Welcome back to the “52 in 52” series. This collection of posts features recently published must-know articles. Our sixteenth post looks at antiarrhythmics in shock refractory OHCA.

Author: Christiaan van Nispen, MD (Emergency Medicine Physician Resident, San Antonio, TX) and Brannon Inman (Chief Resident, Emergency Medicine Physician, San Antonio, TX) // Reviewed by: Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Effect of Time to Treatment with Antiarrhythmic Drugs on Return of Spontaneous Circulation in Shock-Refractory Out-of-Hospital Cardiac Arrest
AKA: The ROC-ALPS Trial
Question:
What is the effect of time of administration of amiodarone versus lidocaine versus placebo in achieving a return of spontaneous circulation (ROSC) by the time of hospital arrival in adults who suffered out-of-hospital cardiac arrest found by emergency medical services to be in ventricular fibrillation or pulseless ventricular tachycardia?
Design: Post-hoc analysis of data from a randomized, controlled trial
PICO
Population:
- Adults with nontraumatic out-of-hospital cardiac arrest
- Must have refractory ventricular fibrillation (VF) or pulseless ventricular tachycardia (pVT) after at least one defibrillation by EMS prior to randomization

Intervention/Control:
- There are three treatment arms in this study
- If the patient remains in VF or pVT after the first defibrillation, randomization occurs into one of the following groups:
- 300 mg amiodarone IV
- 120 mg lidocaine IV
- Placebo (0.9% NS)
- The patient was re-administered a half dose of the medication to which they were randomized if in they remain in persistent VF or pVT after subsequent defibrillation
- Initial and subsequent doses halved if weight is estimated to be < 45 kg
Outcome:
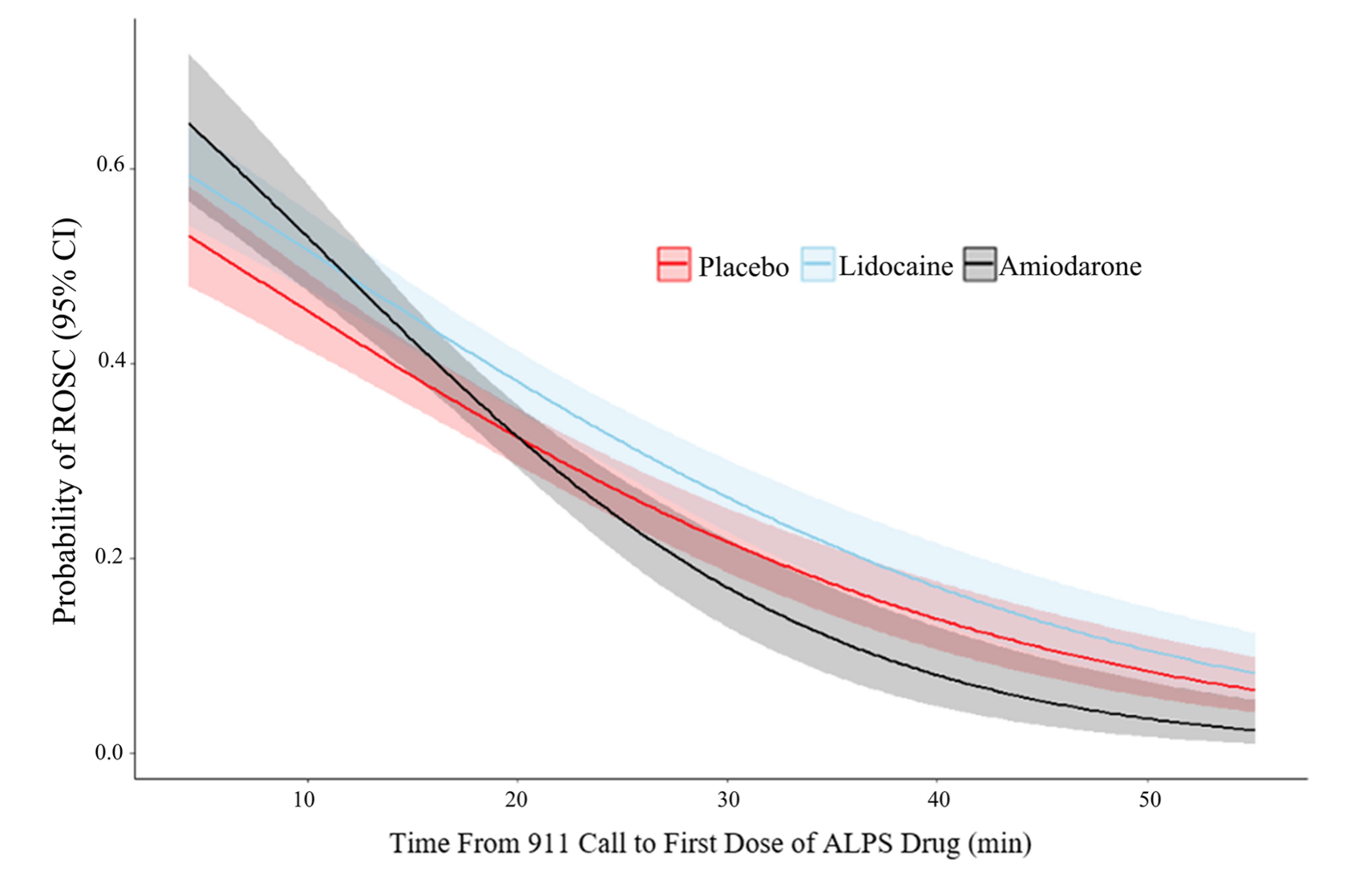
- Primary outcome was ROSC at time of ED/hospital arrival
- The overall achievement of ROSC similar across the groups
- Amiodarone appears to be the superior option if administered < 13.5 minutes post-911 call
- After 13.5 minutes, lidocaine appears superior to amiodarone
- After 19.5 minutes, even the placebo appears superior to amiodarone
Randomization: groups appear appropriately equal, though analysis is per-protocol instead of intention-to-treat.
Take Aways:
- The efficacy of amiodarone appears superior to lidocaine if administered early, but it seems to diminish by the minute to the point that lidocaine eventually becomes superior (around 20 min).
- The study states that early antiarrhythmics are better than late antiarrhythmics in VF and pVT; however, an early placebo is also better than a late placebo. Perhaps, early medication administration is just a marker for early CPR and defibrillation. As this is a post hoc analysis of another study, there exists the potential for numerous confounders. The benefit of early placebo administration is suggestive of this.
- It is unclear if there are any differences between treatment options on survival to hospital discharge, which arguably is more patient-centered than just achieving ROSC at some point.
- This study took place out-of-hospital, so any conclusions would be most applicable to the pre-hospital environment, but inferences could be made to emergency department patients who remain in shockable rhythms. The most notable of which would be that there may exist the possibility for a benefit of early antiarrhythmics.
- Looking at the time curves it appears that later administration of lidocaine is more beneficial than amiodarone. Based on these data, it may be reasonable to attempt lidocaine as the initial antiarrhythmic if a patient is presenting to you with prolonged downtime. But again, these data are hypothesis-generating.
- Largely, this study is interesting. Many questions are raised from this study. Further research is needed to investigate the benefit of antiarrhythmics along a time gradient. It does, however, seem reasonable that early administration would be beneficial. In all likelihood, there is a kindling effect involved in malignant myocardial dysrhythmias such that the longer it propagates the harder it is to break. It would be interesting further to see if there is a benefit to antiarrhythmics at the time of initial defibrillation to prevent recurrence and sustain ROSC.
My Take:
Based on the results of these data I will continue ACLS in the way I always have with a primary focus on good-quality CPR and early defibrillation. I may consciously shift to using earlier antiarrhythmics based on these data in select patients. I would consider lidocaine instead of amiodarone in patients in persistent VF or pVT in whom amiodarone has already been given (consistent with current ACLS guidelines) or who arrive at the hospital still in VF/pVT after prolonged downtime.
Reference:
Rahimi M, Dorian P, Cheskes S, et al. Effect of Time to Treatment with Antiarrhythmic Drugs on Return of Spontaneous Circulation in Shock-Refractory Out-of-Hospital Cardiac Arrest. J Am Heart Assoc. 2022;11(6):e023958. doi:10.1161/JAHA.121.023958








