Today on the emDOCs cast with Brit Long (@long_brit), we have Part 2 on EBM updates for intubation. We’ll cover induction medications, paralytics, VL vs. DL, using the bougie, confirming ETT placement, and post intubation sedation. Please see Part 1 for background, predicting difficult BVM/intubation/cricothryotomy, physiologic factors associated with peri-intubation decompensation, preoxygenation, and apneic oxygenation.
Episode 128: Intubation EBM Updates Part 2
What induction medication should we use?
- Medications include propofol, etomidate, and ketamine. Etomidate and ketamine are more hemodynamically neutral.
- Propofol: primarily works through GABA receptors.
- Commonly used for intubation of status epilepticus, hypertensive emergencies, intracranial emergencies, or severe alcohol withdrawal syndrome (63,64).
- Dosing is 0.5-1.0 mg/kg IV over 10 seconds. Rapid onset of action (less than one minute), and a duration of 2-8 minutes (64).
- Can potentially lead to significant hypotension
- Etomidate: non-barbiturate hypnotic IV anesthetic with no analgesic properties.
- Dosing is 0.2-0.3 mg/kg IV. Onset of action of 30–60 seconds, peak effect of 1 minute, and lasts 200-300 seconds.
- There have have been concerns of adrenal suppression with etomidate, but this is controversial.
- Ketamine: NMDA antagonist with sedative and analgesic properties.
- Dosing is 1-2 mg/kg IV or 4-5 mg/kg intramuscular (IM). It has an onset of action within 30-60 seconds, peak effect within 1 minute, and half-life of 2-4 hours (68).
- Multiple studies have compared ketamine and etomidate, with varying results regarding peri-intubation adverse events (69-71).
- 2024 meta-analysis including 7 RCTs and 1 propensity-matched study evaluated critically ill adult patients who underwent emergency ETI (69). Smilar mortality between ketamine and etomidate (RR 0.96; 95% credible interval 0.8-1.1). No difference in the Sequential Organ Failure Assessment (SOFA) score, vasopressor-free days, ventilator-free days, blood pressure, and first-attempt success (69). With Bayesian analysis of the trial results, 68.6% probability that ketamine would reduce mortality by up to 1% when compared to etomidate. Probability of 41.6% that ketamine would reduce mortality by ≥ 1% when compared to etomidate (69).
- 2025 meta-analysis of 14 studies found no difference in 30 day survival. Ketamine associated with a higher requirement for post-intubation vasopressor support (OR 0.71, 95% CI: 0.53-0.96) but an increase in ICU-free days. Etomidate use correlated with higher incidence of adrenal insufficiency (OR 2.43, 95% CI: 1.67-3.53, P < 0.001). No significant differences in intubation difficulty, cardiovascular collapse, or systemic steroid use between the groups.
- Guidelines:
- SCCM 2023 Clinical Practice Guidelines (published before these meta-analyses) suggest there is no difference between etomidate and other agents in terms of mortality, hypotension, or vasopressor use in the peri-intubation period or through hospital discharge (61).
- ACEP provides a level B recommendation supporting etomidate or ketamine to reduce the risk of peri intubation hypotension. Level c recommendation to avoid fentanyl, midazolam, or propofol in patients are increased risk for postintubation hypotension.
- European Society for Emergency Medicine recognize that both ketamine and etomidate have nearly neutral hemodynamic properties, but etomidate may potentially result in adrenal suppression, and that led them to recommend ketamine (62).
- Summary: Based on the literature, this is an extremely nuanced decision. Both ketamine and etomidate are great options. Propofol may be a good option for patients with status epilepticus, alcohol withdrawal syndrome, and severe hypertension.
What paralytic should we use?
- Paralytic agents are associated with a greater rate of first-pass success; should be using these in the majority of cases of intubation.
- Succinylcholine: first used in the late 1940s (75).
- Depolarizing muscle relaxant that directly binds to postsynaptic acetylcholine receptors. Dosing is 1.0-1.5 mg/kg IV. Onset of 45 seconds and duration of 4-6 minutes (76). May also be administered IM, with a time of onset of 2-3 minutes and duration 10-30 minutes (76).
- Rocuronium: introduced in the 1990s.
- Nondepolarizing agent that competitively antagonizes the acetylcholine receptor (77,78). Dosing is 0.6-1.2 mg/kg IV, and it has a time of onset 45-120 seconds (dose dependent) and duration of action 30-90 minutes (78).
- 2017 meta-analysis included 50 studies comparing succinylcholine with rocuronium found succinylcholine was superior to low dose rocuronium (0.6-0.7 mg/kg) for excellent intubating conditions (RR 0.86; 95% CI 0.81-0.92) and clinically acceptable conditions (RR 0.97; 95% CI 0.95-0.99) (79). No difference in studies utilizing higher doses of rocuronium (≥ 0.9 mg/kg IV).
- National Emergency Airway Registry (NEAR) study found no difference in succinylcholine or rocuronium in first-pass success (87.0% versus 87.5%) or adverse events (14.7% versus 14.8%) (80). Mean dose was succinylcholine 1.8 mg/kg IV and rocuronium 1.2 mg/kg IV.
- Both succinylcholine and high-dose rocuronium achieve similar intubating conditions, they have a similar onset of action, and ultimately both are effective paralytics.
- Must several different factors when choosing the paralytic.
- Succinylcholine has a duration of 4-6 minutes, so can perform a neurologic examination soon after intubation.
- Rocuronium is longer acting but has a reversal agent if it’s necessary (81,82). If further airway management is needed, like a cricothyrotomy, the patient is already paralyzed. Rocuronium should also be used if there is concern for severe hyperkalemia (succinylcholine is a depolarizing paralytic and can result in release of potassium. Succinylcholine not recommended for myasthenia gravis; for these patients use half dose rocuronium (85).
- Several studies have evaluated administering the the paralytic before the sedative based on the onset of action for sedatives being faster than paralytics. May result in cessation of respiration without paralysis, leading to pulmonary derecruitment, CO2 retention, and hypoxia (86-88).
- 2019 study evaluated RSI medication order in ED patients undergoing ETI (89). Found administration of a paralytic before the sedative agent was associated with a reduced time from medication administration to the time of the end of the ETI attempt by 6 seconds (95% CI 0-11 seconds) (89). The difference was not clinically significant, and the risk of paralysis without sedation greatly outweighs this (90).
- 2024 study included 2,2116 patients and found first-attempt failure occurred in 54 (4.3%) patients in the paralytic-first group and 56 (5.9%) in the sedative-first group.
- May consider this, but ensure team is comfortable with it.
Should we use VL or DL?
- Two primary techniques for ETI: DL versus VL with a hyperangulated blade or standard-geometry blade (3,91-93).
- DL: uses a blade with a light source attached to a battery-contained handle to displace the tongue, manipulate the epiglottis, directly visualize the glottic structures, and pass the ETT through the vocal cords.
- VLL: uses the same components as DL but the blade contains a camera in the distal half that transmits images to a screen. See the ETT passing the glottic structures without direct line of sight (91).With hyperangulated blade, the increased curvature doesn’t allow direct visualization, but with a standard geometry VL blade, can visualize directly or with the video monitor (91,93).
- DL is the most commonly utilized technique in ED and ICU settings worldwide, but VL use has increased.
- 2024 meta-analysis including RCTs conducted in the ED and ICU found VL increased first-pass success (RR 1.12; 95% CI 1.04-1.20) and reduced esophageal intubations (RR 0.44; 95% CI 0.24-0.80) and aspiration (RR 0.63; 95% CI 0.41-0.96) (94).
- DEVICE was a multicenter RCT published in 2023 in NEJM that included 1417 patients undergoing ETI in the ED or ICU (93). For the first attempt, patients were randomized to VL or DL. 70% were intubated in the ED. VL improved first-pass attempt success compared to DL (85.1% versus 70.8%; absolute difference 14.3%; 95% CI 9.9% to 18.7%). No difference in complications (hypotension, hypoxia, vasopressor use, cardiac arrest, death, aspiration, esophageal intubation, or teeth injury). Less benefit with VL in first-pass success for those with at least 100 intubations, and DL was favored in those clinicians who had performed > 250 prior intubations (93).
- ACEP provides a level C recommendation to consider VL when available.
- Summary: VL is associated with greater first attempt success, particularly for novice intbuatiors. If you’re a more experienced intubator, go with what you’re comfortable with. No matter the device you use, you must have an established back up plan if your first attempts are unsuccessful.
When should we use a bougie?
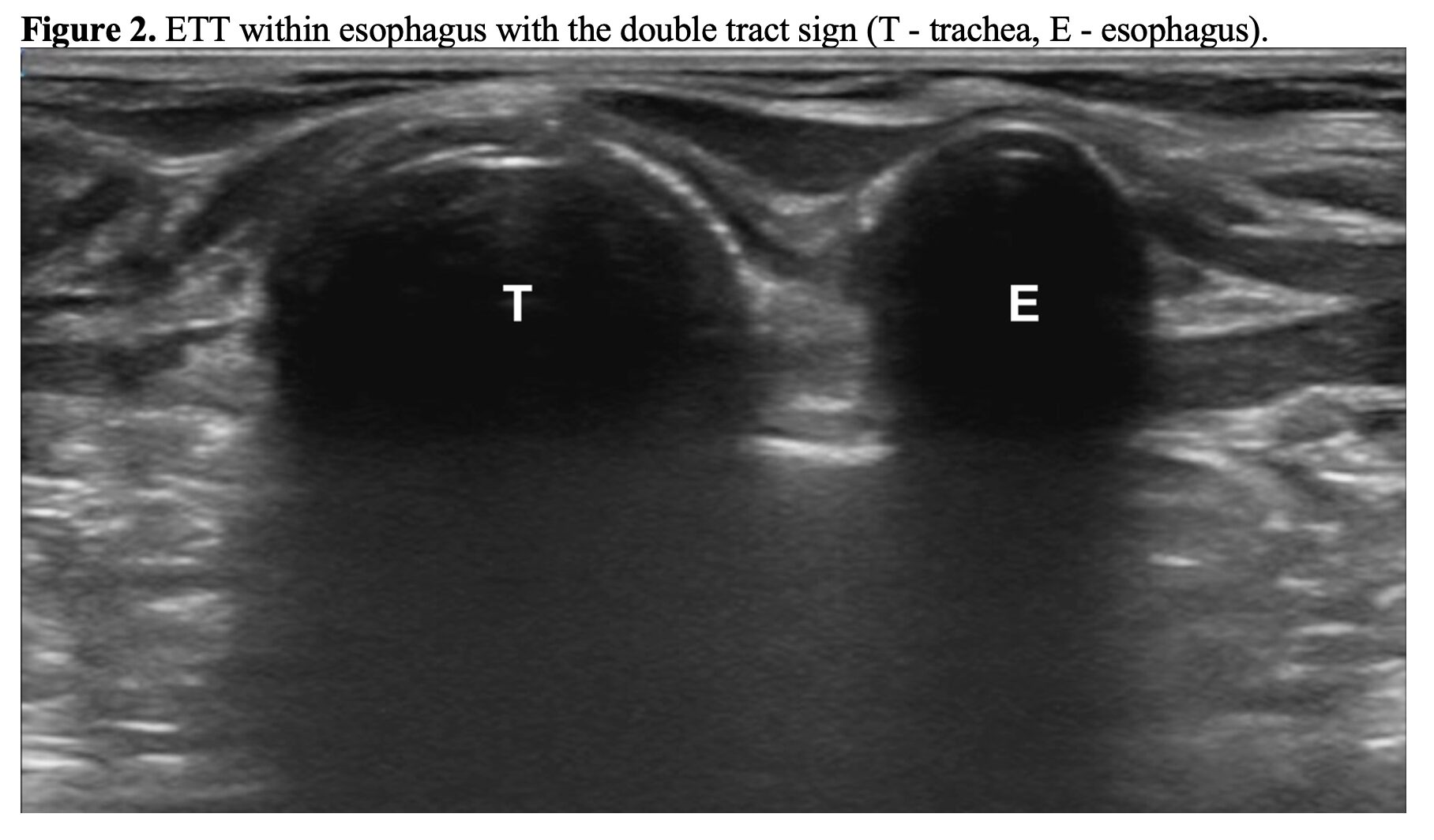
- Bougie is a flexible, 60-cm device with a small 35–40-degree angle at the distal end (coudé tip) (95). Sizes range between 10-15 French.
- Used to consider bougie only after a failed attempt, but more recent studies have looked at using a bougie on the first ETI attempt (96).
- 2018 BEAM RCT randomized patients undergoing ETI to a first attempt facilitated by bougie or ETT with stylet (97). Included 757 patients and found first-attempt success was higher with the bougie (98% versus 87%), but median duration of the attempt and incidence of hypoxia were no different. This trial was conducted at a center where bougie was commonly used (97).
- 2021 RCT with 1,102 patients found no significant difference in first-attempt success (80.4% versus 83.0%) (98).
- 2024 meta-analysis with18 studies found improved first-attempt success overall with use of a bougie (RR 1.11; 95% CI 1.06-1.17), as well as across all subgroups (95). Greatest improvement in patients with a Cormack-Lehane III or IV airway (RR 1.60; 95% 1.40-1.84) (95).
- Advantages for bougie use: improved view of passage of the bougie through the vocal cords, (lowers the likelihood of passing the ETT into the esophagus); allows ETT confirmation within the trachea by feeling the trachea rings or being held up when the bougie reaches the carina; may also facilitate advancing the ETT into a single mainstem bronchus when single lung intubation is needed (99).
- Based on the literature, a bougie likely improves first-attempt success with operators who are experienced in its use. We should be comfortable with the bougie.
How can we confirm ETT placement?
- Variety of techniques: assessing for chest rise, auscultation of breath sounds, ETT condensation, direct visualization, and quantitative or qualitative capnometry.
- Chest rise, auscultation of breath sounds, and ETT condensation are not reliable.
- Capnography can be reliable for ETT confirmation, but there are limitations.
- False positives with hypopharyngeal placement or recent ingestion of a carbonated beverage.
- False negatives when expired CO2 levels are low (cardiac arrest, flash pulmonary edema, massive pulmonary embolism) (100-108).
- POCUS: rapid and reliable means of confirming ETT placement within the trachea and looking for mainstem intubation.
- Meta-analysis found POCUS was 99% sensitive and 97% specific for confirming ETT location (109).
- How to do this? Place the linear probe tranversely on the anterior neck at the level of the suprasternal notch (102-106,109-111).
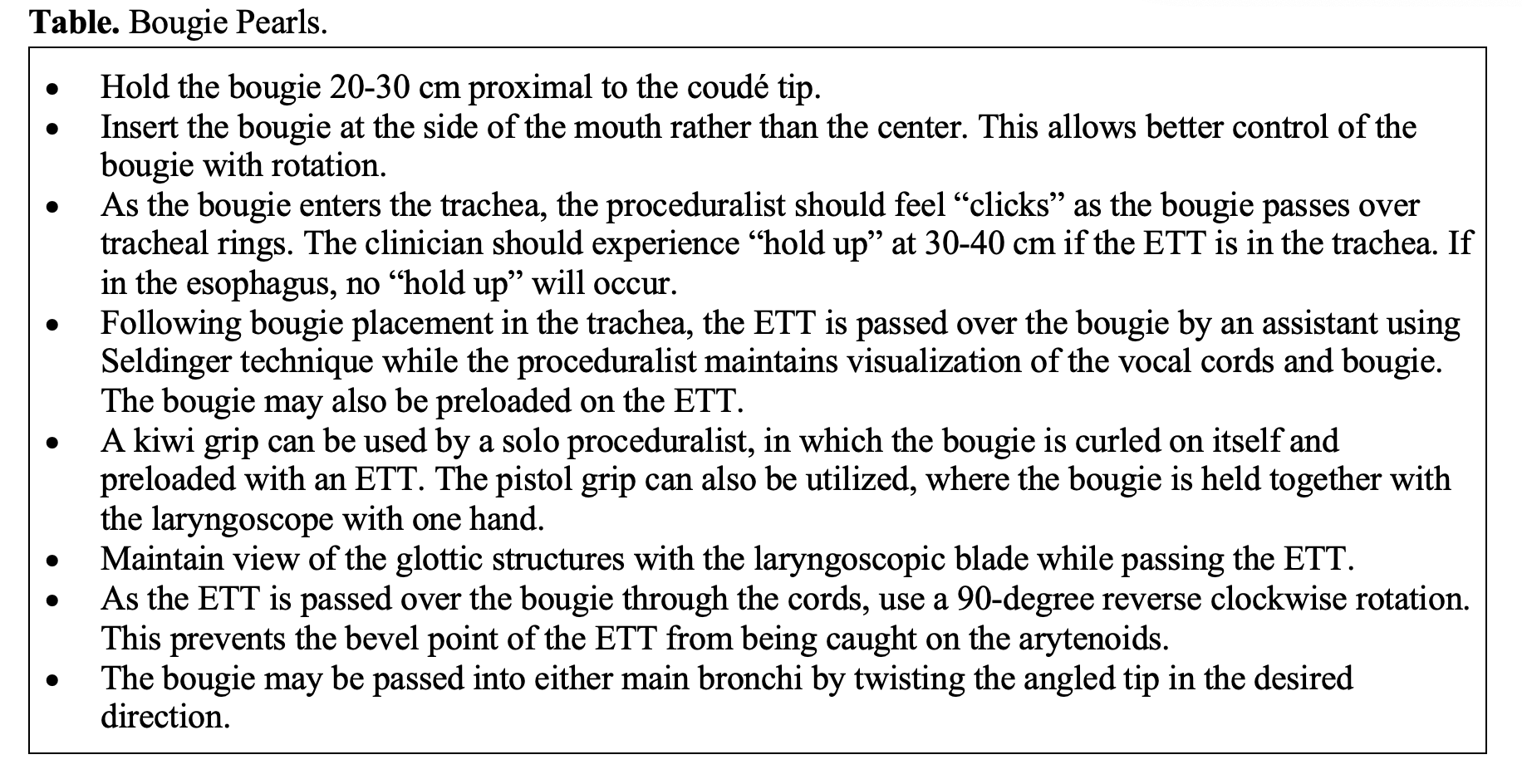
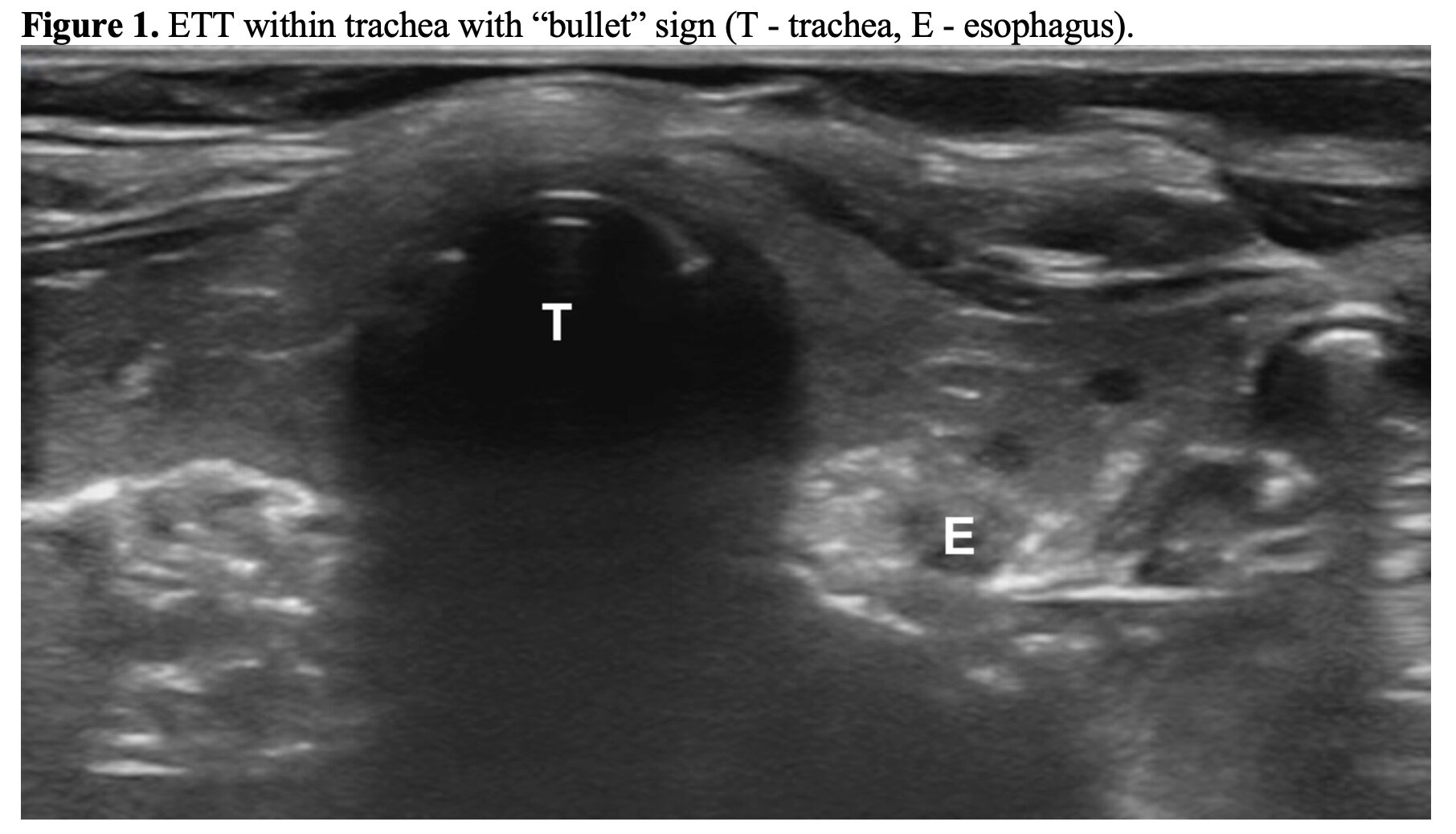
- The static technique can be performed by one clinician after ETI. Looking for a single air-mucosal interface with posterior shadowing (i.e., the “bullet” sign) to confirm ETT placement in the trachea (Figure 1). Twisting of the ETT can help facilitate visualization within the trachea (112,113). If the esophagus is intubated, you’ll see the double tract sign, or a “second” trachea (Figure 2).
- The dynamic method requires another person to evaluate for the presence of motion artifact posterior to the trachea as the ETT passes (confirming appropriate placement), or the appearance of the double tract sign (esophageal placement) (104-106). If it’s not clear, look for bilateral lung sliding (112,114).
- Once the location has been confirmed, may rotate the ultrasound probe 90 degrees clockwise to visualize the ETT cuff in relation to the cricoid and tracheal rings to determine the ETT depth (112,115).
- If bilateral sliding present, the ETT is not mainstemmed.
What should we consider for post-intubation sedation?
- Must ensure adequate sedation and analgesia as soon as the intubation is completed to reduce the risk of post-intubation awareness while paralyzed (86).
- Awareness with recall of paralysis (AWP) is associated with significant long-term sequelae: posttraumatic stress disorder, depression, and phobias (116-118).
- Several recent studies have evaluated this in the ED.
- Single-center observational study of 383 mechanically ventilated ED patients found a prevalence of AWP of 2.6%, with rocuronium placing patients at higher risk of AWP (unadjusted odds ratio 5.1; 95% CI 1.30-20.1) (119). Patients with AWP had a higher degree of perceived threat (13.4 versus 8.5; mean difference 4.9; 95% CI 0.94-8), which is a predisposing factor for posttraumatic stress disorder (119).
- 2023 study including 866 mechanically ventilated ED patients found 66 patients (7.4%; 95% 5.8-9.4) had possible (n=61) or definite (n=5) AWP (120). The specific paralytic or sedative was not significantly associated with recall.
- 2022 study of 388 mechanically ventilated ED patients found 3.4% (13) had AWP, with the majority of these patients receiving rocuronium (12/13; 92.3%) (121). These patients had higher threat perception scale scores (121).
- Summary:
- Based on the current literature, a significant proportion of patients experience AWP. No matter the paralytic or sedative agent used for RSI, must provide adequate post-intubation sedation for patient comfort. Also helps with mechanical ventilator synchrony and reduces the work of breathing. Order post-intubation medications and have them in the room when the induction medication is being administered. Administer sedative and analgesic immediately following ETI.
Summary:
- ETI is an essential skill in emergency medicine.
- There are several tools that use anatomic and physiologic factors, and these can assist in predicting a difficult airway, but do not use them in isolation. Always assume the intubation will be difficult, and have a backup plan.
- Predictors of decompensation: hypotension, apnea/oxygen, RV failure, and acidosis.
- Use preoxygenation and apneic oxygenation to reduce the risk of hypoxemia and decompensation.
- Both etomidate and ketamine are reasonable for induction.
- May use either higher-dose rocuronium or succinylcholine for paralysis.
- VL demonstrates higher first pass success for novice intubators.
- In those who are experienced with its use, a bougie can also improve first pass success.
- There are several options for confirming tube placement, and POCUS can be an adjunct.
- No matter what agents used for induction and paralysis, post-intubation sedation is absolutely essential.
References:
- National Hospital Ambulatory Medical Care Survey. 2018 emergency department summary tables; 2018.
- Brown CA 3rd, Bair AE, Pallin DJ, Walls RM; NEAR III Investigators. Techniques, success, and adverse events of emergency department adult intubations. Ann Emerg Med. 2015 Apr;65(4):363-370.e1.
- Brown CA 3rd, Kaji AH, Fantegrossi A, et al; National Emergency Airway Registry (NEAR) Investigators. Video Laryngoscopy Compared to Augmented Direct Laryngoscopy in Adult Emergency Department Tracheal Intubations: A National Emergency Airway Registry (NEAR) Study. Acad Emerg Med. 2020 Feb;27(2):100-108.
- Centers for Disease Control and Prevention. Emergency Department Visits.Available at https://www.cdc.gov/nchs/fastats/emergency-department.htm. Accessed May 28, 2024.
- Xia M, Ma W, Zuo M, et al. Expert consensus on difficult airway assessment. Hepatobiliary Surg Nutr. 2023 Aug 1;12(4):545-566.
- Park L, Zeng I, Brainard A. Systematic review and meta-analysis of first-pass success rates in emergency department intubation: Creating a benchmark for emergency airway care. Emerg Med Australas. 2017 Feb;29(1):40-47.
- Maguire S, Schmitt PR, Sternlicht E, Kofron CM. Endotracheal Intubation of Difficult Airways in Emergency Settings: A Guide for Innovators. Med Devices (Auckl). 2023 Jul 18;16:183-199.
- Kim C, Kang HG, Lim TH, et al. What factors affect the success rate of the first attempt at endotracheal intubation in emergency departments? Emerg Med J. 2013 Nov;30(11):888-92.
- Koh W, Kim H, Kim K, et al Encountering unexpected difficult airway: relationship with the intubation difficulty scale. Korean J Anesthesiol. 2016 Jun;69(3):244-9.
- Jaber S, Amraoui J, Lefrant JY, et al. Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Crit Care Med 2006;34:2355-61.
- Schwartz DE, Matthay MA, Cohen NH. Death and other complications of emergency airway management in critically ill adults. A prospective investigation of 297 tracheal intubations. Anesthesiology 1995;82:367-76.
- Griesdale DE, Bosma TL, Kurth T, et al. Complications of endotracheal intubation in the critically ill. Intensive Care Med 2008;34:1835-42.
- Sakles JC, Douglas MJK, Hypes CD, Patanwala AE, Mosier JM. Management of Patients with Predicted Difficult Airways in an Academic Emergency Department. J Emerg Med. 2017 Aug;53(2):163-171. d
- Martin LD, Mhyre JM, Shanks AM, Tremper KK, Kheterpal S. 3,423 emergency tracheal intubations at a university hospital: airway outcomes and complications. Anesthesiology. 2011 Jan;114(1):42-8.
- Bair AE, Caravelli R, Tyler K, Laurin EG. Feasibility of the preoperative Mallampati airway assessment in emergency department patients. J Emerg Med. 2010 Jun;38(5):677-80.
- Langeron O, Masso E, Huraux C, et al. Prediction of difficult mask ventilation. 2000 May;92(5):1229-36.
- Kheterpal S, Han R, Tremper KK, et al. Incidence and predictors of difficult and impossible mask ventilation. Anesthesiology. 2006 Nov;105(5):885-91.
- Kheterpal S, Martin L, Shanks AM, Tremper KK. Prediction and outcomes of impossible mask ventilation: a review of 50,000 anesthetics. Anesthesiology. 2009 Apr;110(4):891-7.
- Nørskov AK, Wetterslev J, Rosenstock CV, et al; Collaborators. Prediction of difficult mask ventilation using a systematic assessment of risk factors vs. existing practice – a cluster randomised clinical trial in 94,006 patients. Anaesthesia. 2017 Mar;72(3):296-308.
- Moon TS, Fox PE, Somasundaram A, et al. The influence of morbid obesity on difficult intubation and difficult mask ventilation. J Anesth. 2019 Feb;33(1):96-102.
- Lundstrøm LH, Møller AM, Rosenstock C, et al. High body mass index is a weak predictor for difficult and failed tracheal intubation: a cohort study of 91,332 consecutive patients scheduled for direct laryngoscopy registered in the Danish Anesthesia Database. Anesthesiology. 2009 Feb;110(2):266-74.
- Juvin P, Lavaut E, Dupont H, et al. Difficult tracheal intubation is more common in obese than in lean patients. Anesth Analg. 2003 Aug;97(2):595-600.
- Connor CW, Segal S. The importance of subjective facial appearance on the ability of anesthesiologists to predict difficult intubation. Anesth Analg. 2014 Feb;118(2):419-427.
- Naguib M, Scamman FL, O’Sullivan C, et al. Predictive performance of three multivariate difficult tracheal intubation models: a double-blind, case-controlled study. Anesth Analg. 2006 Mar;102(3):818-24.
- Detsky ME, Jivraj N, Adhikari NK, et al. Will This Patient Be Difficult to Intubate?: The Rational Clinical Examination Systematic Review. JAMA. 2019 Feb 5;321(5):493-503.
- Lundstrøm LH, Vester-Andersen M, Møller AM, Charuluxananan S, et al; Danish Anaesthesia Database. Poor prognostic value of the modified Mallampati score: a meta-analysis involving 177 088 patients. Br J Anaesth. 2011 Nov;107(5):659-67.
- Samsoon GL, Young JR. Difficult tracheal intubation: a retrospective study. Anaesthesia. 1987 May;42(5):487-90.
- Mallampati SR, Gatt SP, Gugino LD, et al. A clinical sign to predict difficult tracheal intubation: a prospective study. Can Anaesth Soc J. 1985 Jul;32(4):429-34.
- Lee A, Fan LT, Gin T, et al. A systematic review (meta-analysis) of the accuracy of the Mallampati tests to predict the difficult airway. Anesth Analg. 2006 Jun;102(6):1867-78.
- Roth D, Pace NL, Lee A, et al. Airway physical examination tests for detection of difficult airway management in apparently normal adult patients. Cochrane Database Syst Rev. 2018 May 15;5(5):CD008874.
- Green SM, Roback MG. Is the Mallampati Score Useful for Emergency Department Airway Management or Procedural Sedation? Ann Emerg Med. 2019 Aug;74(2):251-259.
- Crosby ET. Considerations for airway management for cervical spine surgery in adults. Anesthesiol Clin. 2007 Sep;25(3):511-33, ix.
- Crosby ET. Airway management in adults after cervical spine trauma. Anesthesiology. 2006 Jun;104(6):1293-318.
- Faramarzi E, Soleimanpour H, Khan ZH, et al. Upper lip bite test for prediction of difficult airway: A systematic review. Pak J Med Sci. 2018 Jul-Aug;34(4):1019-1023.
- Bair AE, Chima R. The inaccuracy of using landmark techniques for cricothyroid membrane identification: a comparison of three techniques. Acad Emerg Med. 2015 Aug;22(8):908-14.
- Aslani A, Ng SC, Hurley M, et al. Accuracy of identification of the cricothyroid membrane in female subjects using palpation: an observational study. Anesth Analg. 2012 May;114(5):987-92.
- Gottlieb M, O’Brien JR, Ferrigno N, Sundaram T. Point-of-care ultrasound for airway management in the emergency and critical care setting. Clin Exp Emerg Med. 2024 Mar;11(1):22-32.
- Carsetti A, Sorbello M, Adrario E, et al. Airway ultrasound as predictor of difficult direct laryngoscopy: a systematic review and meta-analysis. Anesth Analg 2022; 134:740-50.
- Andruszkiewicz P, Wojtczak J, Sobczyk D, et al. Effectiveness and validity of sonographic upper airway evaluation to predict difficult laryngoscopy. J Ultrasound Med 2016; 35:2243-52.
- Petrisor C, Szabo R, Constantinescu C, et al. Ultrasound-based assessment of hyomental distances in neutral, ramped, and maximum hyperextended positions, and derived ratios, for the prediction of difficult airway in the obese population: a pilot diagnostic accuracy study. Anaesthesiol Intensive Ther 2018; 50:110-6.
- Yadav NK, Rudingwa P, Mishra SK, Pannerselvam S. Ultrasound measurement of anterior neck soft tissue and tongue thickness to predict difficult laryngoscopy: an observational analytical study. Indian J Anaesth 2019; 63:629-34.
- Yao W, Wang B. Can tongue thickness measured by ultrasonography predict difficult tracheal intubation? Br J Anaesth 2017; 118:601-9.
- Alerhand S. Ultrasound for identifying the cricothyroid membrane prior to the anticipated difficult airway. Am J Emerg Med. 2018 Nov;36(11):2078-2084.
- Rai Y, You-Ten E, Zasso F, et al. The role of ultrasound in front-of-neck access for cricothyroid membrane identification: A systematic review. J Crit Care. 2020 Dec;60:161-168.
- Downing J, Yardi I, Ren C, et al. Prevalence of peri-intubation major adverse events among critically ill patients: A systematic review and meta analysis. Am J Emerg Med. 2023 Sep;71:200-216.
- Russotto V, Myatra SN, Laffey JG, et al; INTUBE Study Investigators. Intubation Practices and Adverse Peri-intubation Events in Critically Ill Patients From 29 Countries. JAMA. 2021 Mar 23;325(12):1164-1172.
- Mosier JM, Hypes CD, Sakles JC. Understanding preoxygenation and apneic oxygenation during intubation in the critically ill. Intensive Care Med. 2017;43:226-8.
- Mosier JM, Joshi R, Hypes C, Pacheco G, Valenzuela T, Sakles JC. The Physiologically Difficult Airway. West J Emerg Med. 2015 Dec;16(7):1109-17.
- Weingart SD. Preoxygenation, reoxygenation, and delayed sequence intubation in the emergency department. J Emerg Med. 2011 Jun;40(6):661-7.
- Weingart SD, Levitan RM. Preoxygenation and prevention of desaturation during emergency airway management. Ann Emerg Med. 2012 Mar;59(3):165-75.e1.
- Kostura M, Smalley C, Koyfman A, Long B. Right heart failure: A narrative review for emergency clinicians. Am J Emerg Med. 2022 Aug;58:106-113.
- Gleason JM, Christian BR, Barton ED. Nasal Cannula Apneic Oxygenation Prevents Desaturation During Endotracheal Intubation: An Integrative Literature Review. West J Emerg Med. 2018 Mar;19(2):403-411.
- Futier E, Constantin JM, Pelosi P, et al. Noninvasive ventilation and alveolar recruitment maneuver improve respiratory function during and after intubation of morbidly obese patients: a randomized controlled study. Anesthesiology. 2011 Jun;114(6):1354-63.
- Gibbs KW, Semler MW, Driver BE, et al, for the PREOXI Investigators and the Pragmatic Critical Care Research Group. Noninvasive Ventilation for Preoxygenationduring Emergency Intubation. N Engl J Med. DOI: 10.1056/NEJMoa2313680.
- Binks MJ, Holyoak RS, Melhuish TM, et al. Apnoeic oxygenation during intubation in the intensive care unit: A systematic review and meta-analysis. Heart Lung. 2017 Nov-Dec;46(6):452-457.
- Binks MJ, Holyoak RS, Melhuish TM, et al. Apneic oxygenation during intubation in the emergency department and during retrieval: A systematic review and meta-analysis. Am J Emerg Med. 2017 Oct;35(10):1542-1546.
- Pavlov I, Medrano S, Weingart S. Apneic oxygenation reduces the incidence of hypoxemia during emergency intubation: A systematic review and meta-analysis. Am J Emerg Med. 2017 Aug;35(8):1184-1189.
- White LD, Melhuish TM, White LK, Wallace LA. Apnoeic oxygenation during intubation: a systematic review and meta-analysis. Anaesth Intensive Care. 2017 Jan;45(1):21-27. d
- White LD, Vlok RA, Thang CY, et al. Oxygenation during the apnoeic phase preceding intubation in adults in prehospital, emergency department, intensive care and operating theatre environments. Cochrane Database Syst Rev. 2023 Aug 2;8(8):CD013558.
- Oliveira J E Silva L, Cabrera D, Barrionuevo P, et al. Effectiveness of Apneic Oxygenation During Intubation: A Systematic Review and Meta-Analysis. Ann Emerg Med. 2017 Oct;70(4):483-494.e11. Chua MT, Ng WM, Lu Q, et al. Pre- and apnoeic high-flow oxygenation for rapid sequence intubation in the emergency department (the Pre-AeRATE trial): a multicentre randomised controlled trial. Ann Acad Med Singap 2022; 51:149–160.
- Acquisto NM, Mosier JM, Bittner EA, et al. Society of Critical Care Medicine Clinical Practice Guidelines for Rapid Sequence Intubation in the Critically Ill Adult Patient. Crit Care Med. 2023 Oct 1;51(10):1411-1430.
- Hohenstein C, Merz S, Eppler F, et al; European Society for Emergency Medicine. Emergency airway management: an EUSEM statement with regard to the guidelines of the Society of Critical Care Medicine. Eur J Emerg Med. 2024 Apr 1;31(2):83-85.
- Gottlieb M, Chien N, Long B. Managing Alcohol Withdrawal Syndrome. Ann Emerg Med. 2024 Mar 25:S0196-0644(24)00105-7.
- Folino TB, Muco E, Safadi AO, et al. Propofol. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430884/
- Williams LM, Boyd KL, Fitzgerald BM. Etomidate. [Updated 2023 Jun 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535364/
- Jabre P, Combes X, Lapostolle F, et al.; KETASED Collaborative Study Group. Etomidate versus ketamine for rapid sequence intubation in acutely ill patients: a multicentre randomised controlled trial. Lancet. 2009;374:293–300.
- Ishimaru T, Goto T, Takahashi J, et al.; Japanese Emergency Medicine Network Investigators. Association of ketamine use with lower risks of post-intubation hypotension in hemodynamically-unstable patients in the emergency department. Sci Rep. 2019; 9:17230.
- Rosenbaum SB, Gupta V, Patel P, et al. Ketamine. [Updated 2024 Jan 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470357/
- Koroki T, Kotani Y, Yaguchi T, et al. Ketamine versus etomidate as an induction agent for tracheal intubation in critically ill adults: a Bayesian meta-analysis. Crit Care. 2024 Feb 17;28(1):48.
- Sharda SC, Bhatia MS. Etomidate Compared to Ketamine for Induction during Rapid Sequence Intubation: A Systematic Review and Meta-analysis. Indian J Crit Care Med. 2022 Jan;26(1):108-113.
- Kotani Y, Piersanti G, Maiucci G, et al. Etomidate as an induction agent for endotracheal intubation in critically ill patients: A meta-analysis of randomized trials. J Crit Care. 2023 Oct;77:154317.
- Li J, Murphy-Lavoie H, Bugas C, et al. Complications of emergency intubation with and without paralysis. Am J Emerg Med. 1999 Mar;17(2):141-3.
- Wilcox SR, Bittner EA, Elmer J, et al. Neuromuscular blocking agent administration for emergent tracheal intubation is associated with decreased prevalence of procedure-related complications. Crit Care Med. 2012 Jun;40(6):1808-13.
- Okubo M, Gibo K, Hagiwara Y, et al; Japanese Emergency Medicine Network Investigators. The effectiveness of rapid sequence intubation (RSI) versus non-RSI in emergency department: an analysis of multicenter prospective observational study. Int J Emerg Med. 2017 Dec;10(1):1.
- Raghavendra T. Neuromuscular blocking drugs: Discovery and development.J R Soc Med. 2002;95(7):363—367.
- Hager HH, Burns B. Succinylcholine Chloride. [Updated 2023 Feb 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499984
- Wicks TC. The pharmacology of rocuronium bromide (ORG 9426). AANA J. 1994 Feb;62(1):33-8.
- Jain A, Wermuth HR, Dua A, et al. Rocuronium. [Updated 2024 Feb 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539888/
- Tran DTT, Newton EK, Mount VAH, et al. Rocuronium vs. succinylcholine for rapid sequence intubation: a Cochrane systematic review. 2017 Jun;72(6):765-777.
- April MD, Arana A, Pallin DJ, et al; NEAR Investigators. Emergency Department Intubation Success With Succinylcholine Versus Rocuronium: A National Emergency Airway Registry Study. Ann Emerg Med. 2018 Dec;72(6):645-653.
- Rech M, Gottlieb M. Sugammadex Should Be Used to Reverse Rocuronium in Emergency Department Patients With Neurologic Injuries. Ann Emerg Med. 2024.
- Chandrasekhar K, Togioka BM, Jeffers JL. Sugammadex. [Updated 2023 May 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.Available from: https://www.ncbi.nlm.nih.gov/books/NBK470263/
- Taha SK, El-Khatib MF, Baraka AS, et al. Effect of suxamethonium vs rocuronium on onset of oxygen desaturation during apnoea following rapid sequence induction. Anaesthesia. 2010 Apr;65(4):358-61.
- Tang L, Li S, Huang S, Ma H, Wang Z. Desaturation following rapid sequence induction using succinylcholine vs. rocuronium in overweight patients. Acta Anaesthesiol Scand. 2011 Feb;55(2):203-8.
- Roper J, Fleming ME, Long B, Koyfman A. Myasthenia Gravis and Crisis: Evaluation and Management in the Emergency Department. J Emerg Med. 2017 Dec;53(6):843-853.
- Nelson JM, Morell RC, Butterworth JF 4th. Rocuroniumversus succinylcholine for rapid-sequence induction using a variation of the timing principle. J Clin Anesth1997;9:317–20.16.
- Sieber TJ, Zbinden AM, Curatolo M, Shorten GD. Tracheal intubation with rocuronium using the” timing principle”. Anesth Analg. 1998;86:1137–40.
- Chatrath V, Singh I, Chatrath R, Arora N. Comparison of intubating conditions of rocuronium bromide andvecuronium bromide with succinylcholine using “timing principle”. J Anaesthesiol Clin Pharmacol 2010;26:493–7.
- Driver BE, Klein LR, Prekker ME, et al. Drug Order in Rapid Sequence Intubation. Acad Emerg Med. 2019 Sep;26(9):1014-1021.
- Gottlieb M, Carlson JN. Speechless: Awareness With Recall of Paralysis in the Emergency Department Setting. Ann Emerg Med. 2021 May;77(5):545-546.
- Berkow LC, Morey TE, Urdaneta F. The technology of video laryngoscopy. Anesth Analg 2018;126:1527-1534.
- Hansel J, Rogers AM, Lewis SR, et al. Videolaryngoscopy versus direct laryngoscopy for adults undergoing tracheal intubation. Cochrane Database Syst Rev. 2022 Apr 4;4(4):CD011136.
- Prekker ME, Driver BE, Trent SA, et al; DEVICE Investigators and the Pragmatic Critical Care Research Group. Video versus Direct Laryngoscopy for Tracheal Intubation of Critically Ill Adults. N Engl J Med. 2023 Aug 3;389(5):418-429.
- Araújo B, Rivera A, Martins S, et al. Video versus direct laryngoscopy in critically ill patients: an updated systematic review and meta-analysis of randomized controlled trials. Crit Care. 2024 Jan 2;28(1):1.
- von Hellmann R, Fuhr N, Ward A Maia I, et al. Effect of Bougie Use on First-Attempt Success in Tracheal Intubations: A Systematic Review and Meta-Analysis. Ann Emerg Med. 2024 Feb;83(2):132-144.
- Gottlieb M, Fix M. Bougie First: Rethinking the Modern Airway Algorithm. Ann Emerg Med. 2024 Feb;83(2):145-146.
- Driver BE, Prekker ME, Klein LR, et al. Effect of Use of a Bougie vs Endotracheal Tube and Stylet on First-Attempt Intubation Success Among Patients With Difficult Airways Undergoing Emergency Intubation: A Randomized Clinical Trial. JAMA. 2018 Jun 5;319(21):2179-2189.
- Driver BE, Semler MW, Self WH, et al; BOUGIE Investigators and the Pragmatic Critical Care Research Group. Effect of Use of a Bougie vs Endotracheal Tube With Stylet on Successful Intubation on the First Attempt Among Critically Ill Patients Undergoing Tracheal Intubation: A Randomized Clinical Trial. JAMA. 2021 Dec 28;326(24):2488-2497.
- Gottlieb M, Sharma V, Field J, Rozum M, Bailitz J. Utilization of a gum elastic bougie to facilitate single lung intubation. Am J Emerg Med. 2016 Dec;34(12):2408-2410.
- Long B, Koyfman A, Vivirito MA. Capnography in the Emergency Department: A Review of Uses, Waveforms, and Limitations. J Emerg Med. 2017 Dec;53(6):829-842.
- Gottlieb M, Holladay D, Peksa GD. Ultrasonography for the Confirmation of Endotracheal Tube Intubation: A Systematic Review and Meta-Analysis. Ann Emerg Med. 2018 Dec;72(6):627-636.
- Gottlieb M, Bailitz J. Can Transtracheal Ultrasonography Be Used to Verify Endotracheal Tube Placement? Ann Emerg Med. 2015;66(4):394–5.
- Sahu AK, Bhoi S, Aggarwal P, et al. Endotracheal Tube Placement Confirmation by Ultrasonography: A Systematic Review and Meta-Analysis of more than 2500 Patients. J Emerg Med. 2020 Aug;59(2):254-264.
- Gottlieb M, O’Brien JR, Ferrigno N, Sundaram T. Point-of-care ultrasound for airway management in the emergency and critical care setting. Clin Exp Emerg Med. 2024 Mar;11(1):22-32.
- Gottlieb M, Holladay D, Burns KM, et al. Ultrasound for airway management: An evidence-based review for the emergency clinician. Am J Emerg Med. 2020;38(5):1007-1013.
- Gottlieb M, Olszynski P, Atkinson P. Just the facts: point-of-care ultrasound for airway management. CJEM. 2021;23(3):277-279.
- Li J. Capnography alone is imperfect for endotracheal tube placement confirmation during emergency intubation. J Emerg Med. 2001;20(3):223-229.
- Eichlseder M, Eichinger M, Pichler A, et al. Out-of-Hospital Arterial to End-Tidal Carbon Dioxide Gradient in Patients With Return of Spontaneous Circulation After Out-of-Hospital Cardiac Arrest: A Retrospective Study. Annals of Emergency Medicine. Published online April 2023:S0196064423001750.
- Gottlieb M, Holladay D, Peksa GD. Ultrasonography for the Confirmation of Endotracheal Tube Intubation: A Systematic Review and Meta-Analysis. Ann Emerg Med. 2018;72(6):627-636.
- Gottlieb M, O’Brien JR, Patel D. SONO case series: point-of-care ultrasound for intubation confirmation. Emerg Med J. 2024 May 28;41(6):379-381.
- Gottlieb M, Nakitende D, Sundaram T, et al. Comparison of Static versus Dynamic Ultrasound for the Detection of Endotracheal Intubation. West J Emerg Med. 2018 Mar;19(2):412-416.
- Gottlieb M, Berzins D, Hartrich M, et al. Diagnostic accuracy of ultrasound to confirm endotracheal tube depth. Am J Emerg Med. 2022 Dec;62:9-13.
- Gottlieb M, Burns K, Holladay D, Chottiner M, Shah S, Gore SR. Impact of endotracheal tube twisting on the diagnostic accuracy of ultrasound for intubation confirmation. Am J Emerg Med. 2020 Jul;38(7):1332-1334.
- Gottlieb M, Alerhand S, Long B. Point-of-Care Ultrasound for Intubation Confirmation of COVID-19 Patients. West J Emerg Med. 2020 Aug 17;21(5):1042-1045.
- Gottlieb M, Cozzi N, Hartrich M, et al. Comparison of dynamic versus static ultrasound to confirm endotracheal tube depth. Am J Emerg Med. 2023 Dec;74:17-20.
- Cook TM, Andrade J, Bogod DG, et al; Royal College of Anaesthetists; Association of Anaesthetists of Great Britain and Ireland. 5th National Audit Project (NAP5) on accidental awareness during general anaesthesia: patient experiences, human factors, sedation, consent, and medicolegal issues. Br J Anaesth. 2014 Oct;113(4):560-74.
- Leslie K, Chan MT, Myles PS, et al. Posttraumatic stress disorder in aware patients from the B-aware trial. Anesth Analg. 2010 Mar 1;110(3):823-8.
- Pandit JJ, Andrade J, Bogod DG, et al; Royal College of Anaesthetists; Association of Anaesthetists of Great Britain and Ireland. 5th National Audit Project (NAP5) on accidental awareness during general anaesthesia: summary of main findings and risk factors. Br J Anaesth. 2014 Oct;113(4):549-59.
- Pappal RD, Roberts BW, Mohr NM, et al. The ED-AWARENESS Study: A Prospective, Observational Cohort Study of Awareness With Paralysis in Mechanically Ventilated Patients Admitted From the Emergency Department. Ann Emerg Med. 2021 May;77(5):532-544.
- Driver BE, Prekker ME, Wagner E, et al. Recall of Awareness During Paralysis Among ED Patients Undergoing Tracheal Intubation. 2023 Feb;163(2):313-323.
- Fuller BM, Pappal RD, Mohr NM, et al. Awareness With Paralysis Among Critically Ill Emergency Department Patients: A Prospective Cohort Study. Crit Care Med. 2022 Oct 1;50(10):1449-1460.
- American College of Emergency Physicians Clinical Policies Subcommittee (Writing Committee) on Airway Management; Godwin SA, Hahn SA, Friedman BW, et al. Clinical Policy: Critical Issues in the Management of Adult Patients Requiring Endotracheal Intubation in the Emergency Department. Ann Emerg Med. 2025 Aug;86(2):e29-e68.
- Long B, Gottlieb M. Emergency medicine updates: Endotracheal intubation. Am J Emerg Med. 2024 Nov;85:108-116.






