Welcome back to the “52 in 52” series. This collection of posts features recently published must-know articles. Our fourth post looks at emergency resuscitative thoracotomy.

Author: Brannon Inman (Chief Resident, Emergency Medicine Physician, San Antonio, TX) // Reviewed by: Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Emergency Resuscitative Thoracotomy: A Nationwide Analysis of Outcomes and Predictors of Futility
Clinical question:
In patients undergoing emergency resuscitative thoracotomy within 60 minutes of ED presentation, what is the survival to hospital discharge, and what if any, are predictors for mortality?
Study design:
- Retrospective chart review of patients who under went emergency resuscitative thoracotomy and were reported in the American College of Surgeons Trauma Quality Improvement Program Database (ACS-TQIP) between 2010-2016
- Primary outcome was survival to hospital discharge
- Secondary outcomes (for those who survived)
- Hospital length of stay (LOS)
- Intensive care unit (ICU) LOS
- Number of complications
- Discharge destination (home versus nursing, long-term or rehabilitation facility).
- Secondary outcomes (for those who did not survive)
- Assessed the location of death: ED, operating room (OR), or ICU.
- Secondary outcomes (for those who survived)
Retrospective review methods:
- Emergency resuscitative thoracotomy was defined using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) and International Classification of Dis- eases, Tenth Revision, Clinical Modification (ICD-10-CM) procedure codes.
- For ICD-9-CM codes, the inclusion criteria were:
- Exploratory thoracotomy (34.02) with open-chest cardiac massage (37.91) or
- exploratory thoracotomy with pericardiotomy (37.12) or
- exploratory thoracotomy with open-chest cardiac massage and pericardiotomy.
- For ICD-10-CM codes, the inclusion criteria were:
- 02JA0ZZ: inspection of heart, open approach, excluding those with 0P800ZZ (procedure code indicating division of the sternum)
- Division of sternum, open approach
- Only patients whose procedures were performed within 60 min of emergency department (ED) presentation were included
PICO:
Population:
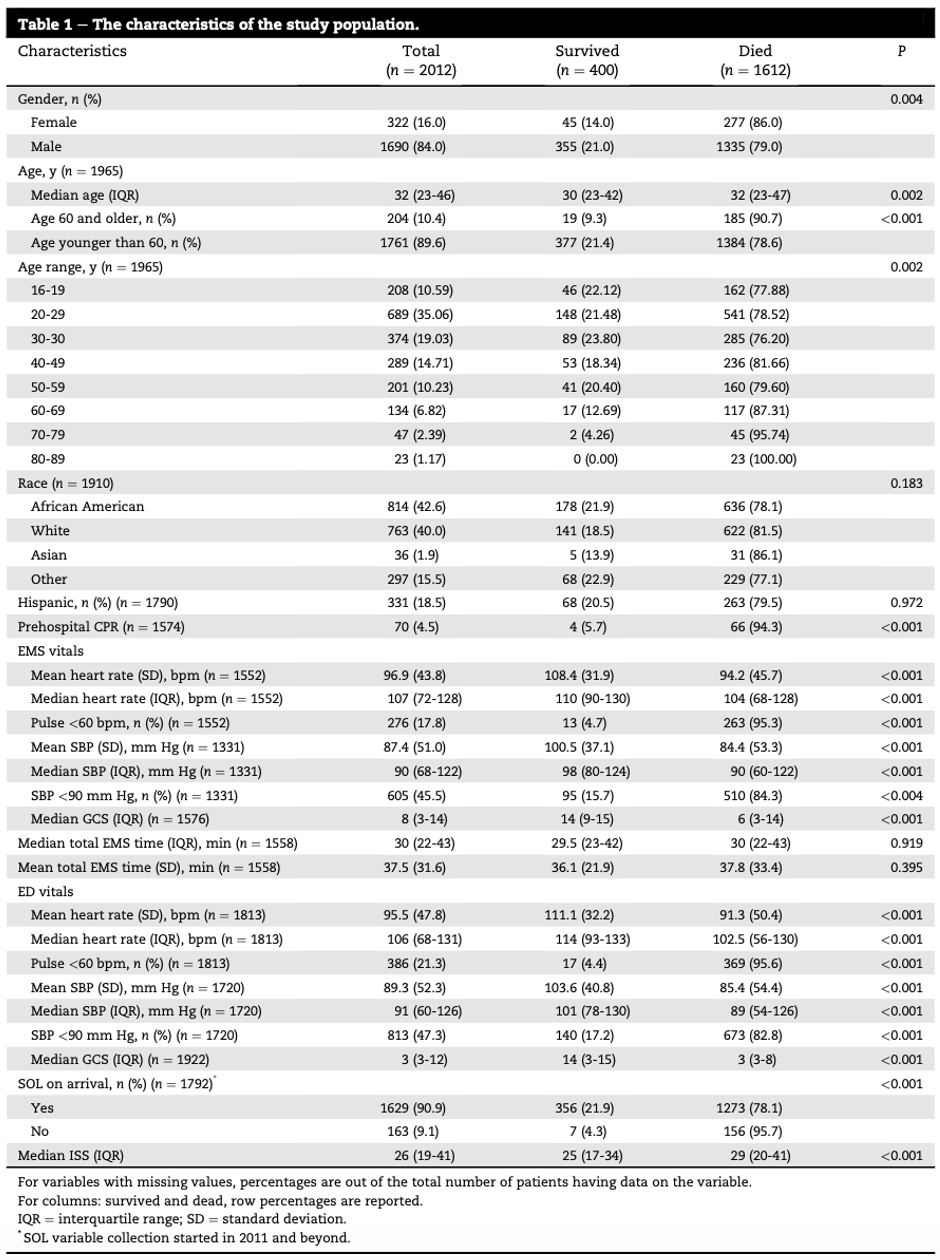
- 1,403,470 patients were screened; 2012 registry reported patients who underwent emergency resuscitative thoracotomy were selected from ACS-TQIP
- Median age was 32 years
- 84% were males
- 66.7% had penetrating trauma
- Median Injury Severity Score was 26
- 87.5% presented with signs of life
Outcome:
- Overall survival to discharge rate
- Average of cohort: 19.9%
- Penetrating: 26.0%
- 18.7% for GSW
- 45.6% for Stab Wound
- GSW was associated with a higher median hospital LOS compared with stab wound (18.5d versus 9d; P < 0.001), a higher median ICU LOS (10d versus 4d; P < 0.001), and a higher likelihood of discharge to a rehabilitation facility instead of home (33.3% versus 23.5%).
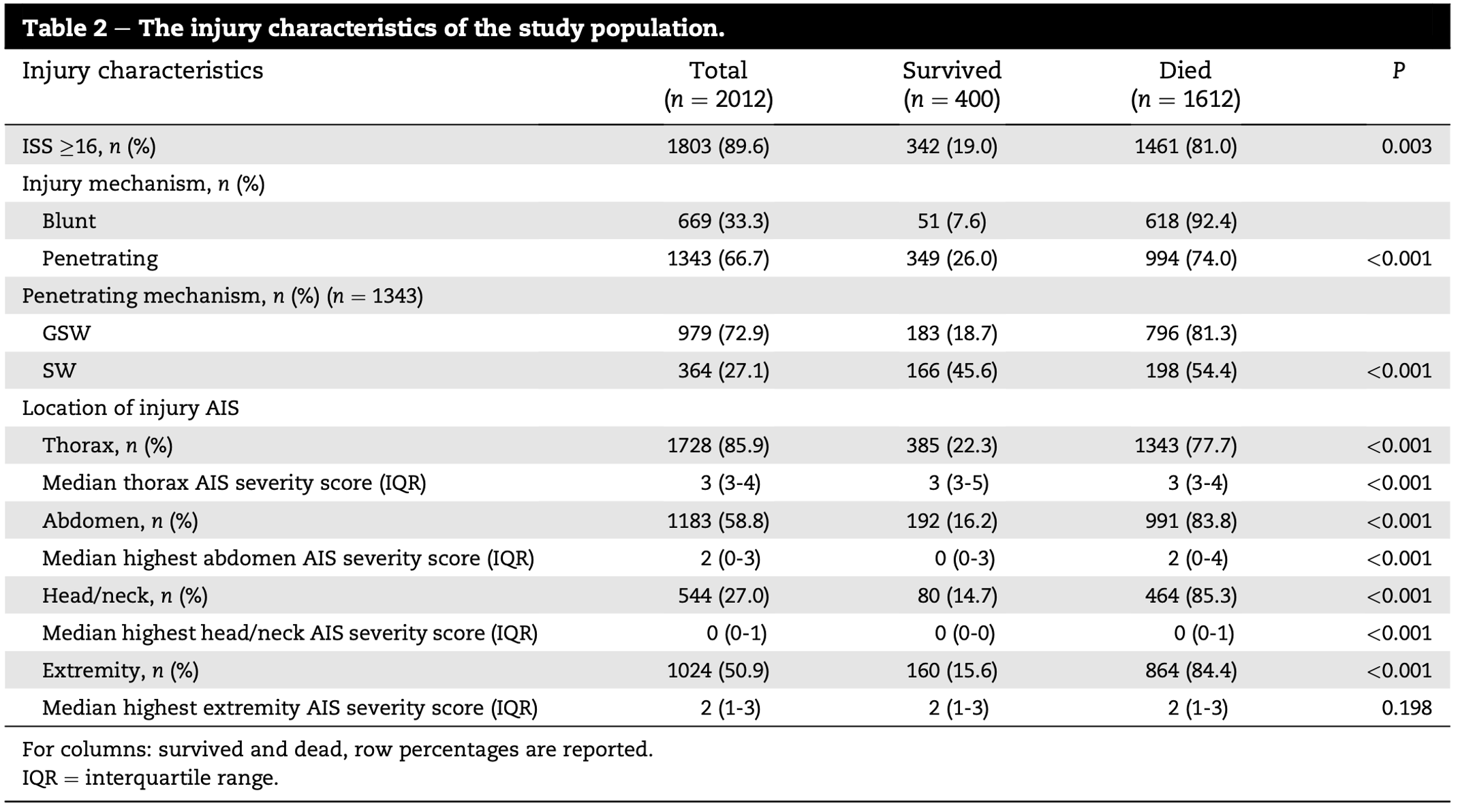
- Blunt: 7.6%
- Penetrating: 26.0%
- Of those who did not survive:
- 28% died in the ED
- 50% died in the OR
- 8% died in the ICU
- Stab Wounds more likely to die in the OR
- Average of cohort: 19.9%
- Independent predictors of mortality
- Age ≥60 years (odds ratio, 2.71; 95% confidence interval [95% CI], 1.26-5.82)
- Blunt trauma (odds ratio, 4.03; 95% CI, 2.72-5.98)
- Prehospital pulse <60 bpm (odds ratio, 3.43; 95% CI, 1.73-6.79)
- ED pulse <60 bpm (odds ratio, 4.70; 95% CI, 2.47-8.941)
- No signs of life on ED arrival (odds ratio, 3.64; 95% CI, 1.08-12.24).
- Blunt trauma was associated with
- Higher median hospital Length of stay (28 d versus 13 d; P < 0.001)
- Higher median ICU LOS (19 d versus 6 d; P < 0.001)
- Higher median number of complications (2 versus 1)
- Greater likelihood of discharge to a rehabilitation facility instead of home (72.5% versus 28.7%; P < 0.001)
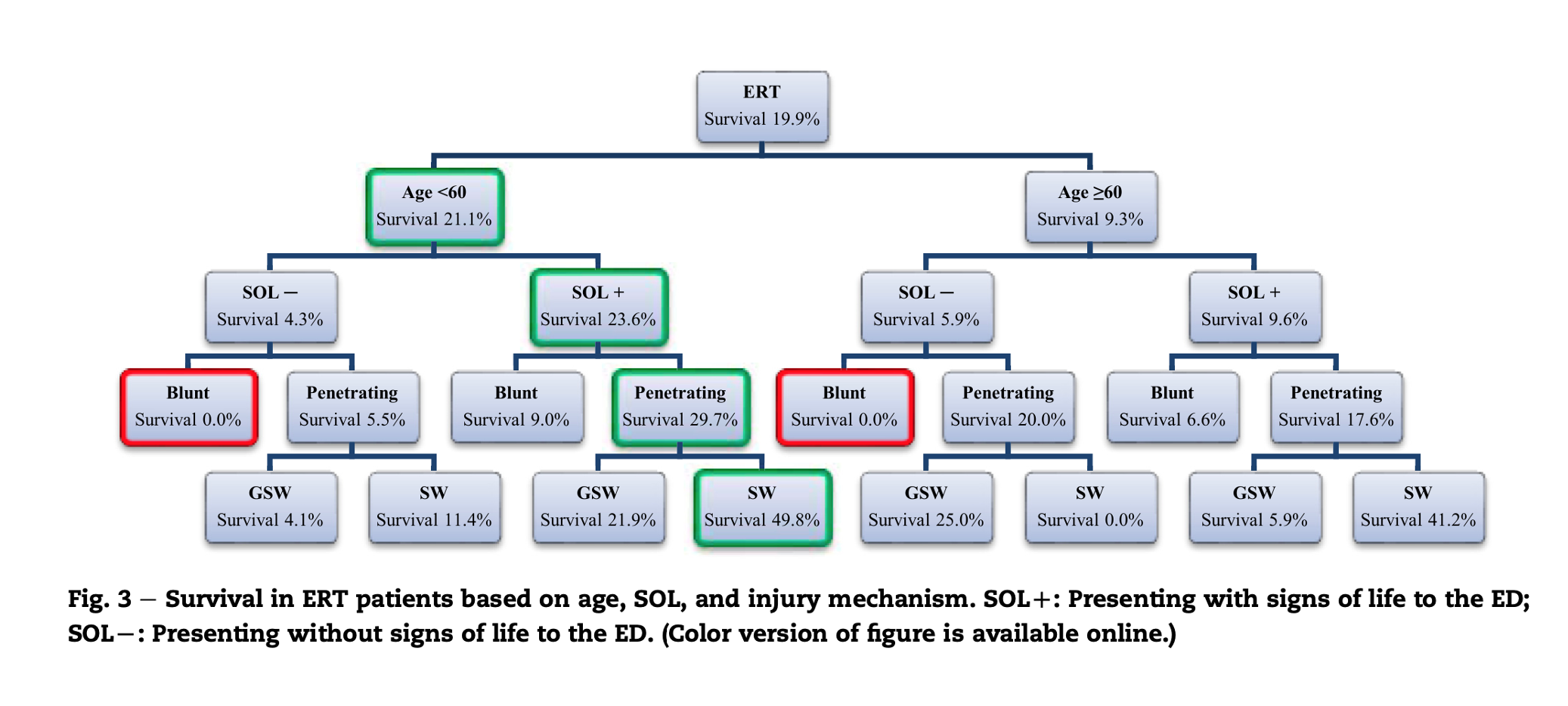
- ERT remained futile in patients with a blunt trauma presenting with no sign of life


Take away:
- Large chart review including >2000 thoracotomy patients.
- Based on the data provided in the manuscript there appears to be a preference for left lateral thoracotomy. It is unclear who underwent the (London) approach or primary clamshell extension. Prior evidence suggests a modified clamshell has a higher success rate when performed by staff emergency physicians, results in less periprocedural iatrogenic injuries, and is the preferred technique by most subjects who undergo training for this procedure.
- Overall mortality remains high (about 80%), though this is better compared to historical (approximately 10% for penetrating and less than 2% for blunt)
- The most common location of death following ED thoracotomy is the OR.
- In patients status post blunt trauma presenting with no signs of life, ERT appears to be futile.
- Penetrating trauma has the most favorable prognosis, with stab wounds doing better than gunshot wounds and having a higher rate of discharge home and shorter hospital and ICU length of stay.
- Overall this study echoes historical data in regards to those with favorable prognosis. However, the rate of survival across the board is higher in this study compared to data from 20 years ago. This might be due to selection criteria and/or improved critical care of the modern age (probably both).
My take:
The best case scenario for emergency resuscitative thoracotomy is a patient less than 60 years with a stab wound to the chest presenting to the ED with signs of life. This won’t change my approach to when I perform a thoracotomy. Blunt trauma will need to present with signs of life and witnessed loss of vital signs, and penetrating patients will need to have short periods of down time. However, I may now perform this procedure (when indicated) with a lower degree of cynicism or nihilism than previously (especially with regards to blunt traumatic arrest). I’m also a fan of the modified clamshell technique.
References:
- Panossian VS, Nederpelt CJ, El Hechi MW, et al. Emergency Resuscitative Thoracotomy: A Nationwide Analysis of Outcomes and Predictors of Futility.J Surg Res. 2020;255:486-494. doi:10.1016/j.jss.2020.05.048.
- Newberry R, Brown D, Mitchell T, Maddry JK, Arana AA, Achay J, Rahm S, Long B, Becker T, Grier G, Davies G. Prospective Randomized Trial of Standard Left Anterolateral Thoracotomy Versus Modified Bilateral Clamshell Thoracotomy Performed by Emergency Physicians. Ann Emerg Med. 2021 Mar;77(3):317-326.








