52 in 52 – #12: PARAMEDIC-2
- Sep 15th, 2022
- Brannon Inman
- categories:
Welcome back to the “52 in 52” series. This collection of posts features recently published must-know articles. Our twelfth post looks at the PARAMEDIC-2 trial.

Author: Christiaan van Nispen, MD (Emergency Medicine Physician Resident, San Antonio, TX) and Brannon Inman (Chief Resident, Emergency Medicine Physician, San Antonio, TX) // Reviewed by: Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
A Randomized Trial of Epinephrine in Out-of-Hospital Cardiac Arrest
AKA: The “PARAMEDIC-2” Trial
Clinical question:
In patients with out-of-hospital cardiac arrest (OHCA), does epinephrine improve 30-day survival compared to placebo?
Study design:
- Double-blind randomized, placebo-controlled trial
- 1:1 allocation ratio with treatment assignments randomly generated via computer
- Conducted with 5 NHS ambulance services in the U.K. between Dec 2014 and Oct 2017

PICO:
Population:
- Included adult patients > 16 years old with out-of-hospital cardiac arrest
- Exclusion criteria
- Traumatic arrest (in 1 EMS service)
- Pregnancy
- Arrest due to asthma
- Arrest due to anaphylaxis
- Administration of epinephrine prior to paramedic arrival
Intervention:
- 1 mg epinephrine every 3-5 minutes
Comparator:
- A placebo solution and an equal volume of isotonic crystalloid (10 mL 0.9% NS)
Outcome:
- Positive trial (statistically significant survival at 30 days higher in epinephrine arm)
- Epinephrine 3.2% survival vs. Placebo 2.4% survival
- Adjusted Odds Ratio (OR): 1.47 (95% CI 1.09 to 1.97
- Absolute risk reduction 0.89%
- NNT 112
- Fragility index of 6
- 8014 patients randomized and 2520 excluded


- Epinephrine resulted in a greater proportion of poor neurologic outcomes (modified Rankin >3 in this study, >2 in many studies examining neurologic outcomes)
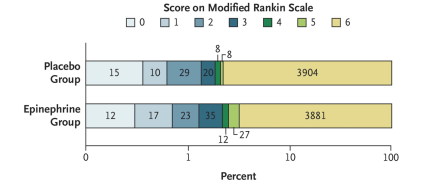
Modified Rankin Score:


Randomization:
- Treatment arms were fairly well balanced.

Take away:
- This is a pragmatic study a large number of patients. It incorporates a patient centered outcome.
- The study is technically positive. However, it shows an increased proportion of survivors with poor neurologic outcomes.
- Internal and external validity seem to be high. Groups were well balanced with bonding between participants and patients, and multiple ambulance services enrolled patients.
- Overall lower survival rate than expected.
- This study displayed high rates of bystander CPR (about 59%).
- This trial had very high rates of initial non-shockable rhythms (78.4 and 79.5%) which probably contributed to the low overall survival. Similarly, 615 patients were removed from the trial as they obtained ROSC from standard care (CPR/defibrillation) before the administration of epinephrine likely also lowering their survival rate. This also reduces external generalizability.
- Epinephrine increases survivability initially, but that gap rapidly narrows as the time approaches 30 days. This is likely due to an initial increase in neurologically devastated survivors who obtain ROSC.

My take:
In the words of Adam Thomas, we don’t make zombies. This study, while technically positive, raises technically numerous practical and moral questions. With the routine use of epinephrine, there is likely to be more ROSC. However, the number of survivors with a good neurologic outcome is statistically nonsignificant. There might be a very small number of people to survive with a good neurologic outcome that otherwise would have been lost. However, we must consider the innumerable patients we condemn to languish with neurologic devastation with the blind, thoughtless, protocol-driven administration of serial epinephrine boluses.
Reference:
- Perkins, G. D., Ji, C., Deakin, C. D., Quinn, T., Nolan, J. P., Scomparin, C., Regan, S., Long, J., Slowther, A., Pocock, H., Black, J. J. M., Moore, F., Fothergill, R. T., Rees, N., O’Shea, L., Docherty, M., Gunson, I., Han, K., Charlton, K., … Lall, R. (2018). A randomized trial of epinephrine in out-of-hospital cardiac arrest.New England Journal of Medicine, 379(8), 711–721. https://doi.org/10.1056/nejmoa1806842
- Lin, S., Callaway, C. W., Shah, P. S., Wagner, J. D., Beyene, J., Ziegler, C. P., & Morrison, L. J. (2014). Adrenaline for out-of-hospital cardiac arrest resuscitation: a systematic review and meta-analysis of randomized controlled trials. Resuscitation, 85(6), 732-740.
