Authors: Jenna Bryant, MD (Emergency Medicine Resident Physician, Parkland Hospital, UT Southwestern) and Joby Thoppil, MD, PhD (Assistant Professor, Department of Emergency Medicine at UT Southwestern, Attending Physician at Parkland Hospital) // Edited By: Tim Montrief, MD (@EMinMiami, Chief Resident, University of Miami/Jackson Memorial Hospital); Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
The evaluation and treatment of acute injuries accounts for approximately 42.2 million visits to US Emergency Departments each year (1). Lacerations and other acute wounds are an important subset of acute injuries with approximately 9 million seen yearly in US Emergency Departments alone (20). These wounds require appropriate physical evaluation for extent of injury, radiographic evaluation for secondary injury, and irrigation/exploration for cleansing and foreign body and debris removal. Special considerations such as location and extent of injury as well as infection risk should be given to determine the optimal closure type and timing. Patients are at risk for infection, severe scarring, decreased mobility/diminished function, or prolonged pain if the emergency physician does not provide the proper initial treatment. We will delve into the basics of laceration management including evaluation, wound cleaning, closure methods, closure timing, special considerations based on location, and the diagnoses that cannot be missed.
Let’s review some cases, keeping in mind some diagnoses you’d rather not miss on first presentation.
Clinical Case 1: A healthy 32-year-old male presents to your ER for a right arm laceration and pain. A man attacked him with a piece of a broken glass bottle in an attempted robbery. The patient reports only a painful stab wound to the right forearm. You inspect the arm and see a 2.5cm curved laceration on the volar mid-forearm- there is no obvious contamination, no visible foreign bodies, and no active bleeding. The patient denies any sensory deficits at the site and distally. The patient is unable to tolerate both active and passive range of motion due to severe pain.
What emergent diagnoses should you consider in this patient?
Clinical Case 2: A morbidly obese, otherwise healthy 40-year-old female presents to your ED via ambulance with concerns for an open fracture. Patient fell onto her right leg with her proximal shin striking the edge of a metal step. She has a large 13 cm gaping laceration with exposed fat and muscle and without obvious bony or tendon injury. X-ray of her lower extremity proved there was no bony involvement of either the tibia or fibula but demonstrated extensive soft tissue injury. Upon further visual inspection, the laceration is rather close to the knee joint, and gapes open when she bends her knee. The patient has normal sensation, normal capillary refill, and full range of motion distally with minimally decreased range of motion at the knee secondary to discomfort from the wound.
What additional diagnostic testing should be considered in a wound close to a joint?
Clinical Case 3: A 62-year-old male with a history of hypertension and medication-controlled diabetes presents with a six-centimeter linear laceration to the left medial upper arm, with minimal extension into the axilla. The patient injured himself while fixing a fence post on his farm two days prior to his arrival in the ED. He slipped and fell, sustained the wound and landed in a pile of mud and excrement. He has some mild pain, but the main reason he came today was because of increased drainage from his wound.
What are some factors that make this wound high risk for infection?
Clinical Case 4: An 18-year-old female presents with foot pain after stepping on broken glass. She was able to get a large piece out, but still has a sensation that “something is still stuck.” She has some mild bleeding which is controlled with a pressure dressing and only complains of mild pain. She has full range of motion, normal capillary refill, and normal sensation. She has a 1.5 cm laceration to the plantar foot, involving the first webspace. There are no obvious foreign bodies, but she feels a sharp sensation when pressure is applied to the area.
What are some indicators that a foreign body is present?
Brief Pathophysiology of Healing
Closure of the wound is performed to obtain a functional imitation of the body’s innate skin barrier for hemostasis and infection prevention. The pathway to healing occurs in sequential fashion; briefly summarized by a hemostatic phase which includes platelet aggregation and clot formation, a proliferative phase mediated by leukocytes, and the maturation and remodeling phases that gradually improve wound tensile strength and integrity (2). Infections, foreign bodies/debris, poor vascular supply, and large gaps can delay or prevent proper wound healing, so proper attention during evaluation and management by the emergency physician is paramount to decreasing the risk of infection and minimizing scar formation (2).
Wound Evaluation
The history behind a wound is an important part of the initial evaluation i.e., the mechanism of injury, location, and length of injury, as well as the degree of contamination, time since injury, tetanus vaccination status, and any neurovascular or musculoskeletal deficits (3). The history helps determine whether radiographic data- either X-ray, computed tomography, or ultrasonography- is necessary. The history can also help determine the extent of irrigation or debridement required, the utility of antibiotics and/or the need for specialist evaluation. If the mechanism of injury (e.g. high energy, stabbing, crush, slice, gunshot), location (e.g. over a bone, near a joint, involving a tendon, through cartilage), depth, or deficits in movement/sensation is concerning for nonvisualized retained foreign body, bone involvement, joint involvement, compartment syndrome, or neurovascular injury, then advanced imaging would be most useful to ensure full evaluation of the extent of injury (3). Plain radiography can identify metallic or other radiodense foreign bodies, determine if there is underlying bone cortex involvement or overt fracture, and can also diagnose an open joint if intra-articular air is seen. Ultrasound, either formal or point-of-care, can be useful in the identification of retained foreign bodies by providing information on depth, location, and orientation relative to the probe. A CT scan will allow for the most detailed evaluation- giving a 3-dimensional assessment that can visualize foreign bodies, bone injuries, joint involvement, vascular injuries, and muscle disruptions that need to be repaired. Imaging modalities, however, cannot diagnose compartment syndrome and the emergency physician should keep the possibility on their differential during initial and repeat evaluations.

Obtain tetanus vaccination history, and update as needed- for large, contaminated wounds ensure patient has had at least three prior doses and one within the last five years. If anyone has a contaminated wound and has not yet had three doses, they will require tetanus immunoglobulin in addition to an updated tetanus toxoid vaccine (2).
Another important factor in infection risk stratification is determined by a patient’s comorbid medical conditions, the level of vascular supply to the wound, (more blood supply leads to better infection control) and bacterial colonization of the skin itself (moist areas such as perineum, axilla, feet/hands are at higher risk of infection) (4). Immunocompromised patients- those on biologic agents or chemotherapy agents, chronic steroid use, and diabetic patients are automatically at higher risk for infection and poor wound healing. Patients with peripheral vascular disease also pose an infection risk, as a healthy blood supply is necessary to prevent infection (4). Injuries to moist body areas should increase the emergency physician’s concern for infection (4).
Cleansing of Wounds – The Why, How, and When
Why? Wounds that present to the ED are dirty by definition, not the same clean incisions that surgeons often manage in the operating room. Removal of gross contamination of dirt, debris, foreign bodies as well as bacterial load begins with wound irrigation.
How? Start with wiping away visible contamination with dampened cloth to be able to visualize wound edges appropriately (5). A recent randomized control trial including over 600 patients performed in an ER setting showed no statistical difference between infection rates with sterile saline wound irrigation compared to potable tap water irrigation (6). The double-blinded study controlled for important factors including volume of irrigation, pressure and technique of irrigation while a small study with an ultimate sample of 625, it is the largest study to date. Potable tap water is a safe option for wound irrigation and should be considered if cost or availability of sterile saline is an issue (6).
The pressure used to irrigate a wound has implications beyond cleaning and can lead to damage of the wound bed, wound edges, or vascular supply which can inhibit proper healing (2). A multitude of opinions exist to describe the optimal pressure for irrigation, but varied data results are available for consideration (20). There are difficulties reliably measuring the pressure of irrigation across an entire wound bed, so assumptions are made regarding the actual pressure attained. A common rule seen is to aim for pressures of approximately 5 to13 psi- which is the pressure to break the adhesion between bacteria and surfaces (2). Multiple techniques have been described to obtain this pressure including irrigation caps attached to bottles, 18- or 19-gauge angiocatheters attached to 30-50cc syringes filled with solution, or simply running under a tap of clean water (2, 3). There is no evidence-based consensus on how to achieve optimal pressure with the irrigation fluid of your choosing, so local practice habits should be taken into consideration (20).
The volume of irrigation is another debated topic, but more is generally better. The minimum recommended is about 50-100cc solution per 1cm of wound. Adjust the amount of solution used based on the amount of contamination as necessary (2, 7).
When? The earlier you can irrigate the wound, the better. Ideally irrigation is performed after anesthetizing to decrease pain and improve ability to fully explore wound (3). Do not let a delayed presentation to treatment prevent full irrigation and exploration.
Types of Closure
Primary: The most common type of closure. This involves immediate fixation of the deep and dermal layers with sutures, staples, adhesive tapes or tissue adhesive (8). This is the preferred method for the majority of acute lacerations that can be cleaned appropriately to optimize wound healing and infection prevention.
Delayed Primary: As the name implies, this involves a delay in wound closure to allow for evaluation at a later date. This is an approach consideration for contaminated, infected, old (>24 hours) or devitalized wounds (2). Involves wound packing with return visit in 3-5 days after wound occurrence and decision to close with sutures, staples, adhesive tape, or tissue adhesive if no signs of infection are present. This is a good method for older wounds or wounds at risk for infection (2). Devitalized wounds have areas of skin or tissue with compromised blood supply and are at risk of infection due to affected delivery of blood products.
Secondary Intention: Involves the least amount of action, but most amount of patient education. Healing is unaided by sutures, staples, or adhesives (2). Allowing the body to heal by wound contraction- that is, healing from the inside/deepest layers out to the epidermal layer. This is a good method for infected or highly contaminated wounds (2). Instead of closing the skin around debris or bacteria, healing from the inside out allows contaminates to escape as the wound heals. This type of closure will result in scar formation as wound edges are not approximated, keep this in mind during your discussion with the patient.
Anesthesia
Local anesthetics typically work by disrupting sensory nerve conduction (8). Typically, ester or amide anesthetics are used i.e, procaine (ester) or lidocaine/bupivacaine (amide). Warming anesthetics to body temperature can reduce the pain on injection (8). Other options for local anesthesia can include topical lidocaine-epinephrine-tetracaine (LET), diphenhydramine or ketamine (8). LET is frequently used in children but has application in adults as well (3). LET, however, is not readily available and requires local compounding. Diphenhydramine is an option for local anesthesia, however, is the least effective in terms of analgesia (8). Finally, local infiltration of ketamine has been shown to have as effective analgesia as bupivacaine (8).
Methods
Suture, staples, adhesive tape, tissue adhesive (8).
Sutures:
Pros: Provides the most amount of tensile strength – necessary for gaping wounds and wounds near moving joints
Cons: Non-absorbable, requires follow up for removal and time/precision/expertise at placement
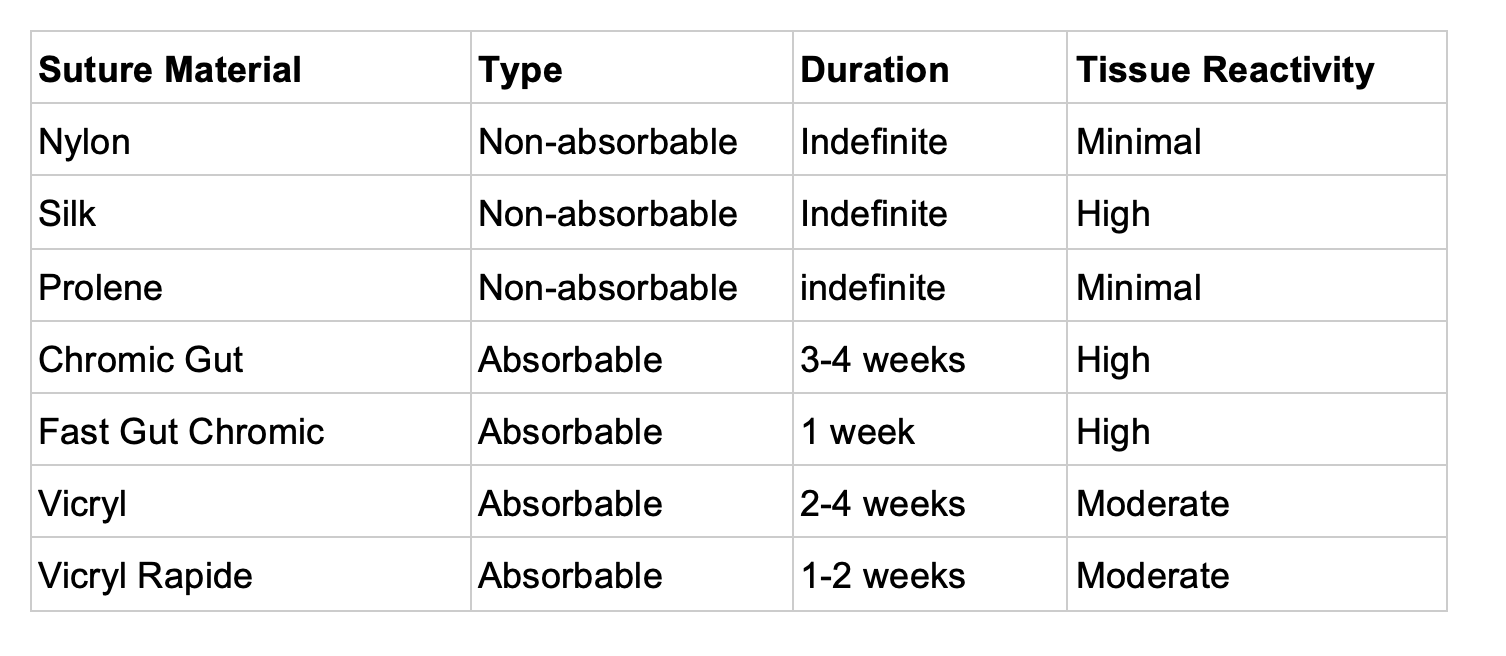
Types of suture: (9, 16).
Staples:
Pros: Fair wound approximation, quick
Cons: Cosmesis/scarring is worse; requires follow up for removal
Adhesive tape:
Pros: Quick, painless, good for skin tears; dissolves/falls off in 5-10 days with no follow up needed
Cons: Low strength, must remain dry, cannot be used on high tension wounds
Tissue adhesive (cyanoacrylate):
Pros: Quick, dissolves/falls off in 5-10 days with no follow up needed
Cons: Better for straight wounds, cannot be used for high tension wounds
Location Considerations
Scalp
Explore the wound for underlying skull fracture, and consider head CT scan before or after evaluation based on clinical picture and circumstances surrounding the injury. Large lacerations, blunt trauma, loss of consciousness, current altered mental status are some examples to consider head CT scan during your full evaluation (10). The easiest closure method are staples as this provides a rapid closure with good strength in an area with low cosmetic concern (10). Simple interrupted with nonabsorbable sutures can also be a consideration if time permits, or cosmesis is concerning (e.g. hairless areas). When exploring wounds, ensure the galea aponeurosis is intact and if not, repair the galea prior to superficial repair (11). The galea is the attachment of facial musculature, and therefore has an important role in maintaining facial structure and symmetry especially during facial expression. The closure is also needed to prevent the possible spread of infection through the potential space close to the skull (13). Galea closure is best performed with absorbable sutures- either 3.0 or 4.0- with simple interrupted as needed. Remove external staples or sutures in 10-14 days (10).
Forehead
Deep wounds require muscle repair to preserve function- this is best achieved with simple interrupted stitches with absorbable sutures (3.0 or 4.0); skin closure can be done with simple interrupted small sutures (6-0, 5-0). Remove superficial sutures in 5-7 days (10).
Face
Eyelids: Examine eyelids carefully for involvement of canthi, lacrimal system, tarsal plate, or lid margin and evidence of penetrating injury- if complex, has lacrimal involvement, or ptosis is present consider ophthalmology consultation/referral for fixation (10). To prevent downstream cosmetic and functional complications, included blocked lacrimal ducts and delayed infections. Simple lacerations should be repaired with 6-0 or 7-0 nonabsorbable suture. Avoid adhesive in this area to prevent accidental eyelid closure or eyelash involvement. Remove sutures in 3-5 days.
Ears: Cartilage structures are at high risk for hematoma formation, which can lead to strangulation of the tissue and disfiguration. Close wounds with 6-0 nonabsorbable sutures, ensure coverage of all cartilage with skin but avoid placement of sutures directly into cartilage by avoiding the smooth/gray cartilage. Apply pressure dressing to prevent hematoma formation- place gauze behind ear and wrap gauze circumferentially around head. See this article on EMDocs for examples of compressive dressing. Establish a wound recheck in 24 hours to assess for hematoma formation. Remove sutures in 5-7 days.
Lip: Intraoral lesions do not need to be sutured unless they are larger than 1cm or gaping (i.e. large enough for food to get stuck). For lesions that penetrate through outside to inside, close mucosal layer first with absorbable suture, followed by muscular layer, then finally skin. Involvement of the Vermillion border should be the first approximated suture on the skin layer- this is an appropriate skill for emergency physicians, but is best to consider your local practice patterns. Use 6-0 suture to improve cosmesis. Remove skin sutures in 5-7 days (10,11).
Arm, Hand
It is important to assess the injury at rest as well as properly evaluate motor nerve/sensory nerve function, tendon function, and perfusion of the extremity distal to the wound during motion (12,13).
Fist Fight Injuries: Do not suture. Provide prophylactic antibiotics if there are not yet signs of infection- cover for polymicrobial infection sources including S. Aureus, Streptococcus spp., Corynebacterium spp., Eikenella corrodens with amoxicillin clavulanate (PO) or ampicillin/sulbactam (IV) or combination of clindamycin & ciprofloxacin for penicillin allergies. Patient requires follow up for wound check in 1-2 days; if signs of infection are present (or develop) patient will require IV antibiotics (12,13).
Flexor Tendon/Volar Injuries: Require urgent hand specialist for definitive repair- either consultation in ER or follow up within 24 hours depending on your local practice patterns. Tendon injuries are often missed, particular partial tendon injuries and lead to decreased hand function if not appropriately identified (14, 15). Clean wound and suture the skin- if tendon is not repaired immediately by a specialist, splint wrist and MCPs with flexion and PIPs/DIPs in extension and ensure timely follow up with hand surgeon (14).
Extensor Tendon/Dorsal Injuries: Can be repaired in ED, but will require follow up with hand specialist. Tendons should be repaired with 4-0 or 5-0 nonabsorbable suture in a figure-of-eight stitch to bring the cut edges together or closely approximated simple interrupted sutures. Splint hand in functional position with wrist in slight extension/ulnar deviation and MCP/DIP/PIPs in slight flexion for follow up with hand surgeon.
Fingertips, Nails
Amputation: Pulp/skin loss with no exposed bone requires dressing changes only. Bone, joint, or tendon involvement requires hand specialist referral, with institutional dependent practices for closure or re-implantation- reimplantation needs immediate referral and proper protection of amputated digit. Wrap the amputated digit in moist gauze and place in a plastic bag, then place the bag in ice- do not place digit directly on ice. If only the distal tip (DIP) is amputated, this usually will not be replanted and will require revision amputation. Revision amputations can be done in the ER by using a rongeur to clip bone to below skin level and close skin flap over exposed bone (13). Prompt follow up with hand surgery should be secured.
Nail bed injuries: Trephinate subungual hematomas that occupy over half of the nail bed- use 18-gauge needle, cautery device, nail drill, or scalpel after proper anesthesia (12). Remove the nail if significant avulsion present to repair underlying nail bed laceration- retain the nail and suture back in place to keep the matrix open (12).
Leg, Foot
These wounds tend to be under higher tension and require more advanced suture techniques to provide support (horizontal/vertical mattress sutures, deep dermal sutures) if they are deep and involve muscles to allow the skin to come back together. Skin can be approximated with staples or sutures. Typically requires 10-14 days before suture/staple removal (17).
Can’t Miss Diagnoses
Open Fracture > visual inspection, Xray/CT; needs immediate antibiotics (first generation cephalosporin, add gentamicin if heavily contaminated), washout with orthopedics/trauma (15).
Open Joint > confirm with Xray/CT; needs immediate antibiotics (again, first generation cephalosporin, add gentamicin if heavily contaminated), washout with orthopedics/trauma (15).
Compartment Syndrome > confirm with physical exam/suspicion; needs immediate fasciotomy/OR management.
Tendon injury > confirm with physical exam, CT scan; repair (if visible), splint and follow up with specialist vs specialist consultation (18).
Arterial injury/compromised vasculature > confirm with inspection, CT; control bleeding, vascular/specialist surgical consultation in ED.
Foreign body > visual inspection, Xray/CT/Ultrasound imaging; not all require removal if search risks damage to surrounding structures; small, inert, deep or asymptomatic foreign bodies can potentially stay; remove all reactive or contaminated foreign (thorns, wood, spines) immediately if possible (19).
Nerve injury > physical examination; assess before and after repair, needs specialist follow up for prolonged recovery monitoring.
Muscle injury > physical examination, CT imaging; needs repair to recover function, splint in functional position and follow up with specialist.
Human bite > history/visual inspection; always needs antibiotics, needs wound check follow up.
Conclusion Case 1: In a patient with pain out of proportion, be sure to consider compartment syndrome, tendon injury, nerve injury, muscle injury, or underlying fracture. A CT scan ordered for this patient revealed a vascular injury with concern for muscular laceration. In the operating room, the patient had primary repair of nerve injury, tendon injury, and venous repair. No foreign body was identified.
Conclusion Case 2: A large wound in proximity to a joint is suspicious for an open joint which is an orthopedic emergency. Other considerations in this case include open fracture and extensive muscular injury. Patient was evaluated with x-ray and CT scan; no air in the joint space and no bony injury, negative for both open joint and open fracture. The large laceration was closed primarily with multiple layers after appropriate irrigation. For further information, please review this EMDocs article on open joints.
Conclusion Case 3: An older (>24h) injury in a high-risk area (here, axilla) is concerning for wound infection and risk of bacterial contamination by falling in mud. Extensive cleaning was performed, with evaluation of the depth of the wound and full function of the arm. This patient was sent home with antibiotics and local wound care instructions, returned for follow up 2 days later and had loose closure of the wound during the second look- delayed primary closure.
Conclusion Case 4: The sensation of a foreign body doubles the chance that a retained foreign body is present (4). The location of this injury could have potential tendon, nerve or vascular injury. On inspection after proper local anesthesia, a 3mm shard of glass is retrieved. The patient’s laceration was primarily closed, and she instructed to protect the laceration repair with hard soled footwear while walking.
Take Home Points:
- Evaluation of the wound begins with the history, continues with full exploration of the wound to assess the extent of repair needed, physical exam to assess structural integrity, and imaging as needed for foreign body/vascular injury (2).
- Warming anesthetics to body temperature can reduce pain with injection (8).
- LET jelly is another adjunct to avoid pain on injection (8).
- Local infiltration of ketamine may be just as efficacious as other topical anesthetics (8).
- Important considerations not to miss: open fracture, open joint, tendon injury, vascular injury, nerve injury, muscle injury, compartment syndrome (3).
- Update tetanus prophylaxis if >5 years have passed since prior immunization (2).
- Irrigation with potable tap water is just as effective as saline irrigation (6).
- Antibiotics for higher risk patients (diabetes, poor circulation, HIV/AIDS, immunocompromised), with wounds in higher risk areas (axilla, perineum, hands, feet), and high-risk wounds (human bites anywhere, mammalian bites to hand) (2).
- If transferring a digit for reimplantation, do not place digit directly on ice! Wrap amputated digit in moist gauze and place in a plastic bag which then goes on ice (14).
Further FOAM Resources:
- Snap, Crackle, POP! Open joint: ED evaluation and management
- Penetrating Wounds in the Emergency Department: Considerations for Management
- Bleeding Hand Wounds
- Betadine and Laceration Repairs
- Compartment Syndrome CCC
- Fingertip Amputations
References:
- US Department of Health, CDC. “FastStats – Emergency Department Visits.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, www.cdc.gov/nchs/fastats/emergency-department.htm.
- Nicks, et al. Acute wound management: revisiting the approach to assessment, irrigation, and closure considerations. Int J Emerg Med. 2010
- Forsch, Randall T., et al. “Laceration Repair: A Practical Approach.” AAFP, Am Fam Physician, 15 May 2017,www.aafp.org/afp/2017/0515/p628.html#.
- Reeder, Timothy J. “Chapter 9: Evaluating and Preparing Wounds.” Tintinalli’s Emergency Medicine Manual, by Michael Thomas. Fitch et al., McGraw-Hill Education, 2018, pp. 81–84.
- Fernandez, R., Griffiths, R. Water for wound cleansing. Cochrane Database Sys Rev. 2012.
- Weiss EA, Oldham G, Lin M, et al Water is a safe and effective alternative to sterile normal saline for wound irrigation prior to suturing: a prospective, double-blind, randomised, controlled clinical trial BMJ Open 2013;3:e001504. doi: 10.1136/bmjopen-2012-001504
- Heitz, Corey R. “Chapter 10: Methods for Wound Closure.” Tintinalli’s Emergency Medicine Manual, by Michael Thomas. Fitch et al., McGraw-Hill Education, 2018, pp. 85-95.
- Mankowitz, Scott L. “Laceration Management”. Selected Topics: Wound Care. The Journal of Emergence Medicine. 2017. Vol 53(3):pp 369-382
- Lee, Hyunjoo, and Layla Abubshait. “PV Card: Laceration Repair and Sutures – A Cheat Sheet Guide.” ALiEM, 2 Aug. 2017, www.aliem.com/2017/03/pv-laceration-repair-and-sutures/.
- Calvert, J. Hayes. “Chapter 11: Lacerations to the Face and Scalp.” Tintinalli’s Emergency Medicine Manual,by Michael Thomas. Fitch et al., McGraw-Hill Education, 2018, pp. 96-100.
- Fapohunda-Adekola, Toyin. “Repair of Lacerations of the Face and Scalp: Part 1.” Journal of Urgent Care Medicine, 4 Sept. 2018, www.jucm.com/repair-of-lacerations-of-the-face-and-scalp-part-1/.
- Sandier, John P. “Chapter 12: Injuries to the Arm, Hand, Fingertip, and Nail.” Tintinalli’s Emergency Medicine Manual,by Michael Thomas. Fitch et al., McGraw-Hill Education, 2018, pp. 101-107.
- Bowen, W. Talbot, and Ellen Slaven. “Evidence-Based Management of Acute Hand Injuries In the Emergency Department.” EBMedicine.net, Emergency Medicine Practice, Dec. 2014, www.ebmedicine.net/media_library/files/1214%20Hand%20Injuries(1).pdf.
- Osgood, J., et al. “Finger Amputation.” WikEM, 23 Apr. 2019, wikem.org/wiki/Finger_amputation.
- Taecker, Matthew, et al. “How to Treat Open Injuries to Flexor Compartment of Fingers and Hands.” Emergency Physicians Monthly, 3 Oct. 2014, epmonthly.com/article/open-injuries-to-flexor-compartment-of-fingers-and-hands/.
- Gunson, Dr. Todd. “Suture Materials.” DermNet NZ, 2008, www.dermnetnz.org/topics/suture-materials/.
- Davenport, Moira. “Chapter 13: Lacerations to the Leg and Foot.” Tintinalli’s Emergency Medicine Manual, by Michael Thomas. Fitch et al., McGraw-Hill Education, 2018, pp. 108-111.
- Konda, Sanjit R., et al. “Computed Tomography Scan to Detect Traumatic Arthrotomies and Identify Periarticular Wounds Not Requiring Surgical Intervention.” Journal of Orthopaedic Trauma, vol. 27, no. 9, Sept. 2013, pp. 498–504., doi:10.1097/bot.0b013e31828219bc.
- Fitch, Michael T. “Chapter 14: Soft Tissue Foreign Bodies.” Tintinalli’s Emergency Medicine Manual, by Michael Thomas. Fitch et al., McGraw-Hill Education, 2018, pp. 112-114.
- Otterness, Karalynn, and Adam J Singer. “Updates in Emergency Department Laceration Management.” Clinical and Experimental Emergency Medicine, vol. 6, no. 2, 2019, pp. 97–105., doi:10.15441/ceem.18.018.
- Torabi, Maha, et al. “ACR Appropriateness Criteria: Acute Hand and Wrist Trauma.” ACR Appropriateness Criteria, American College of Radiology, 2018, https://acsearch.acr.org/docs/69418/Narrative/.
- Bancroft, Laura, et al. “ACR Appropriateness Criteria: Acute Trauma to the Foot.” ACR Appropriateness Criteria, American College of Radiology, 2014, https://acsearch.acr.org/docs/70546/Narrative/.









1 thought on “Wounds and Lacerations in the ED: Management Pearls and Pitfalls for Emergency Physicians”
Pingback: Weekend Knowledge Dump- September 27, 2019 | Active Response Training