical Emergency Response Team, one suggestion is to dilute 1 gram of calcium chloride into a 100 mL bag of normal saline to be infused at the same time each unit of LTOWB is given. Alternatively, calcium via minijet in 10 mL aliquots may be more feasible in the prehospital setting. Calcium repletion during transfusion requires further research to demonstrate a mortality benefit, but it is the author’s opinion that the practice is feasible and seems intuitive.
In general, the current literature needs more robust prospective patient outcome data regarding WB transfusion, though studies performed on retrospective data found WB improved 30-day survival.8 More RCT data are needed in evaluating patient outcomes like mortality and adverse effects, as well as viscoelastic hemostatic assay testing of WB. There is also a need for cost-analysis studies.
Takeaways
- The safety and efficacy of whole blood has been proven in the military setting.
- SWB simplifies transfusion protocols and provides the most physiologic solution, making it the blood product of choice for pre-hospital trauma resuscitation.
- SWB is likely also preferred for initial hospital resuscitation, but more literature is needed.
- Several systems have integrated SWB into the emergency medical system with success using a predefined pre-hospital algorithm despite logistic challenges.
- Calcium administration in the pre-hospital setting should be considered.
The authors would like to acknowledge the following for their contributions to this article as well as the emerging field at large: Dr. Julian Mapp, Dr. David Wampler and Dr. David Miramontes, of University of Texas Health San Antonio Department of Emergency Health Sciences, Office of the Medical Director, San Antonio, Texas; Dr. Donald Jenkins, Professor of Surgery, Division of Trauma and Emergency Surgery at UT Health San Antonio, and Chief Michael Stringfellow of San Antonio Fire Department, Texas.
References/Further Reading
- Wyrzykowski AD, Feliciano DV. Trauma damage control. Trauma. 2008;6:851-870.
- Sauaia A, Moore FA, Moore EE, Haenel JB, Read RA, Lezotte DC. Early predictors of postinjury multiple organ failure. Archives of surgery. 1994;129(1):39-45.
- Spurgeon N. Medical Support of the U.S. Army in Vietnam, 1965–1970 Department of the Army. 1973.:45–80.
- Penn-Barwell J, Bishop J, Roberts S, Midwinter M. Injuries and outcomes: UK military casualties from Iraq and Afghanistan 2003–2012. Paper presented at: Orthopaedic Proceedings 2013.
- Brohi K, Cohen MJ, Ganter MT, Matthay MA, Mackersie RC, Pittet J-F. Acute traumatic coagulopathy: initiated by hypoperfusion: modulated through the protein C pathway? Annals of surgery. 2007;245(5):812.
- Pidcoke HF, Aden JK, Mora AG, et al. Ten-year analysis of transfusion in Operation Iraqi Freedom and Operation Enduring Freedom: increased plasma and platelet use correlates with improved survival. The journal of trauma and acute care surgery. 2012;73(6 Suppl 5):S445-452.
- Beckett MA, Callum J, da Luz LT, et al. Fresh whole blood transfusion capability for Special Operations Forces. Canadian Journal of Surgery. 2015;58(3 Suppl 3):S153.
- Fisher AD, Miles EA, Cap AP, Strandenes G, Kane SF. Tactical damage control resuscitation. Military medicine. 2015;180(8):869-875.
- Spinella PC, Perkins JG, Grathwohl KW, Beekley AC, Holcomb JB. Warm fresh whole blood is independently associated with improved survival for patients with combat-related traumatic injuries. The Journal of trauma. 2009;66(4 Suppl):S69.
- Spinella PC, Pidcoke HF, Strandenes G, et al. Whole blood for hemostatic resuscitation of major bleeding. Transfusion. 2016;56:S190-S202.
- Hughes J, Macdonald V, Hess J. Warm storage of whole blood for 72 hours. Transfusion. 2007;47(11):2050-2056.
- Kurup PA, Arun P, Gayathri NS, Dhanya CR, Indu AR. Modified formulation of CPDA for storage of whole blood, and of SAGM for storage of red blood cells, to maintain the concentration of 2,3-diphosphoglycerate. Vox sanguinis. 2003;85(4):253-261.
- AABB. Circular of Information for the Use of Human Blood and Blood Components. In: AABB, ed: American Association of Blood Banks (AABB); 2017.
- Administration FDA. Code of Federal Regulations Title 21. Chapter I – Food and Drug Administration Department of Health and Human Services 2018.
- Darlington DN, Chen J, Wu X, Keesee J, Liu B, Cap AP. Whole Blood Stored at 4° C for 7 Days Is Equivalent to Fresh Whole Blood for Resuscitation of Severe Polytrauma. Am Soc Hematology; 2014.
- Ponschab M, Schochl H, Gabriel C, et al. Haemostatic profile of reconstituted blood in a proposed 1:1:1 ratio of packed red blood cells, platelet concentrate and four different plasma preparations. Anaesthesia 2015; 70: 528–36.
- Hess JR. Resuscitation of trauma-induced coagulopathy. ASH Education Program Book. 2013;2013(1):664-667.
- Lavee J, Martinowitz U, Mohr R, et al. The effect of transfusion of fresh whole blood versus platelet concentrates after cardiac operations. A scanning electron microscope study of platelet aggregation on extracellular matrix. The Journal of thoracic and cardiovascular surgery. 1989;97(2):204-212.
- Jenkins DH, Rappold JF, Badloe JF, et al. Trauma hemostasis and oxygenation research position paper on remote damage control resuscitation: definitions, current practice, and knowledge gaps. Shock (Augusta, Ga). 2014;41(0 1):3-12.
- Gunter Jr OL, Au BK, Isbell JM, Mowery NT, Young PP, Cotton BA. Optimizing outcomes in damage control resuscitation: identifying blood product ratios associated with improved survival. Journal of Trauma and Acute Care Surgery. 2008;65(3):527-534.
- Spinella PC, Perkins JG, Grathwohl KW, et al. Risks associated with fresh whole blood and red blood cell transfusions in a combat support hospital. Critical care medicine. 2007;35(11):2576-2581.
- Ho J, Sibbald WJ, Chin-Yee IH. Effects of storage on efficacy of red cell transfusion: when is it not safe? Critical care medicine. 2003;31(12):S687-S697.
- Bux J. Transfusion‐related acute lung injury (TRALI): a serious adverse event of blood transfusion. Vox sanguinis. 2005;89(1):1-10.
- Toy P, Popovsky MA, Abraham E, et al. Transfusion-related acute lung injury: definition and review. Critical care medicine. 2005;33(4):721-726.
- Seghatchian J, Krailadsiri P. Platelet storage lesion and apoptosis: are they related? Transfusion and Apheresis Science. 2001;24(1):103-105.
- Kuehnert MJ, Roth VR, Haley NR, et al. Transfusion‐transmitted bacterial infection in the United States, 1998 through 2000. Transfusion. 2001;41(12):1493-1499.
- Getz TM, Montgomery RK, Bynum JA, Aden JK, Pidcoke HF, Cap AP. Storage of platelets at 4 C in platelet additive solutions prevents aggregate formation and preserves platelet functional responses. Transfusion. 2016;56(6):1320-1328.
- Cap AP, Spinella PC. Just chill—it’s worth it! Transfusion. 2017;57(12):2817-2820.
- Pidcoke HF, Spinella PC, Ramasubramanian AK, et al. Refrigerated platelets for the treatment of acute bleeding: a review of the literature and reexamination of current standards. Shock. 2014;41:51-53.
- Cap AP. Platelet storage: a license to chill! Transfusion. 2016;56(1):13-16.
- Kaur P, Basu S, Kaur G, Kaur R. Transfusion protocol in trauma. Journal of emergencies, trauma, and shock. 2011;4(1):103-108.
- Berséus O, Boman K, Nessen SC, Westerberg LA. Risks of hemolysis due to anti‐A and anti‐B caused by the transfusion of blood or blood components containing ABO‐incompatible plasma. Transfusion. 2013;53:114S-123S.
- Cooling L. ABO and platelet transfusion therapy. IMMUNOHEMATOLOGY-WASHINGTON DC-. 2007;23(1):20.
- Strandenes G, Berséus O, Cap AP, et al. Low titer group O whole blood in emergency situations. Shock. 2014;41:70-75.
- Yazer MH, Jackson B, Sperry JL, Alarcon L, Triulzi DJ, Murdock AD. Initial safety and feasibility of cold-stored uncrossmatched whole blood transfusion in civilian trauma patients. Journal of Trauma and Acute Care Surgery. 2016;81(1):21-26.
- Emergency Release Low Titer O Whole Blood Is Now Permitted by AABB Standards [press release]. The Trauma Hemostasis and Oxygen Research (THOR) Network, January 7, 2018 2018.
- Banks AAoB. Standards for Blood Banks and Transfusion Services. American Association of Blood Banks; 2018.
- Hillyer CD, Josephson CD, Blajchman MA, Vostal JG, Epstein JS, Goodman JL. Bacterial contamination of blood components: risks, strategies, and regulation joint ASH and AABB educational session in transfusion medicine. ASH Education Program Book. 2003;2003(1):575-589.
- Porter TF, Silver RM, Jackson GM, Branch DW, Scott JR. Intravenous immune globulin in the management of severe Rh D hemolytic disease. Obstetrical & gynecological survey. 1997;52(3):193-197.
- Reed W, Lee T-H, Norris PJ, Utter GH, Busch MP. Transfusion-associated microchimerism: a new complication of blood transfusions in severely injured patients. Paper presented at: Seminars in hematology 2007.
- Mcginity AC, Zhu CS, Greebon L, et al. Prehospital low-titer cold-stored whole blood: Philosophy for ubiquitous utilization of O-positive product for emergency use in hemorrhage due to injury. Journal of Trauma and Acute Care Surgery. 2018;84(6S):S115-S119.
- Cotton BA, Podbielski J, Camp E, et al. A randomized controlled pilot trial of modified whole blood versus component therapy in severely injured patients requiring large volume transfusions. Annals of surgery. 2013;258(4):527-533.
- Navarrete SB, Rothstein B, Scott MJ. Too Early to Jump Ship on Whole Blood for Hemorrhagic Trauma? Anesthesia & Analgesia. 2018.
- Moore HB, Moore EE, Chapman MP, et al. Plasma-first resuscitation to treat haemorrhagic shock during emergency ground transportation in an urban area: a randomised trial. The Lancet. 2018;392(10144):283-291.
- Jones AR, Frazier SK. Increased mortality in adult patients with trauma transfused with blood components compared with whole blood. Journal of trauma nursing: the official journal of the Society of Trauma Nurses. 2014;21(1):22-29.
- Repine TB, Perkins JG, Kauvar DS, Blackborne L. The use of fresh whole blood in massive transfusion. J Trauma. 2006;60(6 Suppl):S59-69.
- Chandler MH, Roberts M, Sawyer M, Myers G. The US military experience with fresh whole blood during the conflicts in Iraq and Afghanistan. Seminars in cardiothoracic and vascular anesthesia. 2012;16(3):153-159.
- Dodge M, Thompson D, Bank E, Nealy W, Fisher A. Whole blood in EMS may save lives. J Emerg Med Serv. 2018;43(2):50-54.
- Olaussen A, Peterson EL, Mitra B, O’Reilly G, Jennings PA, Fitzgerald M. Massive transfusion prediction with inclusion of the pre-hospital Shock Index. Injury. 2015;46(5):822-826.
- Hamada SR, Rosa A, Gauss T, et al. Development and validation of a pre-hospital “Red Flag” alert for activation of intra-hospital haemorrhage control response in blunt trauma. Critical Care. 2018;22(1):113.
- Caputo ND, Fraser RM, Paliga A, et al. Nasal cannula end-tidal CO2 correlates with serum lactate levels and odds of operative intervention in penetrating trauma patients: a prospective cohort study. Journal of Trauma and Acute Care Surgery. 2012;73(5):1202-1207.
- Stone Jr ME, Kalata S, Liveris A, et al. End-tidal CO2 on admission is associated with hemorrhagic shock and predicts the need for massive transfusion as defined by the critical administration threshold: A pilot study. Injury. 2017;48(1):51-57.
- Lockey D, Crewdson K, Davies G. Traumatic cardiac arrest: who are the survivors? Annals of Emergency Medicine. 2006;48(3):240-244.
- Moriwaki Y, Sugiyama M, Tahara Y, et al. Blood transfusion therapy for traumatic cardiopulmonary arrest. Journal of emergencies, trauma, and shock. 2013;6(1):37.
- Moor P, Rew D, Midwinter M, Doughty H. Transfusion for trauma: civilian lessons from the battlefield? Anaesthesia. 2009;64(5):469-472.
- Istaphanous GK, Wheeler DS, Lisco SJ, Shander A. Red blood cell transfusion in critically ill children: a narrative review. Pediatric Critical Care Medicine. 2011;12(2):174-183.1. Wyrzykowski AD, Feliciano DV. Trauma damage control. Trauma. 2008;6:851-870.
- MacKay EJ,Stubna MD,Holena DN, et al. Abnormal Calcium Levels During Trauma Resuscitation Are Associated With Increased Mortality, Increased Blood Product Use, and Greater Hospital Resource Consumption: A Pilot Investigation. Anesthesia and Analgesia. 2017;125(3):895-901.
- Kyle T, Greaves I, Beynon A et al. Ionised calcium levels in major trauma patients who received blood en route to a military medical treatment facility. Emergency Medicine Journal. 2018;35(3):176-179.
- Giancarelli A, Birrer KL, Alban RF, et al. Hypocalcemia in trauma patients receiving massive transfusion. The Journal of Surgical Research. 2016;202(1):182-187.









1 thought on “Whole Blood in Trauma: Ready for Primetime?”
Pingback: Helblod – Översikt – Mind palace of an ER doc