Authors: Laurence Baril, MD (EM Resident Physician, Laval University) // Reviewed by: James Dazhe Cao, MD (@JamesCaoMD, Associate Professor of EM, Medical Toxicology, UT Southwestern Medical Center, Dallas, TX); Alex Koyfman, MD (@EMHighAK); and Brit Long, MD (@long_brit)
Case:
A 30-year-old male without past medical history is brought to you from the airport. The policeman accompanying him tells you that he was caught swallowing packets in the airport hall when he noticed that the police officers were watching him. For now, his only symptoms are a mild agitation and diaphoresis. He denies any illicit drug use or packet ingestion. On exam, the patient looks anxious. He has a blood pressure of 155/89, heart rate of 115, respiratory rate of 14, SpO2 98% on room air, and temperature of 37.2°C (99°F). He does not demonstrate any toxidrome on exam and does not have any abdominal tenderness.
Questions:
- Where do you put this patient in your ED?
- Do you order investigations?
- Do you start any treatment up front?
Background and Definitions:
Ingestion of illicit drugs for transportation is not a frequent presentation but can be a challenging one. Those patients have been classified in three groups, according to the mechanism of ingestion:
- Body packers
- Body stuffers
- Body pushers
The first and best known is the body packers. These patients intentionally ingest cautiously prepared drug packets in an important quantity in order to transport them. The packets are resistant and do not tend to break by passing through the digestive tract. However, if they do break, the consequences might be dramatic, due to the impressive quantity of drug now released in the intestines, potentially inducing a fatal overdose.
The second group of patients is the body stuffers. These patients ingest drug packets that are much more artisanal and fragile, in a hurry, in a moment when they feel threatened by law-enforcing officers. The amount of drug ingested is often smaller, but the packets are more prone to break and induce a significant toxicity.
The final group is the body pushers, meaning people who hide drug packets in various orifices (rectum, vagina, nose, ears, etc.). They represent a very heterogenous group, often co-occurring with one of the two previously described modes of ingestion.
When to suspect it?
Drug-transporting patients may present in a variety of ways. They might be reported by police and other law-enforcement officers and not be symptomatic of their ingestion. They might present with gastrointestinal complications (perforation, obstruction, etc.). Finally, they can show signs of toxicity, ranging from mild agitation or sedation to cardiac arrest.
How should we evaluate these patients?
When faced with a history of illicit drug ingestion for transport, the provider should try to understand what drug was ingested and in what type of packaging. The clinician must keep in mind that the patient might have incentives to hide elements and provide an incomplete or changing history. We must keep a high index of suspicion for these reasons.
The first step is to evaluate the patient and look for signs of complications from the ingestion. Leakage of the packets may lead to intoxication by the ingested drug. The most often seen ingestions are cocaine and heroin, but cannabinoids, fentanyl, and other stimulants have been reported.1 The toxidrome will therefore usually be either opioid or sympathomimetic. Of note, patients are often mildly tachycardic and hypertensive due to their recent detention. It might be useful to observe the patient and see if these signs resolve by themselves and look for other signs of toxidrome (agitation, mydriasis, arrhythmia, diminished peristaltic, diaphoresis, etc.). The other complications to look for clinically are anatomical including obstruction, perforation, and/or bowel ischemia. A thorough physical exam including a good abdominal evaluation is critical for the patient management.2,3,4,5
What test to order?
The gold standard for identifying body packers is the CT scan without contrast. The sensitivity has been reported up to 100% with a good specificity. This modality enables us to count the number of packets ingested and to look for complications. If anatomical complications are suspected based on the physical exam, a CT with contrast can enhance the sensitivity.2,3,4
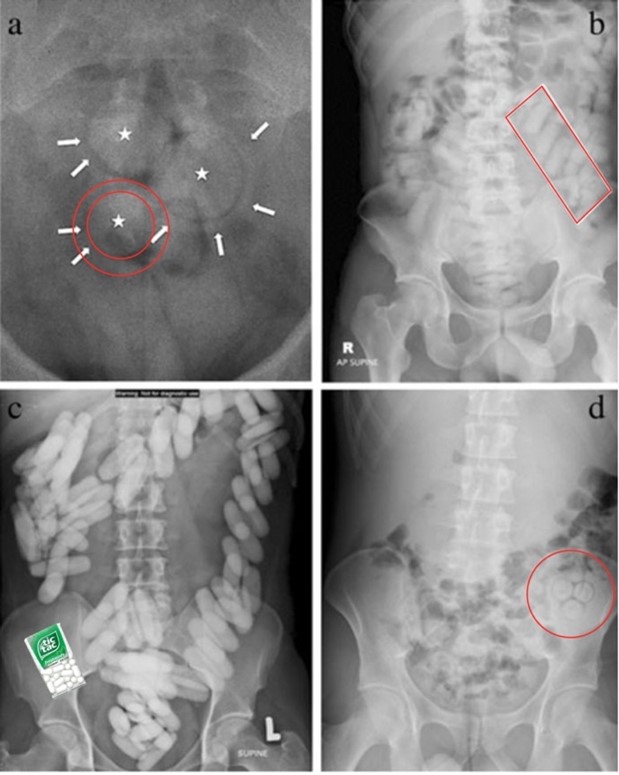
Abdominal X-rays were historically the first exam modalities to identify drug packets. However, most recent studies identified a sensitivity of 60–90% for body packers and much lower for body stuffers or pushers. Some clinical findings on X-rays are the “double condom sign” (a), the “parallelism sign” (b), the “Tic-tac sign” (c) and the “Rosette Sign (d).6 However, body packers develop innovative ways such aluminum foil and liquid drugs to make the packets less radio-opaque. Additionally, many false positives have been reported with stools, calcifications, and other intestinal foreign bodies. So, in the end, what to think of the X-ray? It can certainly be a screening tool, but we have to keep in mind that it is neither sensitive nor specific. Some experts advocate for the use of contrast-enhanced or plain abdominal X-ray to confirm the passage of packets if those were proven to be radio-opaque in the first place. In patients for whom we would prefer to limit exposure to radiation (pediatrics and pregnant women), the use of ultrasound has been described, with fairly good results (sensitivity 91%, specificity 70%).7
MRI is also an option for pregnant patient, but this is mostly an expert recommendation and case reports rather than strong evidence-based medicine.8 (Figure 1)
What about the urine drug screen?
Looking for an indication for the urine drug screen? Unfortunately, it is not the case here. The only situation in which this test would be useful is if it was initially negative, and then turned positive because of leaking packets. However, this condition is quite rare, and patients transporting illicit drugs have often used some in the last hours of days, which ends up in positive tests. Those tests also have their loads of false positives and false negatives and generally are not helpful in guiding management of body packers, stuffers, or pushers.
Your patient has 40 drug packets in his bowel. What to do now?
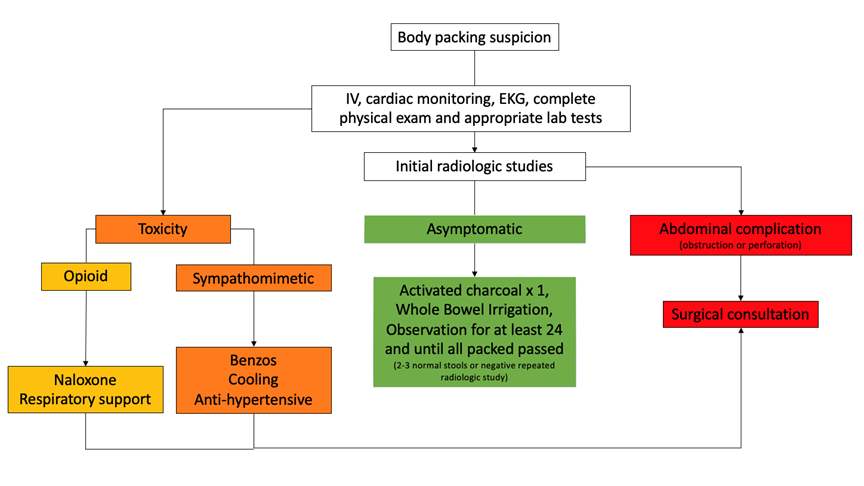
Three scenarios are possible at this point (Figure 2):
- First is the asymptomatic patient with no toxidrome or abdominal complication. In this group, most experts recommend whole bowel irrigation with or without activated charcoal an hour before starting the irrigation. Activated charcoal is more clearly recommended for the management of body stuffers, whose packets are at high risk of breaking, but remains controversial in the management of body packers. An in vitro study showed that the use of activated charcoal preceding whole bowel irrigation could decrease to absorption of cocaine more than any of these interventions in isolation.9 All asymptomatic patients must be observed at least 6 hours in the emergency department to watch for signs of toxicity or complication.7 They can be discharged after if all the packets have been expelled, confirmed by 2 bowel movements without any packets, or a negative radiological testing. The only indication to operate on an asymptomatic patient would be failure to pass all packets or an important number of packets in the stomach that are judged improbable to pass the pylorus. In this case, the recommended approach would be laparotomy, since endoscopic or laparoscopic approach results in a risk of rupturing the packets and releasing the drug.10
- The next group of patients is the one with abdominal complications. Those can be obstruction or perforation of the esophagus, stomach, or intestines. The diagnosis is suspected by the physical exam, confirmed by X-ray or CT, and taken care of in the operating room. In these cases, our role in the ED is to provide good supportive care and urgent surgical consultation.
- The last group of patients is the one showing signs of drug toxicity. This can range from mild symptoms to cardiac arrest. In this group of patients, the symptoms should be addressed with appropriate treatment (naloxone for opioid overdoses and benzodiazepines and cooling for sympathomimetic drugs) and the surgeon rapidly called for an urgent consultation. For any toxicity more severe than mild and reversible symptoms, an operative approach will be the safest treatment.10
What if my patient is a body stuffer?
If the drug packets are fragile and were rapidly ingested by the patient, the risk of a surgical complication is lower, but the risk of leakage and subsequent toxicity is much higher. Body stuffers therefore differ from packers in the investigations and treatment that is recommended, First, CT imaging is much less useful since both radiographic sensitivity and risk of surgical complications are lower. For the same reason, surgical teams should only be involved if there is a strong suspicion of surgical complications (obstruction, perforation, etc.). These patients should also be observed in the ED and may reasonably receive a dose of activated charcoal if compliant. Since the overall quantity of ingested drugs is lower than packers, this period of observation can be reduced to 6 hours for sympathomimetic xenobiotics.11 Whereas opioid toxicity may be “silent”, overnight monitoring may be reasonable for patients stuffing opioid agonists. Watch for any signs of toxicity and treat accordingly.12
And what if my patient had also hidden drugs in his rectum?
Body pushers represent a heterogenous group of patients. Most of them do not hide an important amount of drug using this specific method. Nonetheless, some absorption of the drug has been reported with vaginal packets. Diagnosis is usually clinical. Treatment consists of the removal of the packets with irrigation if possible, and observation in the ED to make sure that no sign of toxicity develops.11,13
In any of these cases, if the diagnosis is not clear or if the treatment pathway seems ambiguous, local poison centers can be of great help.
Case Followup:
The patient underwent whole-bowel irrigation with PEG-3350. After 3 hours of observation in the ED, the patient developed progressive tachycardia, hypertension, and increased psychomotor agitation. He started to seize and received 4 mg of IV lorazepam. With the diagnosis already made and now signs of severe toxicity, the general surgeon was consulted and brought the patient to the operating room.
Clinical Pearls:
- Be suspicious. Patients are sometimes reluctant to give complete information due to legal considerations.
- When suspecting body packing, stuffing, or pushing, look for signs of toxicity and abdominal complications.
- The best diagnostic tool is abdominal CT. X-ray can be used as a screening tool but is far from diagnostic. Urine drug screens are rarely
- Asymptomatic body packers should undergo whole bowel irrigation preceded by activated charcoal if they do not have any contraindication. They should be observed at least 24 hours and can be discharged once all their packets have been expelled.
- Patient presenting with gastrointestinal obstruction or perforation should undergo
- Imaging is less useful for body stuffers, which can be observed in the ED. The duration of observation depends on what type of drugs they ingested.
- Patients with signs of drug toxicity are a true emergency. We must provide appropriate treatment for the identified toxidrome, and packets must be removed surgically.
- Drug toxicity should be treated as for any intoxicated patients: Benzodiazepines and external cooling for sympathomimetic overdose, and naloxone and respiratory support for opioid toxicity.
References:
- Shahnazi, M., Sanei Taheri, M., & Pourghorban, R. (2011). Body packing and its radiologic manifestations: a review article. Iranian journal of radiology: a quarterly journal published by the Iranian Radiological Society, 8(4), 205–210. https://doi-org.acces.bibl.ulaval.ca/10.5812/iranjradiol.4757
- Traub, S. J., Hoffman, R. S., & Nelson, L. S. (2003). Body packing–the internal concealment of illicit drugs. The New England journal of medicine, 349(26), 2519–2526. https://doi-org.acces.bibl.ulaval.ca/10.1056/NEJMra022719
- Booker, R. J., Smith, J. E., & Rodger, M. P. (2009). Packers, pushers and stuffers–managing patients with concealed drugs in UK emergency departments: a clinical and medicolegal review. Emergency medicine journal: EMJ, 26(5), 316–320. https://doi-org.acces.bibl.ulaval.ca/10.1136/emj.2008.057695
- Heymann-Maier, L., Trueb, L., Schmidt, S., Carron, P. N., Hugli, O., Heymann, E., & Yersin, B. (2017). Emergency department management of body packers and body stuffers. Swiss medical weekly, 147, w14499. https://doi-org.acces.bibl.ulaval.ca/10.4414/smw.2017.14499
- Mandava, N., Chang, R. S., Wang, J. H., Bertocchi, M., Yrad, J., Allamaneni, S., Aboian, E., Lall, M. H., Mariano, R., & Richards, N. (2011). Establishment of a definitive protocol for the diagnosis and management of body packers (drug mules). Emergency medicine journal: EMJ, 28(2), 98–101. https://doi.org/10.1136/emj.2008.059717
- Cappelletti, S., Piacentino, D., Sani, G., Bottoni, E., Fiore, P. A., Aromatario, M., & Ciallella, C. (2016). Systematic review of the toxicological and radiological features of body packing. International journal of legal medicine, 130(3), 693–709. https://doi-org.acces.bibl.ulaval.ca/10.1007/s00414-015-1310-3
- Bulakci, M., & Cengel, F. (2016). The role of radiology in diagnosis and management of drug mules: an update with new challenges and new diagnostic tools. The British journal of radiology, 89(1060), 20150888. https://doi.org/10.1259/bjr.20150888
- Pinto, A., Reginelli, A., Pinto, F., Sica, G., Scaglione, M., Berger, F. H., Romano, L., & Brunese, L. (2014). Radiological and practical aspects of body packing. The British journal of radiology, 87(1036), 20130500. https://doi.org/10.1259/bjr.20130500
- Makosiej, F. J., Hoffman, R. S., Howland, M. A., & Goldfrank, L. R. (1993). An in vitro evaluation of cocaine hydrochloride adsorption by activated charcoal and desorption upon addition of polyethylene glycol electrolyte lavage solution. Journal of toxicology. Clinical toxicology, 31(3), 381–395. https://doi-org.acces.bibl.ulaval.ca/10.3109/15563659309000407
- Das, D., & Ali, B. (2003). Towards evidence-based emergency medicine: best BETs from the Manchester Royal Infirmary. Conservative management [correction of management] of asymptomatic cocaine body packers. Emergency medicine journal: EMJ, 20(2), 172–174. https://doi-org.acces.bibl.ulaval.ca/10.1136/emj.20.2.172
- Moreira, M., Buchanan, J., & Heard, K. (2011). Validation of a 6-hour observation period for cocaine body stuffers. The American journal of emergency medicine, 29(3), 299–303. https://doi.org/10.1016/j.ajem.2009.11.022
- Yamamoto, T., Malavasi, E., Archer, J. R., Dargan, P. I., & Wood, D. M. (2016). Management of body stuffers presenting to the emergency department. European journal of emergency medicine: official journal of the European Society for Emergency Medicine, 23(6), 425–429. https://doi-org.acces.bibl.ulaval.ca/10.1097/MEJ.0000000000000277
- Wankhade, V. K., & Chikhalkar, B. G. (2018). Body packing and intra-vaginal body pushing of cocaine: A case report. Legal medicine (Tokyo, Japan), 31, 10–13. https://doiorg.acces.bibl.ulaval.ca/10.1016/j.legalmed.2017.12.004









1 thought on “Body Packers, Stuffers, and Pushers: Time Bombs in Our EDs”
Pingback: Quiz 158, June 17th, 2022 – The FOAMed Quiz